Disease burden and productivity cost of chronic rhinosinusitis patients referred to a tertiary centre in Australia
Introduction
Chronic rhinosinusitis (CRS) is a common chronic inflammatory disease with its prevalence ranging from 4.9% to 10.9% (1-4). Its negative impact on patients’ quality of life has been well recognised (5). Studies have demonstrated that in some respects, CRS can have a greater impact on patients’ quality of life than other chronic disorders such as back pain, chronic heart failure, angina pectoris and chronic obstructive pulmonary disease (6,7). Patients in the working age group are especially predisposed to the impairment with loss of workplace productivity (1,8). This is due to the detrimental health effects of CRS, which include bodily pain (9), headache (10), nasal dysfunctions (10), poor sleep (11,12), fatigue (10) and acute infections (13).
Economic evaluations on chronic medical conditions have been shown to assist the healthcare providers in better estimation of the associated societal costs and the cost-effectiveness of treatments provided. For example, Asthma (14), migraine (15) and diabetes (16) are among the common chronic conditions that have optimised their management by defining their disease burden to society. On the other hand, there are no gold standards in cost-effective treatment for CRS, despite increased understandings in its diagnosis, pathophysiology and management options (17). This suggests the importance to quantify CRS-related costs, in order to determine the cost-effectiveness of treatments available.
The socio-economic burden of CRS has been investigated in recent years with its both direct and indirect costs estimated. Bhattacharyya (18), in 2007, estimated the annual direct cost of CRS in the United States (U.S.) to be $8.6 billion. Using the Medical Expenditure Panel Survey, Bhattacharyya (18) demonstrated this direct cost was predominantly attributed to medication use, physician office visits and emergency department presentations. Similarly, Chung et al. (19) showed CRS patients to have significantly higher healthcare costs than non-CRS patients, where CRS patients had increased expenditures in both ENT outpatient services and other healthcare services.
Equally important to the direct economic burden of CRS is its cost to patients, where studies have estimated the productivity cost of CRS, using different methodologies (6,8,20). We argue that while the productivity cost has been investigated in other developed countries, the results may not be applicable to Australia due to inherent differences in the healthcare system and the socioeconomic status between countries. At Royal Brisbane and Women’s Hospital (RBWH), the high volume of CRS referrals to the department of ENT offers an opportunity to assess the productivity cost of CRS that is tailored to the Australian population.
The primary objective of this study is to determine the productivity cost among patients suffering CRS in Australia. Secondarily, the study aims to describe the use of Sino-Nasal Outcome Test-22 (SNOT-22) in the Australian population. SNOT-22 is a widely accepted tool in assessing the degree of disease-specific quality of life impairment for patients with CRS. It is both validated and reliable in differentiating the disease-affected patients from the normal healthy population with higher scorings for worsening diseases (21).
Methods
Participants
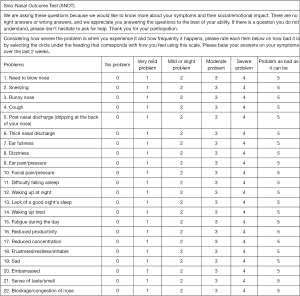
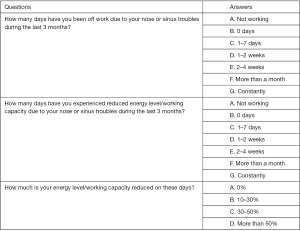
From January 2013 to January 2016, patients attending the rhinology clinic at RBWH were asked to complete clinical surveys as part of their assessments. The survey included questions on age, gender, and CRS-related outcomes, using SNOT-22 (Figure 1), and health economics questions (Figure 2) to describe CRS-related productivity loss. Participants were recruited from patients who were referred to the rhinology clinic for management and had CRS clinically diagnosed by our staff specialists. The data collection was limited to surveys completed during their first visits, in order to avoid any treatment effect. Exclusion criteria were applied to patients who reported to be not working or who did not complete the survey. No specific age restriction was applied to select the participants, based on the open definition of full-time adult employees by the Australian Bureau of Statistics as any employee paid at the full time adult rate for their occupation (22). This research was approved by the ethics committee at RBWH.
Measurement of productivity cost
The human capital approach was adopted to define CRS-related productivity cost. A series of formulas was applied to calculate the productivity cost, using lost productive time (LPT), presenteeism (PT), absenteeism (AT), and the latest average daily income for full-time adults in Queensland, Australia.
PT was defined as the reported work days affected by CRS with reduced work capacity, while AT was the reported number of work days missed due to CRS-related symptoms. In the preceding three months prior to clinic visits, participants were asked to report days affected or missed due to CRS using options of 0 days, 1–7 days, 1–2 weeks, 2–4 weeks, more than a month, and constantly. For days affected with reduced work capacity, participants were given levels of 0%, 10–30%, 30–50% and more than 50% to describe their perceived levels of work capacity reduction (WCR).
The average paid work time per participant was presumed to be full-time, which was defined as 8 hours per day, 5 days per week with 4 weeks of recreational leave per year. This gave a total of 240 expected work days per year. Therefore, 60 work days were estimated to be in the 3 months’ period that participants were asked to recall on the number of work days affected or missed due to CRS. For the purpose of calculating LPT, the reported work days affected or missed were translated to 0, 5, 10, 20, 30 and 60 days from the options of 0 days, 1–7 days, 1–2 weeks, 2–4 weeks, more than a month, and constantly, respectively. Similarly, perceived levels of WCR were translated to 0%, 25%, 50% and 75% from 0%, 10–30%, 30–50%, and more than 50%, respectively.
Annual AT was derived by multiplying the reported work days missed due to CRS or AT by four. Annual PT was then defined by applying the average percentage of reported WCR to the reported work days affected or PT and then multiplied by four. Thus CRS-related LPT or the number of days with productivity lost by CRS was the sum of both annual AT and annual PT, which was defined by the equation:
LPT = (AT ×4) + (PT ×4 × WCR)
Mean values of AT and PT from participants were calculated to produce mean LPT which was quantified as average days lost per CRS patient. The average weekly income in Australian Dollars (AUD) for full-time adults in Queensland was obtained from the Australian Bureau of Statistics (22), which was divided by 5 work days per week to give the average income per day. This was then used to monetise CRS-related LPT to estimate its productivity cost.
Secondary outcomes
Secondary outcomes included patients’ presenting age, gender and SNOT-22 scores. SNOT-22 score describes the severity of CRS among participants by asking them to describe their symptoms in twenty-two defined items (Figure 1). Additionally, these symptoms were categorised into separate domains, as DeConde and his colleagues have described (23). SNOT-22 was broken down into three sinus-specific symptom domains, based on rhinologic, extranasal rhinologic, and ear/facial symptoms; and two general health-related domains, which included psychological and sleep dysfunctions. The underlying domains to each item of SNOT-22 are summarized in Table 1. Descriptive analyses were applied to interpret the outcomes collected. The impact of age and SNOT-22 scores on the degree of productivity costs was assessed using Pearson’s correlation coefficient.
Table 1
| Domains | Survey items |
|---|---|
| Rhinologic symptoms | Q1, Q2, Q3, Q6, Q21, Q22 |
| Extranasal rhinologic symptoms | Q4, Q5, Q6 |
| Ear/facial symptoms | Q2, Q7, Q8, Q9, Q10 |
| Psychological dysfunction | Q14, Q15, Q16, Q17, Q18, Q19, Q20 |
| Sleep dysfunction | Q11, Q12, Q13, Q14, Q15 |
Results
A total of 448 completed surveys were obtained between January 2013 and January 2016, and 139 patients were excluded for not working for income. Among the 309 included participants, the average age of participants was 46.3 years old with a wide range of 14 to 73 years old. There were slightly more males (n=168; 54.4%) than females. Table 2 summarizes the results on the productivity cost and SNOT-22 outcomes.
Table 2
| Outcomes | Mean |
|---|---|
| PT | |
| Reported number of work days affected | 13.6 |
| Annual number of work days affected | 54.4 |
| WCR (%) | 21.5 |
| Annual PT LPT (days) | 11.7 |
| AT | |
| Reported number of work days missed | 6.4 |
| Annual number of work days missed or Annual AT LPT (days) | 25.6 |
| Productivity cost | |
| Total annual paid work LPT (days) (PT + AT) | 37.3 |
| Monetised daily work LPT (AUD) | $292.06 |
| Annual productivity cost (AUD) | $10,893.84 |
| SNOT-22 | |
| Total SNOT-22 score | 42.0 |
| Rhinologic symptoms | 12.5 |
| Extranasal rhinologic symptoms | 5.2 |
| Ear/facial symptoms | 7.5 |
| Psychological dysfunction | 13.6 |
| Sleep dysfunction | 11.8 |
WCR, work capacity reduction; LPT, lost productive time; SNOT-22, Sino-Nasal Outcome Test-22; AUD, Australian dollar; PT, presenteeism; AT, Absenteeism.
Annually, an average of 54.4 days was reported to be affected by CRS with mean daily reduction of 21.5% in work capacity. The mean annual PT and the mean annual AT were calculated to be 11.7 and 25.6 days, respectively. The mean overall annual LPT was estimated to be 37.3 work days lost per CRS patient.
According to the Australian Bureau of Statistics’ Average Weekly Earnings survey in May 2016, full-time employees in Queensland had an average weekly income of AUD $1,460.30 (22). Thus, an average daily income of AUD $292.06 was derived for each participant during monetisation of the mean annual LPT in this study. This estimated an overall annual productivity cost of AUD $10,893.84 per patient with CRS in Australia.
The mean SNOT-22 score was 42.0 with a range of 0 to 108. Specific domains demonstrated mean scores of 12.5 [0–28], 5.2 [0–15], 7.5 [0–23], 13.6 [0–35], 11.8 [0–25] for rhinologic symptoms, extranasal rhinologic symptoms, ear/facial symptoms, psychological dysfunction and sleep dysfunction, respectively.
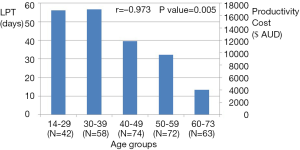
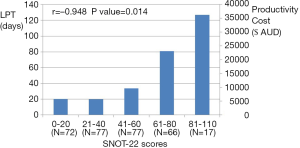
Significant correlations were found on the assessment of the degree of productivity costs to age and SNOT-22 scores. Figure 3 illustrated a significant correlation found between higher productivity costs and younger age groups (r=−0.973; P value =0.005). Patients younger than 40 years of age reported the highest LPT, while patients aged 60 years old or older had the lowest LPT. Secondly, SNOT-22 scores significantly correlated to the degree of productivity costs (r=0.948; P value =0.014). In a positive linear relationship (Figure 4), higher SNOT-22 scores or worse CRS symptoms lead to increased productivity costs.
Discussion
Productivity cost represents the societal perspective of disease burden and its economic loss to society. For efficient healthcare resource allocations, the goal of economic evaluations remains pivotal around understanding the social cost of diseases to adequately inform the policy makers before implementing appropriate health policies (24). Following the principle in the productivity cost study on refractory CRS by Rudmik et al. (8), this study examined the disease burden of CRS in the Australian community. The annual productivity cost was determined to be AUD $10,893.84 per patient from a cohort of 309 CRS patients referred to the rhinology clinic in an Australian tertiary hospital. Increasing productivity cost was found to significantly associate with worse SNOT-22 scores and younger patients with greater income potentials.
CRS and health economics
In Australia, studies have documented productivity costs for chronic pain and obesity. When adjusted for inflation, the annual costs of lost productivity due to chronic pain were AUD $6,780.25 and AUD $3,624.23 for males and females, respectively (25), while the annual indirect cost for obesity was AUD $701.06 per adult (26). In the U.S., the annual productivity costs were estimated to be $3,327.24, $5,869.59, and $7,670.59 for diabetes (16), chronic migraine (15), and severe asthma (14), respectively, after adjustment for inflation. Comparatively, our finding of CRS-related productivity cost is higher than the reported productivity costs of these common chronic conditions.
Acknowledging the differences in the average incomes between countries, the estimated annual LPT of 37.3 work days in this study is much lower than the reported 63.4 work days by Rudmik et al. (8), but their annual AT of 24.6 work days is comparable to our finding of 25.6 work days. In a large cohort of 47,725 sinusitis patients, Bhattacharyya (20) observed a much lower annual AT of 5.7 work days. The inconsistencies in these results are likely attributed to the differences in methodologies, where Bhattacharyya (20) relied on the inaccurate physician coding for sampling that may have included healthy subjects without CRS, leading to an underestimation of CRS-related disease burden. On the other hand, Rudmik et al. (8) have only included patients with refractory CRS, representing a group of patients with more severe CRS. This is reflected in the higher mean SNOT-22 score of 52.8 in their study to 42.0 in this study (8).
Another potential reason for the much higher annual LPT reported by Rudmik et al. (8) is their approach in including reduced work capacity as a daily impact for PT with an estimated annual PT of 38.8 work days. In comparison, we reported a much lower annual PT of 11.7 work days. This is because our survey has taken into account that patients with CRS can have some days better than others, and the participants were given the opportunity to describe how many days they have experienced reduced work capacity, rather than presuming that all CRS patients experience reduced work performance every day.
SNOT-22
SNOT-22 is a validated tool that is reliable and easily applicable with questions to quantitatively rate the severity of CRS. In previous studies using SNOT-22, patients with CRS were generally reported to have baseline total scores of 32.0 to 53.0 (27-30), while for non-CRS population, a mean SNOT-22 score of 11.3 was reported (31). Furthermore, recent researches have demonstrated increasing evidence that subscales of SNOT-22 can provide more clinically meaningful information on variations in patient severity and response to treatment than the one-dimensional interpretation of its total scores (32). For example, the domains of psychological and sleep dysfunctions were found to be significant predictors for elective endoscopic sinus surgery with sustained improvement in common sleep-related symptoms post-surgery (23,30).
Using SNOT-22, we demonstrated a mean baseline score of 42.0 from the 309 working patients who completed the health economics questions. There were no specific findings in the subscales of SNOT-22, with the scorings evenly spread among the five domains. While our SNOT-22 score provides some reassurance that our sample may resemble the CRS population in the community, SNOT-22 score is not a tool to diagnose CRS. Its interpretation is limited to describe the severity of sinonasal symptoms and health-related quality of life via patients’ self-reporting. Furthermore, higher scores of SNOT-22 have been shown to be influenced by asthma, depression and primary headache disorders (31,33).
Limitations
As with any retrospective study approach, there are selection biases in our recruitment of participants, which could potentially confound our results. The absence of questions on participants’ comorbidities, especially concurrent sinus pathologies, in the survey prevents consideration of variables that may contribute to the recorded LPT and SNOT-22 scores. Secondly, the exclusion of non-working patients limits our findings to Australian workers only. The impact of CRS reported in this study is biased against the part of Australian population from retirees, students and those taking a career break. Thirdly, recall bias can be a common issue for any study that relies on participants to recall past events, which presents as a potential risk for loss in precision during the quantification of AT and PT. However this risk should be minimized, as our survey was structured to follow the current recommendation on recall periods of 3 months (34). The answers for multiple-choice health economics questions were also provided in ranges to assist patients in easy identification of the answers that best suit them.
Secondary to the difficulty in differentiating the individual work hours of participants, the presumption of participants as full-time workers was taken with the use of human capital approach in valuing productivity loss. This raises concerns for overestimation in LPT, since some participants will be part-time workers and, unlike friction cost method, human capital method does not take the employer’s perspective into consideration, where productivity falls only for the time period until another employee takes over the patient’s work and production loss is minimized (34). Due to this potential overestimation, the productivity cost found in this study may have limited application in answering the economic burden of CRS to society, while the estimation of income loss to patients remains accurate. Although there are limitations, this research is the first to describe the CRS-related productivity cost in Australia, providing insight to its financial burden to the patients in addition to its impact on the quality of life.
Conclusions
The detrimental effects of CRS on health-related quality of life can cause substantial loss of income to its patients due to reduced work capacity and work absences. Health economics questions appear to be a simple adjunct to SNOT-22 that can assist clinicians in assessing the economic burden of CRS to their patients. The high productivity cost for CRS estimated in this study provides a strong incentive to develop a cost-effective management model to recognise and treat CRS early.
Acknowledgments
We thank all the staff at RBWH ENT outpatient clinic, especially the nursing staffs for their support in assisting patients to complete the surveys. We also thank Debbie Broughton, principal data analyst, at Patient Safety and Quality Improvement Service, Clinical Excellence Division, Department of Health, Queensland Government, for her involvement in the establishment of database framework.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.01.03). AC serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Waiver for patient informed consent was considered justified with National Statement 2.3.10 and approved by Human Research Ethics Committee, Royal Brisbane & Women’s Hospital. Ref No: HREC/16/QRBW/315.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bhattacharyya N. Functional limitations and workdays lost associated with chronic rhinosinusitis and allergic rhinitis. Am J Rhinol Allergy 2012;26:120-2. [Crossref] [PubMed]
- Cho YS, Choi SH, Park KH, et al. Prevalence of otolaryngologic diseases in South Korea: data from the Korea national health and nutrition examination survey 2008. Clin Exp Otorhinolaryngol 2010;3:183-93. [Crossref] [PubMed]
- Pilan RR, Pinna FR, Bezerra TF, et al. Prevalence of chronic rhinosinusitis in Sao Paulo. Rhinology 2012;50:129-38. [PubMed]
- Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe--an underestimated disease. A GA(2)LEN study. Allergy 2011;66:1216-23. [Crossref] [PubMed]
- Rudmik L, Smith TL. Quality of Life in Patients with Chronic Rhinosinusitis. Curr Allergy Asthma Rep 2011;11:247-52. [Crossref] [PubMed]
- Sahlstrand-Johnson P, Ohlsson B, von Buchwald C, et al. A multi-centre study on quality of life and absenteeism in patients with CRS referred for endoscopic surgery. Rhinology 2011;49:420-8. [PubMed]
- Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinology 2012;50:1-12. [PubMed]
- Rudmik L, Smith TL, Schlosser RJ, et al. Productivity costs in patients with refractory chronic rhinosinusitis. Laryngoscope 2014;124:2007-12. [Crossref] [PubMed]
- Chester AC, Sindwani R, Smith TL, et al. Systematic review of change in bodily pain after sinus surgery. Otolaryngol Head Neck Surg 2008;139:759-65. [Crossref] [PubMed]
- Soler ZM, Mace J, Smith TL. Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol 2008;22:297. [Crossref] [PubMed]
- Alt JA, Smith TL. Chronic rhinosinusitis and sleep: a contemporary review. Int Forum Allergy Rhinol 2013;3:941-9. [Crossref] [PubMed]
- Alt JA, Smith TL, Mace JC, et al. Sleep quality and disease severity in patients with chronic rhinosinusitis. Laryngoscope 2013;123:2364-70. [PubMed]
- Rank MA. Acute exacerbations of chronic rhinosinusitis occur in a distinct seasonal pattern. J Allergy Clin Immunol 2010;126:168-9. [Crossref] [PubMed]
- Cisternas MG, Blanc PD, Yen IH, et al. A comprehensive study of the direct and indirect costs of adult asthma. J Allergy Clin Immunol 2003;111:1212-8. [Crossref] [PubMed]
- Serrano D, Manack AN, Reed ML, et al. Cost and predictors of lost productive time in chronic migraine and episodic migraine: Results from the American Migraine Prevalence and Prevention (AMPP) Study. Value Health 2013;16:31-8. [Crossref] [PubMed]
- American Diabetes A. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033-46. [Crossref] [PubMed]
- Bernic A, Dessouky O, Philpott C, et al. Cost-Effective Surgical Intervention in Chronic Rhinosinusitis. Curr Otorhinolaryngol Rep 2015;3:117-23. [Crossref]
- Bhattacharyya N. Incremental Health Care Utilization and Expenditures for Chronic Rhinosinusitis in the United States. Ann Otol Rhinol Laryngol 2011;120:423-7. [Crossref] [PubMed]
- Chung SD, Hung SH, Lin HC, et al. Health care service utilization among patients with chronic rhinosinusitis: A population-based study. Laryngoscope 2014;124:1285-9. [Crossref] [PubMed]
- Bhattacharyya N. Contemporary assessment of the disease burden of sinusitis. Am J Rhinol Allergy 2009;23:392-5. [PubMed]
- Morley AD, Sharp HR. A review of sinonasal outcome scoring systems - which is best? Clin Otolaryngol 2006;31:103-9. [Crossref] [PubMed]
- Australian Bureau of Statistics. Average Weekly Earnings, Australia, May 2016. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/6302.0Main+Features1May%202016?OpenDocument
- DeConde AS, Mace JC, Bodner T, et al. SNOT-22 quality of life domains differentially predict treatment modality selection in chronic rhinosinusitis. Int Forum Allergy Rhinol 2014;4:972-9. [Crossref] [PubMed]
- Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. 4th edition. Oxford: Oxford University Press, 2015.
- van Leeuwen MT, Blyth FM, March LM, et al. Chronic pain and reduced work effectiveness: the hidden cost to Australian employers. Eur J Pain 2006;10:161-6. [Crossref] [PubMed]
- Yates J, Murphy C. A cost benefit analysis of weight management strategies. Asia Pac J Clin Nutr 2006;15:74-9. [PubMed]
- de Vilhena D, Duarte D, Lopes G. Sino-Nasal Outcome Test-22: translation, cultural adaptation and validation in Portugal. Clin Otolaryngol 2016;41:21-4. [Crossref] [PubMed]
- Abdalla S, Alreefy H, Hopkins C. Prevalence of sinonasal outcome test (SNOT-22) symptoms in patients undergoing surgery for chronic rhinosinusitis in the England and Wales National prospective audit. Clin Otolaryngol 2012;37:276-82. [Crossref] [PubMed]
- de Dorlodot C, Horoi M, Lefebvre P, et al. French adaptation and validation of the sino-nasal outcome test-22: a prospective cohort study on quality of life among 422 subjects. Clin Otolaryngol 2015;40:29-35. [Crossref] [PubMed]
- El Rassi E, Mace JC, Steele TO, et al. Improvements in sleep-related symptoms after endoscopic sinus surgery in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol 2016;6:414-22. [Crossref] [PubMed]
- Farhood Z, Schlosser RJ, Pearse ME, et al. Twenty-two-item Sino-Nasal Outcome Test in a control population: a cross-sectional study and systematic review. Int Forum Allergy Rhinol 2016;6:271-7. [Crossref] [PubMed]
- Browne JP, Hopkins C, Slack R, et al. The Sino-Nasal Outcome Test (SNOT): can we make it more clinically meaningful? Otolaryngol Head Neck Surg 2007;136:736-41. [Crossref] [PubMed]
- Lal D, Rounds AB, Rank MA, et al. Clinical and 22-item Sino-Nasal Outcome Test symptom patterns in primary headache disorder patients presenting to otolaryngologists with “sinus” headaches, pain or pressure. Int Forum Allergy Rhinol 2015;5:408-16. [Crossref] [PubMed]
- Zhang W, Bansback N, Anis AH. Measuring and valuing productivity loss due to poor health: A critical review. Soc Sci Med 2011;72:185-92. [Crossref] [PubMed]
Cite this article as: Liu T, Cooper T, Earnshaw J, Cervin A. Disease burden and productivity cost of chronic rhinosinusitis patients referred to a tertiary centre in Australia. Aust J Otolaryngol 2018;1:5.