The modified endoscopic pre-lacrimal approach: how I do it
Introduction
The maxillary sinus is the sinus most commonly affected by disease. It is often described as being pyramidal in shape, with its base medially, forming the lateral nasal wall, and its apex lateral at the zygomatic process of the maxilla. It varies greatly in size, shape, position and pneumatisation, not only in different individuals, but also in different sides of the same individual (1). A broad spectrum of disease processes can involve the maxillary sinus, such as infective, odontogenic and neoplastic. In simple cases, a standard uncinectomy and middle meatal antrostomy may suffice for visualisation and clearance of disease. However, we too frequently come across scenarios where we can visualise extensive maxillary sinus disease but lack the ability to remove it. In such scenarios where a standard uncinectomy and middle meatal antrostomy do not suffice, there are few other options. Historically, the Caldwell-Luc approach was used for exactly such a scenario. However, due to the complex three-dimensional nature of the maxillary sinus, the Caldwell-Luc approach did not provide adequate access to certain regions of the maxillary sinus and had complications such as facial numbness due to infraorbital nerve injury, as well as numbness of the teeth and gums (2).
The pre-lacrimal recess is a concavity in the medial anterosuperior portion of the maxillary sinus. It is located anterior to the nasolacrimal duct, on the medial wall of the maxillary sinus (3).
The approach to the maxillary sinus via the pre-lacrimal recess was first described by Zhou et al. in 2007 (4), and again in 2013 (5) as an alternative approach to the maxillary sinus. It was again described in further detail by Morrisey et al. in 2016 (6). The original description of the approach involved making a curved mucosal incision on the lateral nasal wall just anterior to the head of the inferior turbinate. The nasal mucosa was then undermined off the lateral nasal wall. The maxillary sinus was entered with a chisel, and the medial bony wall of the maxillary sinus removed. This method provided excellent visualisation of all the regions of the maxillary sinus, whilst still maintaining the integrity of the nasolacrimal duct and inferior turbinate. The pre-lacrimal approach has also been extrapolated by other authors into an approach to the pterygopalatine fossa and infratemporal fossa. Others have used this approach to remove polyps and inverted papilloma arising from the maxillary sinus. We propose a modification of the technique described by Zhou et al., which is potentially quicker and results in the preservation of normal nasal anatomy.
Methods
A retrospective review of patients who underwent the modified pre-lacrimal approach between March 2016 and June 2018 was performed. Seven patients who underwent this approach were identified. All seven patients underwent a standard uncinectomy and middle meatal antrostomy, and if the pathology in the maxillary sinus was inaccessible, proceeded to have a modified pre-lacrimal approach performed during the same operation. Surgical complications and patient outcomes were evaluated (Table 1).
Table 1
| Patient | Sex | Age | Pathology | Complications | Outcome |
|---|---|---|---|---|---|
| 1 | F | 35 | Antrochoanal polyp | NIL | Disease free |
| 2 | F | 31 | Antrochoanal polyp | NIL | Disease free |
| 3 | M | 34 | Antrochoanal polyp | NIL | Disease free |
| 4 | F | 18 | Aspergilloma | NIL | Disease free |
| 5 | F | 69 | Suspected melanoma on the lateral wall of the maxillary sinus | NIL | Disease free |
| 6 | M | 47 | Aspergilloma | NIL | Disease free |
| 7 | F | 55 | Antrochoanal polyp | NIL | Disease free |
Objective
To assess the effectiveness and usefulness of the modified pre-lacrimal approach to the maxillary sinus.
Surgical technique
The nose is initially prepared with topical vasoconstrictor on neuropatties. An infiltration of 0.5% bupivacaine in 1;10,000 adrenaline is then applied to the lateral nasal wall, head of the inferior turbinate, inferior meatus and the floor of the nose.
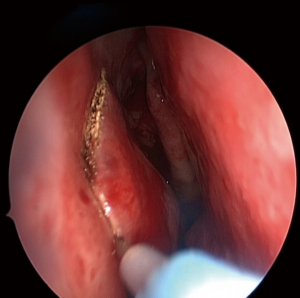
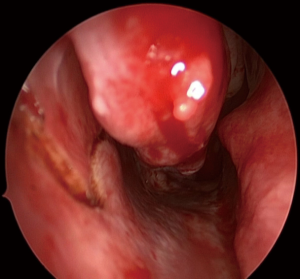
A standard uncinectomy and middle meatal antrostomy is performed, which facilitates a wide opening into the maxillary sinus. The next step requires an anterior C-shaped incision (Figures 1,2) that is made down to bone with monopolar diathermy, extending from the anterior border of the nasolacrimal duct, down between the nasal surface of the pyriform aperture and the head of the inferior turbinate, extending into the inferior meatus. Care is taken not to extend the incision lateral to the pyriform aperture of the nose as it passes anterior to the insertion of the inferior turbinate. Within the inferior meatus, an inferiorly based mucosal flap is created (Figure 3) and is reflected down. This is the same inferior meatus mucoperiosteal flap that the authors use for the endoscopic approach to the medial maxillectomy, but this flap will protect the inferior osteotomy.

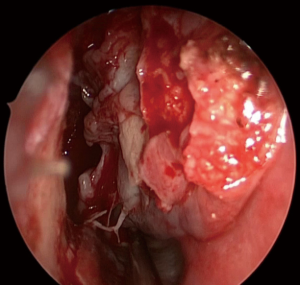
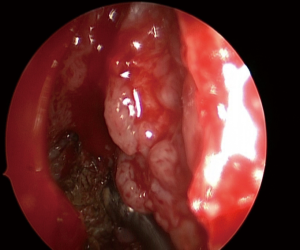
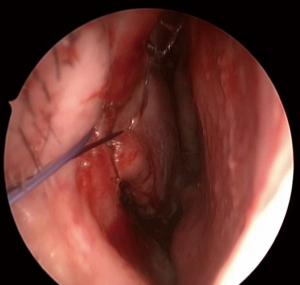
The mucosa of the anterior incision is then undermined off the lateral nasal wall and inferior meatus with a suction Freer elevator. Once the mucosa is freed enough for an osteotomy to be undertaken, a vertical bony cut is then made with a 4 mm osteotome through the lateral nasal wall, just deep to the pyriform aperture, into the maxillary sinus. The first osteotomy is usually anterior to the inferior turbinate through the pre-lacrimal recess, entering the maxillary sinus. The osteotome may be stabilised and guided into the maxillary sinus by first removing the anterior 1–2 mm of bone from the inferior turbinate where it inserts onto the lateral nasal wall. Further bony cuts are then made either preferentially with an osteotome, or with a 2.5 mm dacryocystorhinostomy cutting bur postero-superiorly along the lateral nasal wall to the nasolacrimal duct. After reflecting the mucosal flap in the inferior meatus, the osteotomy is then extended posteriorly along the inferior meatus to form the inferior cut. This results in a bone/mucosa flap pedicled on the nasolacrimal duct and the inferior turbinate posteriorly. This flap can be swung medially into the nasal cavity (Figures 4,5) to provide good access to the maxillary sinus, whilst preserving the nasal mucosa and entire inferior turbinate. Work can then be done in the maxillary sinus (Figure 6). A 30 or 70 degree scope can be used to assist visualization of all the regions of the maxillary sinus, but in most cases, the 0 degree endoscope affords adequate visualisation of the entire sinus. At the end of the procedure, the bone flap is replaced, mucosa overlaid and sutured with an absorbable 3/0 stitch (Figures 7,8). A small piece of absorbable packing is placed into the inferior meatus to control bleeding and assist healing. This modification preserves the entire bony medial wall of the maxillary sinus, in contrast with the existing description of the pre-lacrimal approach to the maxillary sinus, which sacrificed the entire bony medial wall of the maxillary sinus.


Results
The modified pre-lacrimal approach to the maxillary sinus was successful in treating all 7 patients. There were no incidents of nasolacrimal duct injury, facial or dental numbness during the follow-up period. We did not note any recurrences in patients who had antrochoanal polyps removed via this modified approach during the follow-up period. Post-operative epiphora occurred in only two patients but lasted less than four days in both.
Discussion
An uncinectomy and middle meatal antrostomy is the first step in accessing and treating pathologies of the maxillary sinus. However, due to the unique position and anatomy of the maxillary sinus, this may not suffice. Historically, alternative techniques such as the Caldwell-Luc approach, and the canine fossa approach were developed, to allow us to visualise all the surfaces of the maxillary sinus. These procedures, though simple and quick, are still open procedures, and inevitably lead to some degree of discomfort in the oral cavity. The modified pre-lacrimal approach eliminates the need for an incision or puncture in the oral cavity, and provides a wide and clear surgical view, with improved manoeuvrability for one instrument or more in the maxillary sinus. The improved surgical view also allows us to visualize and resect tumour in the maxillary sinus that may not have seen via the middle meatal antrostomy.
The pre-lacrimal recess is bounded by the pyriform aperture anteriorly, and the nasolacrimal duct posteriorly. Damage or fracture of the pyriform aperture may cause a cosmetic deformity, and injury to the nasolacrimal duct may lead to epiphora, which may require further surgery to correct. Other complications of the pre-lacrimal approach include nasal obstruction due to inferior turbinate destabilization, numbness of the teeth, persistent crusting and synechia. We believe that with our modified pre-lacrimal approach, we can minimize damage to the nasolacrimal duct as most of its bony covering is left intact, as well as decrease the incidence of nasal obstruction as the inferior turbinate is stabilized by the underlying bone.
In select patients, the distance between the pyriform aperture and nasolacrimal duct may be smaller than usual. In such patients, there is minimal space for an osteotomy and less working space overall. In these patients, the bone around the nasolacrimal duct can be removed to facilitate the anterior osteotomy. Alternatively, a formal endoscopic medial maxillectomy with dacryocystorhinostomy may be performed, especially in the presence of a neoplastic process.
In our study, 4/7 (57%) of patients underwent the modified pre-lacrimal approach for antrochoanal polyp. During a mean follow-up period of 9.4 months, no recurrence had developed. This concurs with the result from Comoglu et al. (10), who had similar results when using the conventional pre-lacrimal approach to excise antrochoanal polyps. The risk of recurrence of such polyps is likely greatly decreased via the pre-lacrimal approach, as optimal visualization and complete clearance are made simpler by greatly improved access to the maxillary sinus. We believe that this technique is best suited for patients with maxillary sinus pathology that does not require long term close observation, as such patients may be better served with a medial maxillectomy. As a result, in our study, neoplastic processes such as inverted papilloma or malignancies arising from the maxillary sinus were not treated with this technique. However, we note that the pre-lacrimal approach has been used by multiple other authors for the excision of inverted papilloma with good short-term results. Jurado-Ramos et al. (11) reported a recurrence rate of 11.8% (4/34) when utilizing the trans-nasal endoscopic medial maxillectomy technique for excising inverted papillomas of the maxillary sinus. Healy et al. (12) also performed trans-nasal endoscopic medial maxillectomy for the resection of inverted papillomas and noted a recurrence rate of 26.7% (8/30). In contrast, Zhou et al. (5) used a pre-lacrimal recess approach, and had a recurrence rate of 8.33% (1/12). Suzuki et al. (13) performed a similar approach and derived a recurrence rate of 1.96% (1/51). After evaluating these studies, it appears that the recurrence rate of the pre-lacrimal approach, when used to treat inverted papilloma, appears to be no higher than when a trans-nasal endoscopic medial maxillectomy is performed. This may be attributed to better disease clearance with straight-on visualization via the pre-lacrimal approach, compared to a trans-nasal endoscopic medial maxillectomy. With the medial maxillectomy, visualisation and manipulation of the tumour may require curved instruments and endoscopes, especially if the nasolacrimal system is preserved. However, at this time, we maintain that the pre-lacrimal approach may not be the most appropriate in treating inverted papillomas or malignancies of the maxillary sinus as surveillance is difficult. Further long-term studies will need to be performed to assess the feasibility of this approach to treat the above-mentioned conditions.
Conclusions
Our modified pre-lacrimal approach is a safe and simple modification of the existing techniques. We believe that it minimises manipulation of the nasolacrimal duct and thus epiphora, and also reduces the likelihood of inadvertent intra-nasal trauma. It also provides excellent visualisation of all surfaces in the maxillary sinus and has the added benefit of preserving normal lateral nasal wall bony anatomy, thus minimizing potential complications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.10.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Standring S, Borley NR, Collins P, et al. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 40th ed. New York, NY: Churchill Livingstone, 2008:547-60.
- Low WK. Complications of the Caldwell-Luc operation and how to avoid them. Aust N Z J Surg 1995;65:582-4. [Crossref] [PubMed]
- Hosemann W, Scotti O, Bentzien S. Evaluation of telescopes and forceps for endoscopic transnasal surgery on the maxillary sinus. Am J Rhinol 2003;17:311-6. [Crossref] [PubMed]
- Zhou B, Han DM, Cui SJ, et al. Endoscopic nasal lateral wall dissection approach to maxillary sinus. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2007;42:743-48. [PubMed]
- Zhou B, Han DM, Cui SJ, et al. Intranasal endoscopic prelacrimal recess approach to maxillary sinus. Chin Med J (Engl) 2013;126:1276-80. [PubMed]
- Morrissey DK, Wormald PJ, Psaltis AJ. Prelacrimal approach to the maxillary sinus. Int Forum Allergy Rhinol 2016;6:214-8. [Crossref] [PubMed]
- Koh LT, Dhepnorrarat RC. Mucosal and bony incisions. Asvide 2018;5:841. Available online: http://www.asvide.com/article/view/28179
- Koh LT, Dhepnorrarat RC. Accessing and treating pathology in the maxillary sinus. Asvide 2018;5:842. Available online: http://www.asvide.com/article/view/28180
- Koh LT, Dhepnorrarat RC. Suturing the inferior turbinate and packing the inferior meatus. Asvide 2018;5:843. Available online: http://www.asvide.com/article/view/28181
- Comoglu S, Celik M, Enver N, et al. Transnasal Prelacrimal Recess Approach for Recurrent Antrachoanal Polyp. J Craniofac Surg 2016;27:1025-7. [Crossref] [PubMed]
- Jurado-Ramos A, Jodas JG, Romero FR, et al. Endoscopic medial maxillectomy as a procedure of choice to treat inverted papillomas. Acta Otolaryngol 2009;129:1018-25. [Crossref] [PubMed]
- Healy DY Jr, Chhabra N, Metson R, et al. Surgical risk factors for recurrence of inverted papilloma. Laryngoscope 2016;126:796-801. [Crossref] [PubMed]
- Suzuki M, Nakamura Y, Yokota M, et al. Modified transnasal endoscopic medial maxillectomy through prelacrimal duct approach. Laryngoscope 2017;127:2205-9. [Crossref] [PubMed]
Cite this article as: Koh LT, Dhepnorrarat RC. The modified endoscopic pre-lacrimal approach: how I do it. Aust J Otolaryngol 2018;1:30.