A 5-year review of aural foreign body removal in a Major Victorian Hospital
Introduction
Aural foreign body (FB) is not an uncommon presentation to the emergency department (ED). Aural FB in the external auditory canal (EAC) of the ear, although unlikely to be life-threatening, may result in significant morbidity to the patient due to the discomfort, pain and other symptoms associated with this condition. The EAC is innervated by the vagus nerve (nerve of Arnold), the auricular-temporal branch of the mandibular nerve and by a small branch from the facial nerve; it is this richness of innervation which explains the sensitivity of the EAC and severe pain these patients may experience (1,2). We analysed the medical records of all patients who presented with an aural FB in the EAC to the ED of Frankston Hospital, a major Victorian Hospital in the Mornington Peninsula between 2012 and 2016.
Material and methods
This is a retrospective review (January 2012 to December 2016 inclusive) of patients that presented with aural FB to a single institution; Frankston Hospital ED. This study was approved by the Human Research Committee of Peninsula Health (reference number: QA/17/PH/10). A list of patients who presented with an aural FB to the ED department was derived from the Frankston Hospital medical records. Some were walk-in patients, while others were referred by their general practitioner (GP). The information obtained from medical records included: age at presentation, gender, side of presentation, type of FB found, presenting symptoms such as otalgia, ear discomfort, hearing loss, buzzing sound, crawling sensation, ear discharge, bleeding, others or no symptom. The type of aural FB was categorised as one of the following: no FB, insect, cotton tip, bead, part of ear phone/hearing aid, food/fruits, part of an ear plug or putty, a stone or pebble, bit of plastic, paper or rubber or a Styrofoam ball, a part of an ear ring, or toys and or playdough. Any other materials that appeared just the once and did not fit the aforementioned criteria were classed as either others (organic) or others (inorganic).
In addition, the length of time the FB was reported to have been lodged in the ear (in days), number of attempts at removal, methods of removal and the medical personnel involved in removal of FB. The latter group was categorised as GP; ED nurse practitioner/intern, registrar or consultant; ear, nose and throat (ENT) resident, registrar or consultant and unknown (when the name and job description were not written clearly in patient’s notes). GPs were included as some patients had one or two attempts by their GPs prior to presenting to the ED. The method of extraction included a group “others/not documented” in which the records did not document the method of extraction or the hand-written medical notes were illegible. The locations where removal of FB was successfully accomplished were categorised into: ED without sedation, ED with sedation or operating theatre under general anaesthesia (GA). Complications following removal of FB were categorised as canal abrasion, bleeding, tympanic membrane perforation and inflamed tympanic membrane. However, the records did not consistently show which attempt and therefore which technique was associated with a complication. The records and therefore results show which technique was used for the successful extraction of the aural FB.
The data generated was entered into a spreadsheet (Excel v14, Microsoft Office Professional Office), which was then imported into STATA v15 (StataCorp LLC, Texas, USA). The data was examined to determine if it was normally distributed using the Shapiro-Wilk test for normal data. Rejection of the Shapiro-Wilk null hypothesis (P<0.05) meant that data was not normally distributed, and therefore non-parametric tests were used and data describing a population was reported as median and range (min, max). The majority of variables were categorical and thus reported as numbers (percentages). These were tested using Fisher’s exact test. The extraction methods, number of aural FB extraction attempts and location of aural FB extraction were also examined using ordered logistic regression in STATA to see if they predicted “whether or not there was a complication following extraction of aural FBs”.
Statistical significance for a test required P<0.05. Results were graphed using Sigmaplot v13 (Systat Software Inc, California, USA).
Results
Presentation
Between 2012 and 2016 inclusive, 477 patients presented to Frankston Hospital ED with aural FBs. Ninety-seven of these patients were found not to have an aural FB on examination and were excluded. In the study population (n=380), there were 201 (53%) male and 178 (47%) female patients.
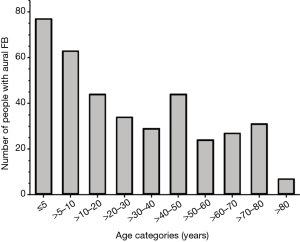
The median age of the remaining population (n=380) was 21 with a minimum and maximum range of 1 and 85. To further analyse the incidence of aural FB across different ages, the population was stratified into age groups as demonstrated in Figure 1. The data was categorised as one of the following: 0–5, >5–10 and then 10-year intervals up to 80 with a final >80 age group (Figure 1). Using this categorisation, the largest proportion of patients who presented with an aural FB was in the 5 year and under category (20%). However, 49% of patients were aged between 0 and 20 years and therefore 51% of patients who presented with an aural FB was an adult (>20 and over). This demonstrates an almost equal proportion between the paediatric and adult age groups.
In addition, the median age of the excluded population was not statistically significantly different from the study population {n, median [min, max], excluded: 97, 26 [0, 76] vs. included: 380, 21 [1, 85], P=0.61, by Mann-Whitney Rank Sum test}.
Two hundred and one (53%) patients had FB identified in the left ear and the remaining 179 (47%) in the right ear. This demonstrates a relatively equal distribution between the sides of ear affected. However, there was a statistically significant difference in the percentage of aural FB presented in the left vs. the right EAC, when comparing those aged 14 and below and those greater than 14. In the 14 years old and under group, 76 (39%) had FB in the left ear and 121 (62%) in the right, compared to those greater than 14 group where 158 (56%) had FB in the left ear and 122 (44%) in the right (Fisher’s exact test, P=0.000). The proportions of FB located in either side of the ear in our 14 years old and under group were quite similar to those described in the study by Peridis et al. (3), where 32% and 68% of objects were removed from left and right ears respectively.
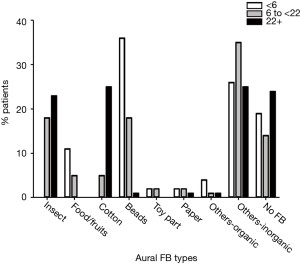
Types and frequencies of aural FBs found in this study are shown in Table 1. The proportion of patients found with each type of aural FB was significantly related to the following age groups: 0–5, 6–21 and 22–85 years of age (Figure 2, χ2=187.1, degrees of freedom =16, P=0.000 by Fisher’s exact test). The majority of the variety of aural FB types seen in this population was observed in these three age groups. The most common aural FB types found in the entire study population were insects (16.1%), followed by cotton (14.3%) and beads (13.6%, Table 1).
Table 1
| Types of foreign body | Number | Percentage (%) |
|---|---|---|
| No foreign body | 97 | 20.3 |
| Insects | 77 | 16.1 |
| Cotton tips | 68 | 14.3 |
| Beads | 65 | 13.6 |
| Part of ear phone/hearing aid | 45 | 9.4 |
| Others (inorganic) | 25 | 5.2 |
| Food/fruits | 18 | 3.8 |
| Part of ear plugs/putty | 17 | 3.6 |
| Stone/pebble | 12 | 2.5 |
| Others (organic) | 9 | 1.9 |
| Plastic bits | 9 | 1.9 |
| Paper bits | 7 | 1.5 |
| Rubber bits | 6 | 1.3 |
| Styrofoam ball | 6 | 1.3 |
| Part of ear rings | 6 | 1.3 |
| Part of toys | 5 | 1.0 |
| Playdough | 5 | 1.0 |
| Total | 477 | 100.0 |
The largest proportions of insects and cotton FB were identified in those aged 22 and above (23% and 25% respectively, Figure 2). Interestingly, insects and cotton were not found in patients aged 5 years and below (0% and 0% respectively, Figure 2). Most bead aural FB were identified in the 0–5 years old age group (36%, Figure 2), compared to those aged 22 years and above (1%, Figure 1). These demonstrate that the type of aural FB found is most likely to be influenced by the age of the patient.
In this study, patients with FB in the ear presented with a range of symptoms as shown in Table 2. The most common presenting symptom was otalgia (14%). However, it is worth noting that 64% of the study population were asymptomatic at the time of examination in the ED at Frankston Hospital.
Table 2
| Types of symptom | Number | Percentage (%) |
|---|---|---|
| No symptom | 243 | 63.9 |
| Otalgia | 52 | 13.7 |
| Discomfort | 27 | 7.1 |
| Hearing loss | 25 | 6.6 |
| Buzzing sound | 16 | 4.2 |
| Crawling sensation | 7 | 1.8 |
| Discharge | 3 | 0.8 |
| Bleeding | 1 | 0.3 |
| Others | 6 | 1.6 |
| Total | 380 | 100.0 |
There was a significant relationship between the frequency of presenting symptoms and the age of the patient when categorised into three different age groups (0 to ≤5, 6 to ≤21 and 22+ years of age), χ2=31.66, degrees of freedom =14, P=0.004 by Fisher’s Exact test). Otalgia was more frequently reported in the “6 to ≤21” age group, at approximately 3 times the percentage compared to the “5 years and under” group (23% vs. 8% respectively). Those patients aged 5 years and under were described more frequently as asymptomatic (80%) compared to the “6 to ≤21” and “22+” age groups (54% and 62% respectively).
Two hundred and sixty-one (68.7%) patients reported having their FB retained in the ear for less than a day. For the rest, 20 (5.3%) had their FB in their ear for 1 to 3 days, 25 (6.6%) for 3 to 7 days and 11 (2.9%) for 1 to 4 weeks. The remaining 4 (1%) patients reported having the aural FB in their ear for more than 4 weeks. In these cases, they were asymptomatic and all the aural FBs were identified as part of the patients’ hearing aids, hence explaining the longer duration of the FB. Finally, 59 (16%) cases had unknown durations as patients were either ensure of the duration of FB in their ear or the duration had not been documented in their medical records.
Extraction
Methods used to successfully extract the FB are shown in Table 3, with the most common method employed being the forceps (crocodile/alligator forceps) in 123 (32.4%) patients. One hundred and eleven (29.2%) patients had their FB removed by a method of removal which was not documented, and these cases were termed “other methods”.
Table 3
| Methods | Number | Percentage (%) |
|---|---|---|
| Forceps | 123 | 32.4 |
| Micro-suction | 64 | 16.8 |
| Metallic L-shaped hook | 36 | 9.5 |
| Curette | 21 | 5.5 |
| Syringing | 25 | 6.6 |
| Others/not documented | 111 | 29.2 |
| Total | 380 | 100.0 |
FB, foreign body.
Of the 380 patients with an aural FB, 278 (73.2%) had the FB removed successfully in the ED on the first attempt (Table 4). However, there were 21 (5.5%) and 14 (3.7%) patients which required 3 or 4 attempts respectively. Table 4 shows the number of attempts it took to successfully remove the aural FB in all cases. Although rare, there were four cases that required 6 or 7 attempts [3 (0.8%) and 1 (0.3%) respectively]. The distribution of age (in years) data failed the Shapiro-Wilk test for normality (P=0.0000), therefore the median (min, max) of age for each attempt number category (Table 4) has been used for further analysis using the Kruskal-Wallis equality of population rank test. This found a significant difference in the median age for the different number of attempts (χ2=13.6, degrees of freedom =6 and P=0.035). In general, a lower median age was associated with more attempts needed to successfully remove the aural FB.
Table 4
| Attempts | Number of patients | Percentage (%) | Median age [min, max] (years) |
|---|---|---|---|
| 1 | 278 | 73.2 | 25.5 [1, 85] |
| 2 | 54 | 14.2 | 14 [1, 80] |
| 3 | 21 | 5.5 | 6 [2, 81] |
| 4 | 14 | 3.7 | 7.5 [4, 73] |
| 5 | 9 | 2.4 | 11 [3, 32] |
| 6 | 3 | 0.8 | 13 [3, 13] |
| 7 | 1 | 0.3 | 11 [11, 11] |
| Total | 380 | 100.0 | – |
FB, foreign body.
A list of medical personnel who attempted extraction is shown in Table 5, with “ED registrar” as the most frequent group with attempts at aural FB removal. Two-thirds of all attempts to remove the aural FB were performed by the ED or ENT registrar (Table 5). The distribution of age data also failed the Shapiro-Wilk test for normality (P=0.0000), therefore the median (min, max) age data (Table 5) were investigated with respect to the different categories of medical personnel by the Kruskal-Wallis test. This found a statistically significant difference in the median age of patient treated by different categories of medical personnel (χ2=83.25, degrees of freedom =7 and P=0.0001). ED nurses or interns treated patients with an older median [min, max] age of 63.5 [50, 65] years, while ED consultants saw patients with a much younger median [min, max] age of 4.5 [1, 19] years. The remainder of the personnel saw patients of differing median age but with fairly wide age ranges.
Table 5
| Types of medical personnel | Number | Percentage (%) | Median age [min, max] (years) |
|---|---|---|---|
| General practitioner | 45 | 9.1 | 8 [1, 81] |
| ED nurse practitioner/intern | 52 | 10.5 | 43.5 [3, 85] |
| ED registrar | 211 | 42.6 | 28 [1, 81] |
| ED consultant | 36 | 7.3 | 12.5 [1, 81] |
| ENT resident | 10 | 2.0 | 21 [4, 73] |
| ENT registrar | 118 | 23.8 | 7 [1, 84] |
| ENT consultant | 22 | 4.4 | 4.5 [2, 19] |
| Unknown | 1 | 0.2 | 11 [11, 11] |
| Total | 495 | 100.0 | – |
FB, foreign body; ED, Emergency Department; ENT, ear, nose and throat.
Aural FBs were successfully removed in ED without sedation for 309 (81.3%) patients, while 20 (5.3%) had their FB removed in ED with sedation (nitrous oxide) and remaining 51 (13.4%) under GA in the operating theatre. These proportions were not statistically significantly different with respect to each extraction location (by Fisher’s exact test, χ2=0.23, P=1.00). Examination of the median age of patients according to where they had their aural FB extracted (see Table 6) found a statistically significant association (by Kruskal-Wallis test, χ2=81, P=0.0001). In general, removal of their aural FB in the ED with no sedation had a population with an older median age of 30. Extraction in ED with sedation or in Theatre under GA had median ages of 4 and 5 respectively, but the minimum and maximum age ranges were much narrower in the latter compared to the former (Table 6).
Table 6
| Location of extraction | Number | Percentage (%) | Median age [min, max] (years) |
|---|---|---|---|
| ED without sedation | 309 | 81.3 | 30 [1, 85] |
| ED with sedation | 20 | 5.3 | 4 [1, 65] |
| Theatre with general anaesthesia | 51 | 13.4 | 5 [2, 19] |
| Total | 380 | 100.0 | – |
FB, foreign body; ED, Emergency Department.
Only 40 (10.5%) patients, of 380 patients, were found to have complications following aural FB removal. Complications included canal abrasion (n=33, 8.7%), bleeding from the ear (n=6, 1.6%), inflamed tympanic membrane (n=1, 0.3%) and TM perforation (n=1, 0.3%).
Ordered Logistic Regression analysis was conducted to determine if: (I) extraction methods; (II) number of aural FB extraction attempts and (III) location of aural FB extraction significantly predicted whether there was a complication or not following extraction of aural FBs. Of all the methods examined, only extracting aural FBs using an L-shaped hook significantly predicted having a post-extraction complication, with an odds ratio of 1.66 (95% CI, 1.3–2.11, P=0.000). All other methods of extraction had no statistically significant effect on the probability of a post-extraction complication (all P>0.05). Increasing the number of attempts statistically significantly predicted increased complications post-extraction, with 3 attempts having an odds ratio of 3.4 (95% CI, 1.03–11.16, P=0.044), 4 attempts having an odds ratio of 4.8 (95% CI, 1.65–20.25, P=0.006) and 5 attempts having an odds ratio of 11.6 (95% CI, 2.85–46.8, P=0.001). The extraction location of the aural FB; i.e. whether extraction took place in the ED without sedation, ED with sedation or operating theatre under GA, did not significantly predict a post-operative complication (P=0.57).
Discussion
The majority of articles describing patients presenting with aural FBs are usually limited to the paediatric populations. In contrast, patients in this study ranged in age from neonates to the elderly, and just over half the presenting population was over 20 years of age (51%, Figure 1). This highlights the need to include older age groups in current literature to help optimise aural FB management.
Children tend to insert FB into their ears on purpose, whereas adults are more likely to accidentally retain FB in their ears. The reasons for children inserting FBs intentionally into their ears can range from irritation caused by otalgia and attraction to small, round or shiny objects to simple reasons such as curiosity or for fun (2). As for adults, the habit of using cotton tips to clean the ear or use of aural devices inserted into the EAC such as hearing aids, ear phones, ear plugs or ear putty may result in these objects being left in the ear canal by accident.
It is worth noting that a substantial number (20%) of patients who presented to Frankston Hospital ED for treatment of suspected aural FB were not found to have an aural FB upon examination, and thus were excluded from this study. This could not be simply explained by stating that the population was too young for enabling effective communication of their complaints. It was earlier stated that the median ages were not statistically different between the included and excluded groups. Thus, the reason for exclusion of the group was unlikely to be due to children being too young to communicate their presenting complaints effectively. We suspect that carers for younger patients who are unable to vocalise their problem, are more keen to bring them to the ED, especially when they see a child pulling or rubbing their ears long enough for them to suspect a FB in their ears. In the case of adults, most of them present to ED almost immediately, with the assumption that a FB is stuck in their ears after discovering part of the objects they had inserted into their ears were missing.
The most common aural FB found in our study was “Insects”, which were removed from 77 (16.1%) patients. The Mornington Peninsula, within which Frankston Hospital is located, is a popular holiday destination with many camping sites, beaches and caravan parks. As a haven for outdoor activities, this translates to a higher incidence of insects seen amongst all aural FB seen here in our hospital. Yaroko and Irfan from Hospital Universiti Sains Malaysia also reported the most common FB found to be insects, although at a considerably higher percentage at 54% (4).
Overall in our study, FBs were presented almost as frequently in the right as in the left ear (47% vs. 53%, respectively). This ratio is similar to two other studies (2,5). When we divided the groups according to age, we found that the majority of children (61%) aged 14 and under had an aural FB removed from their right ear and the remainder from their left (39%). If we expected that right-handed individuals would tend to insert objects in their right ear; as the general population is thought to consist of right to left handers in a ratio of 9:1, it would seem either left handers are more prone to lodging objects in their EAC or that handedness is not related to which ear an object is lodged (2,5). However, whether an object is lodged on the same side as the dominant hand may also depend on whether the object is placed deliberately in the ear. In our study, the handedness of each participant was not recorded, making it impossible to assess in this population whether handedness was associated with the side where the aural FB was found. We did however, find that two-thirds of the patients aged 14 years and under, presented with a FB inserted into their right ear, while FB in those over the age of 14 were almost equally distributed between the right and left ear. Likewise, in an earlier study, Peridis et al. found a significant relationship between handedness and the ear which contained the foreign object. More objects were inserted into the right ear by right-handed children (93%) compared to their left ear (7%) and more into their left ear by left-handed children (64%) than into their right ear (36%). The authors interpreted this relationship as being related not only to deliberate insertion of the object but also their relative ability to reach. However, this assumption ignores the fact that patients may have accidentally lodged a FB into the opposite ear using their non-dominant hand of which they have less fine control over.
The majority of patients, 243 (63.9%) with aural FBs were asymptomatic. This is likely due to the inert nature of most FBs and/or the short duration the FBs being retained in their ears. Those who were symptomatic reported otalgia as the most common symptom. Our study demonstrated a potential relationship between otalgia and age groups. Of those reporting otalgia, less than 14% were aged 5 years and less, while 45% and 41% were aged >5 to 20 and more than 20 years and older. This either suggests that patients aged 5 years and under have a higher pain threshold or that beads are the least painful type of aural FB for it is the most common type of aural FB removed from patients aged 5 years and under. Other symptoms such as ear discomfort, hearing loss, buzzing sound etc. each presented in less than 10% of the patient population.
There is no one particular method universally recognised as the best method for all aural FB removal. The method chosen to remove aural FBs should be based on several factors such as the location, shape, consistency and composition of the FB. Forceps (crocodile) are best used to remove soft, graspable objects such as cotton buds or sponges. Round, smooth objects like beads or hard objects like pebbles are best removed with an L-shaped hook. Soft, friable objects can be suctioned using micro-suckers and small non-hygroscopic objects can be syringed out with saline heated to body temperature.
Complications found post-extraction could be either due to existing irritation of FB to the ear canal and tympanic membrane or from attempted extraction by patients or medical personnel. Regression analysis showed that aural FBs extraction using an L-shaped hook significantly predicted having a complication following extraction. Although the ENT unit are the only ones using an L-shaped hook in our study, most aural FB that were referred to the ENT unit had multiple extraction attempts prior. Hence, it is likely that these repeated attempts will have already contributed to an increased risk of post-extraction complications.
As demonstrated in our study, a higher number of attempts significantly predicted having a complication post-extraction. This was likely because most aural FBs (except insects) are inserted or lodged in the outer cartilaginous portion of the ear canal. With each failed extraction, there is a cumulative risk of the FB being pushed deeper into the EAC, ending up either deep in the isthmus between the cartilaginous and bony portion of the EAC or in the deeper bony portion of the EAC right next to the ear drum. Given the confined space of the EAC, the further an aural FB is lodged, the more difficult the extraction is without causing damage to surrounding structures. Therefore, it is important to recognize that each unsuccessful attempt can significantly jeopardize the success of subsequent efforts. Repeated attempts not only lead to risk of injuring the EAC and bleeding, but can also compromise a patient’s cooperation (5), especially in children who have a variable level of cooperation (1).
In contrast, the location where the aural FBs were extracted; i.e., whether extraction took place in the ED without sedation, ED with sedation or operating theatre under GA, did not statistically significantly predict having a complication post-operatively. Hence it is obvious that majority of aural FB cases can be successfully managed in the ED without sedation, unless the FB was found to be too deep in the EAC. It is with initial failure due to inexperience or wrong method of removal, and multiple attempts that results in unnecessary escalation to use of adjuncts such as local sedation with nitrous oxide and subsequently GA. This inevitably wastes more time and resources. A simple procedure that carries little or no additional risk should always be attempted if it potentially avoids the use of GA (6).
According to the American Family Physician [with Strength of Recommendation Taxonomy (SORT) grade C], all aural FB cases should be referred to ENT specialty for removal except for those which are directly visible and graspable (7). Obviously, it would be impractical to mandate the referral of all aural FB cases to the ENT specialty. As observed in our study, other non-ENT medical personnel, especially those from the ED, are also well experienced in managing these patients. Therefore, it is highly recommended that aural FB removal should be performed by trained personnel, in order to avoid complications. However, if failure of the initial attempt is anticipated, particularly in the paediatric population, the best initial management is to obtain an ENT referral without any preliminary attempt. This will avoid potential physical trauma to the ear canal and more importantly, emotional trauma to the patient especially if they are children (6).
Just like performing any medical procedure, the key to successfully removing aural FBs is to have all necessary equipment prepared and ready. This includes an LED headlight, an appropriately sized aural speculum, the correct instruments for FB removal and a cooperative or well restrained patient. Occasionally, instilling a 4% lignocaine solution into the ear canal and waiting for 15 minutes for the anaesthetic to take effect can lessen the pain and make the patient more comfortable (8). Others have tried spraying the EAC with 10% Lignocaine to anaesthetise the ear. We do not use topical analgesic agents as although it provides some anaesthesia, it does not provide complete anaesthesia of the ear for safe removal of aural FB.
Conclusions
Some studies have reported percentages as high as 30% (9) and 53% (10) for removal of aural FBs under GA, while others have reported lower rates such as 12.2% (4) and 8.4% (2). Our rate of 14% for removal of aural FBs under GA suggests that there is room for improvement. Most aural FB removals, when done correctly the first time, have minimal complications and do not require GA. Our study demonstrated the importance of educating front line doctors such as GPs and ED physicians, that only experienced medical personnel, or juniors under the supervision of experienced personnel, should attempt removal of aural FBs. All failed first attempt thereafter should be referred to the ENT specialty without further attempts. With each additional attempt, the rate of complications increases. ENT opinion should be sought whenever there is doubt and the treating doctor must always remember, “First, do no harm” as attributed to Hippocrates.
Summary
- Children tend to insert FB into ear on purpose, whereas adults are more likely to accidentally retain FB in their ears;
- 63.9% of patients with aural FBs are asymptomatic;
- 81% of patients had their aural FBs successfully removed in ED without sedation;
- Increasing the number of attempts in removing aural FBs statistically significantly predicted having a complication post-extraction;
- Aural FB removal should be performed by trained personnel in order to avoid complications;
- All failed first attempts should be referred to the ENT specialty without further attempts as, with each additional attempt, the rate of complications increases.
Acknowledgments
We would like to thank Dr. Vicky Tobin and Frankston Hospital Librarians.
Funding: This study was not financially supported from any external sources and was fully funded by the Department of Surgery, Frankston Hospital.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.09.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Human Research Committee of Peninsula Health (reference number: QA/17/PH/10).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gregori D, Morra B, Berchialla P, et al. Foreign bodies in the ears causing complications and requiring hospitalization in children 0-14 age: results from the ESFBI study. Auris Nasus Larynx 2009;36:7-14. [Crossref] [PubMed]
- Chinski A, Foltran F, Gregori D, et al. Foreign bodies in the ears in children: the experience of the Buenos Aires pediatric ORL clinic. Turk J Pediatr 2011;53:425-9. [PubMed]
- Peridis S, Athanasopoulos I, Salamoura M, et al. Foreign bodies of the ear and nose in children and its correlation with right or left handed children. Int J Pediatr Otorhinolaryngol 2009;73:205-8. [Crossref] [PubMed]
- Yaroko A, Irfan M. An annual audit of the ear foreign bodies in hospital universiti sains malaysia. Malays Fam Physician 2012;7:2-5. [PubMed]
- Olajide TG, Ologe FE, Arigbede OO. Management of foreign bodies in the ear: a retrospective review of 123 cases in Nigeria. Ear Nose Throat J 2011;90:E16-9. [PubMed]
- Irfan M. Ear foreign body: tackling the uncommons. Med J Malaysia 2012;67:352. [PubMed]
- Heim SW, Maughan KL. Foreign bodies in the ear, nose, and throat. Am Fam Physician 2007;76:1185-9. [PubMed]
- Burton M, Gadre AK. Foreign body in the external auditory canal. Ear Nose Throat J 2009;88:988. [PubMed]
- Kadish H. Ear and nose foreign bodies: "It is all about the tools Clin Pediatr (Phila) 2005;44:665-70. [Crossref] [PubMed]
- Mackle T, Conlon B. Foreign bodies of the nose and ears in children. Should these be managed in the accident and emergency setting?. Int J Pediatr Otorhinolaryngol 2006;70:425-8. [Crossref] [PubMed]
Cite this article as: Ng TT, Lim JWJ. A 5-year review of aural foreign body removal in a Major Victorian Hospital. Aust J Otolaryngol 2018;1:25.