The combined endoscopic radical antrostomy and buccal fat pad (BFP) approach is effective in managing oroantral fistulae
Introduction
Oroantral fistulae (OAFs) occur when an oro-antral communication between the oral cavity and maxillary sinus fails to close and a pathological epithelialized tract forms between the two cavities (1). While several causes of OAF exist, the vast majority (2) are caused by iatrogenic dental extraction of the posterior maxillary teeth, due to the close anatomical relationship between the apical roots of these teeth and the maxillary sinus floor.
OAFs, if left untreated, can be associated with significant morbidity as up to 90% of patients develop chronic bacterial sinusitis (3) over the following weeks. Other manifestations of OAF include nasal leaks, nasal dysphonia, dysphagia, halitosis, coryza, dysgeusia, unilateral nasal obstruction and facial pain.
While smaller fistulas may close spontaneously via secondary intention, larger fistulas almost ubiquitously require surgical closure (4-8). The buccal fat pad (BFP) approach, described initially in 1977 by Egyedi, continues to be a common surgical option in the management of OAF. The fat pad’s proximity to the surgical field, abundant blood supply and its ease in dissection have made the BFP an effective technique in closure of oral defects.
However, the infective maxillary sinusitis also needs to be addressed, both to provide symptomatic relief but also to reduce infective load and maximise the chances of flap survival and fistula closure. Functional endoscopic sinus surgery (FESS) is now established as the gold standard surgical intervention for maxillary sinus debridement from conventional intraoral approaches such as the Caldwell-Luc procedure. FESS confers several benefits (9) over traditional intraoral techniques, as it is a minimally invasive approach, preserves sinonasal mucosa and physiological mucociliary drainage, and facilitates in-office sinus surveillance.
The purpose of this paper is to describe a successful technique in using the combined antrostomy and BFP approach for the management of OAF, which combines an intra-oral repair with endonasal FESS of the affected maxillary sinus under a single anaesthetic through this review, the author’s report their outcomes in a case series of patients who underwent this procedure.
Methods
All consecutive patients who underwent a combined endoscopic radical antrostomy with BFP for OAF identified from operating theatre logbooks at Norwest Private Hospital, a private surgical hospital in Sydney, Australia were identified.
Indication for surgery was either recurrent maxillary sinusitis or immediately following recognition of oroantral communication after dental extraction. Recurrent sinusitis was odontogenic in origin arising from the molar teeth on the ipsilateral side. It was defined as patients with dental pain or peri-odontitis reporting symptoms of facial pain and pressure. The patients in the series needed to have a primary dental complaint and subsequent investigation including a CT scan demonstrating an ipsilateral opacified maxillary sinus. Surgery was performed as a combined case by both an oral maxillofacial surgeon (A Naim) and otolaryngology-head and neck surgeon (F Riffat) and all patients underwent a combined assessment preoperatively. Dental extractions were performed in every case and none of the patients were managed for a spontaneous or malignant fistula. We presume that the driving force behind these fistulae and sinusitis was the focus of apicitis and some of the patients had maxillary sinus mucosal thickening despite a patent ostiomeatal complex. Patients who had concurrent chronic rhinosinusitis and multiple sinus pathology were excluded as were patients with other dental issues such as sinus lifts, implants or previous OAF. No patients required turbinate surgery to facilitate access to the maxillary antrum. All of our cases in this series occurred in the molar teeth and no patients demonstrated a fistula occurring between teeth, although this could likely be closed with a similar approach.
Retrospective review of prospectively collected data of each patient’s hospital medical records was then performed. Baseline demographics collected included age at time of surgery, sex, presenting symptoms and the indication for surgery. Outcomes were reviewed based on records kept at the first post-operative follow-up at 6 weeks. Successful outcome was defined as closure of the OAF. The authors used the 6-week follow-up period as this is the standard time for assessment of regional flaps—and an assessment of mucosalisation with the native gingiva could be assessed. If this was achieved, the flap was determined to have healed.
It was hypothesized that antral decompression was less likely to cause flap ischaemia, infection or breakdown. The sinus decompression antrostomy was an ancillary procedure for patients with ipsilateral opacified maxillary sinuses in the presence of apicitis or an established fistula post-extraction.
Surgical technique
- The patient is prepared for oral surgery with a mouth gag and occlusive blocks, in a supine position with shoulder roll. The OAF defect is examined endo-orally in this position.
- The nose was decongested with topical atomized Moffatt’s solution (2 mL Cocaine 10%; 1 mL 1:1,000 adrenaline, 2 mL 8.4% sodium bicarbonate; and 5 mL of normal saline). The anterior nasal septum and inferior turbinates were injected with Lignospan Special (2.2 mL 2% Lidocaine Hydrochloride, 1 in 80,000 adrenaline tartrate) using a 25G hypodermic needle.
- A rigid endoscope is then passed through the nasal cavity on the affected side to assess for any concurrent sinonasal pathology.
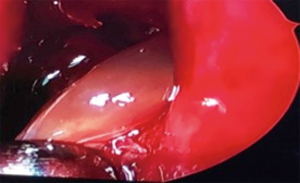
- A radical endonasal maxillary antrostomy is then performed with a 30-degree endoscope. The uncinate process is initially opened, then subsequently enlarged to include the fontanelles to the orbital floor, posterior antral wall and attachment of the inferior turbinate. Any debris encountered are cleared from the maxillary sinus, using curved scopes and instruments where necessary (Figure 1).
- A 70-degree endoscope was used for better view and if required a lacrimal probe could be used to visualize the fistula defect. Visualisation of the fistula was not usually necessary as the repair was per-orally with vascularized fresh tissue. In some cases, the 70-degree scope was used to remove dental fragments dislodged in the sinus.
- A circular incision is then made around the opening to the OAF. A trapezoidal mucoperiosteal flap is raised and everted.
- An incision is made in the buccal mucosa ipsilateral to the defect. Careful blunt dissection follows, until the yellow buccal fat tissue is encountered, an appropriate volume of buccal adipose tissue is then harvested to approximate the fistula defect.
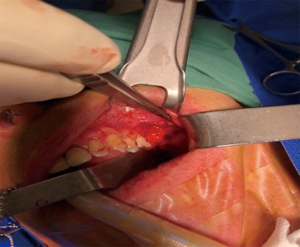
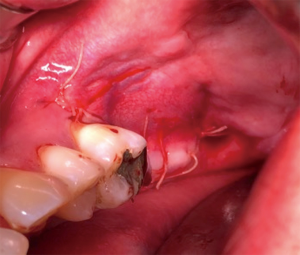
- The BFP is advanced to cover the fistula defect and secured to the palatal mucosa without tension (Figure 2). The mucoperiosteal flap is then returned to its initial position and secured with absorbable sutures (Figure 3).
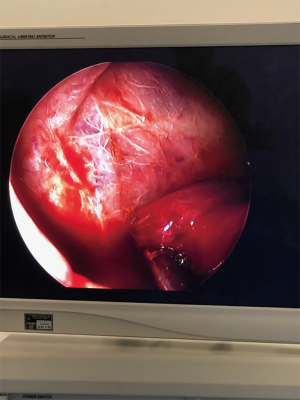
- The endoscope is then inserted back into the nose and the defect examined from above to ensure complete closure of the fistula (Figure 4).
Post-operative care
All patients were planned to stay overnight in hospital after their procedure. The nasal passage was packed with sinufoam in all patients. Patients underwent regular nasal saline douching three times a day for 6 weeks, a 2-week course of broad spectrum or culture-directed oral antibiotics, and advised to avoid nose blowing, straining, sneezing or any Valsalva-associated manoeuvre. Patients were also required to use chlorhexidine mouthwash 0.2% as an oral rinse for 1–2 weeks post-operatively. Patients had planned first follow-up at 6 weeks post-operatively.
Results
A total of 15 patients (age 50.1±10.3 years; 60% male) were included in the study. All patients were discharged the following day with no immediate surgical complications including epistaxis, facial paraesthesia or anosmia. All patients experienced successful closure of OAF. No fat pads experienced breakdown and no patients required further revision surgery.
All patients had an OAF defect and surgery was performed for either recurrent sinusitis in the context of dental impaction and apicitis or following recognition of the communication following dental extraction. All fistulas were related to molar dental extraction in our series. Indication for surgery was relatively equal between recurrent maxillary sinusitis (46.7%, n=7) and post-dental extraction (53.3%, n=8). This is summarised in Table 1. All patients exhibited symptoms including mucopurulent discharge, nasal congestion, pain and swelling prior to the procedure. All patients were assessed preoperatively and imaged radiographically. Patients who had concurrent chronic rhinosinusitis and multiple sinus pathology were excluded and surgery was not performed in a combined approach.
Table 1
| Patient | Age/sex | Indication | Closure of fistula |
|---|---|---|---|
| 1 | 56 M | Recurrent sinusitis | Y |
| 2 | 62 M | Post extraction fistula | Y |
| 3 | 43 M | Post extraction fistula | Y |
| 4 | 37 F | Post extraction fistula | Y |
| 5 | 66 F | Post extraction fistula | Y |
| 6 | 31 M | Recurrent maxillary sinusitis | Y |
| 7 | 45 M | Recurrent maxillary sinusitis | Y |
| 8 | 62 F | Post extraction fistula | Y |
| 9 | 51 F | Recurrent maxillary sinusitis | Y |
| 10 | 42 F | Recurrent maxillary sinusitis | Y |
| 11 | 47 F | Post extraction fistula | Y |
| 12 | 62 M | Post extraction fistula | Y |
| 13 | 54 M | Recurrent maxillary sinusitis | Y |
| 14 | 51 M | Post extraction fistula | Y |
| 15 | 43 M | Recurrent maxillary sinusitis | Y |
All patients reported a subjective improvement in their symptoms of facial pressure and pain at the time of the 6-week follow-up appointment. No patients presented to an emergency department post operatively and none complained of significant epistaxis, facial paraesthesia and anosmia. Of the 15 patients, none of the patients required a return to the operating theatre and postoperative pain was minimal, controlled with simple analgesia only.
Discussion
While many causes of oroantral communicating defects exist (8,9), such as osteomyelitis, dental infections radiation therapy, trauma, the majority of cases are secondary to iatrogenic injury following dental extraction. The most common site of communication is in the posterior maxillary teeth due to the proximity to the antrum and the thin antral floor which divides them (ranging from 1 to 7 mm). Oroantral defects can range in size (8) and clinical presentation. While small defects less than 2 mm can resolve without further surgical intervention, large defects more than 3 mm often persist and lead to chronic inflammation and maxillary sinusitis). Odontogenic causes (10) for maxillary sinusitis have been shown to be prevalent in both immunocompetent and immunosuppressed hosts, and risk factors for developing this complication following tooth extraction include performance of an incision (11), mesioangular tooth angulation, and type 3 RS classification (i.e., significant superimposition of the roots of all posterior maxillary teeth with the sinus floor).
The BFP is comprised of adipose tissue that is similar morphologically to orbital fat and distinct from subcutaneous fat (4). This specialised type of fatty tissue is called syssarcosis, and has a unique role in facilitating the gliding motion of the muscles of mastication. The BFP is a lobulated structure with a central body and four extensions—buccal, pterygoid, pterygopalatine and temporal. Each part of the BFP is encapsulated separately and is anchored to the surrounding structures by ligaments. There are a number of suspected physiological functions of the BFP, which include protection of neurovascular structures, improving movement between muscles and preventing negative pressure in newborns while sucking.
The BFP also has rich vascular supply, with multiple tributaries from the maxillary, superficial temporal arteries and the facial artery. The excellent blood supply, proximity to potential defects, epithelialization outcome and successful outcomes make it a treatment of choice for oral reconstruction procedures (4).
The BFP was first described (4,5) by Dr. Peter Egyedi in 1977 in a case series where the technique was successfully used in four patients who had large palatal defects. Since then, it’s applications have broadened and the technique has been adopted to manage other oral and maxillofacial pathologies and oral reconstruction techniques.
The BFP has also been well described as a viable surgical technique in the management of OAF. A paper by Poeschl et al. (5) demonstrated that in 161 patients with OAF, the BFP procedure was successful in all but 12 patients. Most of these unsuccessful cases were noted to have occurred in patients with concurrent infection at time of operation, history of tumour resection or in particularly complicated fistula defects. As a result, in these patients it appears that the BFP alone may be insufficient in ensuring fistula closure.
It is the author’s opinion that high intra-maxillary pressure and persistent intra-antral mucosal infection are the potential predisposing factors leading to failure of OAF closure. As a result, we suggest that combining a 3 layered (fat, mucoperiosteum and mucosa), well vascularised flap with extensive debridement of maxillary sinus infection maximises fistula closure rates and minimises fat pad breakdown and dehiscence.
The combined endoscopic radical antrostomy and BFP technique described in this paper combines a radical antrostomy with the BFP to manage the maxillary sinus congestion concurrently with fistula closure. There are multiple advantages to the technique that the authors have used in this study. Drainage of the maxillary sinus and reduced intra-antral pressure contributes to a concurrent reduction of flap dehiscence, local infection and ischaemia. The evacuation of the sinus and of purulent secretions reduce local infection and the inflamed maxillary sinus is allowed to heal via a natural mucociliary pathway. Furthermore, closure of the fistula defect is possible using only one anaesthetic and examination of the flap both superiorly and inferiorly can be performed intra-operatively and at all subsequent follow-up visits. In our case series, all patients experienced successful closure and symptom improvement with a negligible complication profile and a 0% revision rate.
Conclusions
The combined approach of FESS and BFP appears to be a safe and effective method for the management of patients with OAF in the context of tooth extraction or chronic maxillary sinusitis.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.11.01). FR serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Western Sydney Local Health District Human Research Ethics Committee (No. 5425/QA). Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khandelwal P, Hajira N. Management of Oro-antral Communication and Fistula: Various Surgical Options. World J Plast Surg 2017;6:3-8. [PubMed]
- Hassan O, Shoukry T, Raouf AA, et al. Combined palatal and buccal flaps in oroantral fistula repair. Egypt J Ear, Nose Throat Allied Sci 2012;13:77-81.
- Haas R, Watzak G, Baron M, et al. A preliminary study of monocortical bone grafts for oroantral fistula closure. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:263-6. [Crossref] [PubMed]
- Hassani A, Shahmirzadi S, Saadat S. Applications of the Buccal Fat Pad in Oral and Maxillofacial Surgery. Available online: https://www.intechopen.com/books/a-textbook-of-advanced-oral-and-maxillofacial-surgery-volume-3/applications-of-the-buccal-fat-pad-in-oral-and-maxillofacial-surgery
- Poeschl PW, Baumann A, Russmueller G, et al. Closure of oroantral communications with Bichat's buccal fat pad. J Oral Maxillofac Surg 2009;67:1460-6. [Crossref] [PubMed]
- Horowitz G, Koren I, Carmel NN, et al. One stage combined endoscopic and per-oral buccal fat pad approach for large oro-antral-fistula closure with secondary chronic maxillary sinusitis. Eur Arch Otorhinolaryngol 2016;273:905-9. [Crossref] [PubMed]
- Daif ET. Long-Term Effectiveness of the Pedicled Buccal Fat Pad in the Closure of a Large Oroantral Fistula. J Oral Maxillofac Surg 2016;74:1718-22. [Crossref] [PubMed]
- Yang S, Jee YJ, Ryu DM. Reconstruction of large oroantral defects using a pedicled buccal fat pad. Maxillofac Plast Reconstr Surg 2018;40:7. [Crossref] [PubMed]
- Penttilä MA, Rautiainen ME, Pukander JS, et al. Endoscopic versus Caldwell-Luc approach in chronic maxillary sinusitis: comparison of symptoms at one-year follow-up. Rhinology 1994;32:161-5. [PubMed]
- McCarty JL, David RM, Lensing SY, et al. Root Cause Analysis: An Examination of Odontogenic Origins of Acute Maxillary Sinusitis in Both Immunocompetent & Immunocompromised Patients. J Comput Assist Tomogr 2017;41:484-8. [Crossref] [PubMed]
- Hasegawa T, Tachibana A, Takeda D, et al. Risk factors associated with oroantral perforation during surgical removal of maxillary third molar teeth. Oral Maxillofac Surg 2016;20:369-75. [Crossref] [PubMed]
Cite this article as: Noussair M, Wong E, Naim A, Riffat F. The combined endoscopic radical antrostomy and buccal fat pad (BFP) approach is effective in managing oroantral fistulae. Aust J Otolaryngol 2018;1:32.