
Paediatric petrous temporal bone fractures: a 5-year experience at an Australian paediatric trauma centre
Introduction
The temporal bone forms part of the lateral skull base and is made up of the squamous, styloid, tympanic, mastoid and petrous segments (1). The petrous temporal bone (PTB) is one of the hardest bones in the body and therefore a significant amount of force must be applied to result in a fracture (2). The PTB contains essential anatomical structures including the facial nerve, internal carotid artery, the cochlea and vestibule, which are responsible for hearing and balance respectively (3).
A PTB fracture can result in significant immediate and long-term complications including facial nerve palsy (FNP), conductive and/or sensorineural hearing loss, cerebrospinal fluid (CSF) leak and related neurological injuries (4). Early childhood hearing loss has been clearly shown to result in poorer outcomes in a multitude of important developmental skills such as communication, language, cognition and motor skills (5-7). Facial expression plays an important role in conveying emotions, which is critical in the social development of children (8). A FNP can be extremely disfiguring and can result in severe stigmatization and social isolation, especially in the paediatric population (9). This in turn has been shown to increase the prevalence of anxiety and depression in those with a FNP (10). Complications associated with PTB fractures can have enormous functional, developmental and social implications in the paediatric population and therefore, appropriate and timely management is required to ensure optimal outcomes.
There are currently no studies that look exclusively at PTB fractures in an Australian paediatric population. The primary aim of this study was to investigate the prevalence of PTB fractures in children who presented with a traumatic skull fracture and the prevalence of associated otological and neurological complications. The secondary aim of this project was to provide general recommendations on the early management of paediatric PTB fractures based on regional data. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo.2020.03.05).
Methods
This retrospective cohort study was conducted at a tertiary referral paediatric trauma centre, The Royal Children’s Hospital (RCH), Melbourne. The RCH is the primary paediatric trauma centre in Victoria, Australia. This study included all paediatric patients admitted to the RCH over a 5-year period between January 2013 and December 2017 with a traumatic skull fracture. This study was approved by the Royal Children’s Hospital Ethics Committee as a low-risk project and the requirement for consent was waived.
Data was extracted from the Royal Children’s Hospital electronic medical records (EPIC) and pre-established trauma databases. Outcome measures included age, sex, mechanism of injury, type of PTB fracture, otological and neurological deficits, other associated injuries, and mortality.
The sequalae of petrous temporal fractures were specifically collected, and included presence of CSF leak, presence and grade of facial nerve injury, and presence, type and grade of hearing loss at time of 3-month follow-up. PTB fractures were classified using both the conventional ‘longitudinal vs. transverse’ system and the newer ‘otic capsule sparing vs. otic capsule violating’ system. FNP was graded in this study using the House Brackmann scale (HB). HB 2 was classified as mild, HB 3 or 4 as moderate, and HB 5 or 6 as severe FNP.
It is standard practice at our institution that all PTB fractures are reviewed on admission, treated accordingly and then followed up with an audiogram and by the Otolaryngology, Head and Neck unit at 3 months. Severity of conductive or sensorineural hearing loss was classified as normal (audiometry ISO ≤20 dB), mild (audiometry ISO 21-40dB), moderate (audiometry ISO 40–70 dB), severe (audiometry ISO 70–90 dB), and profound (audiometry ISO ≥90 dB).
Results
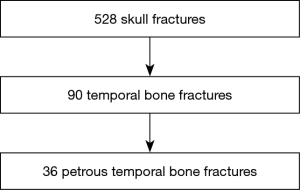
Five hundred and twenty-eight patients were admitted to our institution with a diagnosis of a traumatic skull fracture between January 2013 and December 2017. Ninety patients (17%) were diagnosed with a temporal bone fracture, of which 36 (7%) specifically involved the PTB. The median age was 7 years old and 63% of PTB fractures occurred in males. Two patients had bilateral PTB fractures (Figure 1).
With regards to temporal bone fracture classifications, 28 (78%) had longitudinal fractures and 32 (88%) had otic capsule sparing fractures. All subjects with an otic capsule violating fracture (n=4) had at least one direct otological or neurological complication. The most common mechanism of injury was a fall from height (69%) followed by motor vehicle accidents (17%) and blunt trauma (Table 1).
Table 1
| Characteristics | Values |
|---|---|
| Subject | N=36 |
| Sex (male) | 23 (63%) |
| Age range | 13 months to 15 years old |
| Median age (years) | 7 |
| Longitudinal PTB fractures | 28 (78%) |
| Otic capsule sparing PTB fractures | 32 (89%) |
| Bilateral PTB fractures | 2 (6%) |
| Mortality | 0 |
| Mechanisms of injury | |
| Fall from height | 25 (69%) |
| Motor vehicle accident | 6 (17%) |
| Blunt trauma | 5 (14%) |
Twenty-eight (78%) petrous temporal fractures were associated with an intracranial injury. These included pneumocephalus, extra-axial haemorrhage and traumatic brain injury. In this cohort, there were multiple associated injuries necessitating involvement from other surgical specialities including orthopaedic (6%), cardiothoracic (3%), oral & maxillofacial (6%), plastic & reconstructive (6%), and paediatric surgery (3%).
Of the 36 patients with PTB fractures, nine (25%) patients had at least one direct otological or neurological complication from their fracture, which consisted of FNP, CSF leak and/or hearing loss. Three (8%) had a transient FNP, two of which were moderate (HB 3 or 4), and one was mild (HB 2). All patients were initially treated with intravenous and subsequently oral steroids and had resolved at time of 3-month review. Three (8%) had biochemically proven CSF otorrhea, two of which spontaneously resolved within 1 week with non-surgical therapy. One patient with CSF otorrhea required the insertion of a lumbar drain and their CSF otorrhea subsequently resolved within 24 hours.
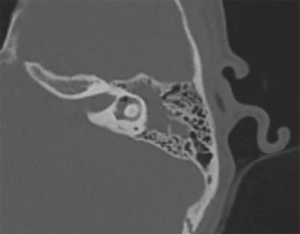
Seven patients (19%) had persistent hearing loss at 3 months proven with an audiogram. Two (6%) had a purely conductive hearing loss (CHL), four (11%) had a purely sensorineural hearing loss (SNHL) and one (3%) had a severe to profound mixed hearing loss. For the two who had purely CHL, neither were severe enough to necessitate any surgical intervention and one declined the offer of a hearing aid. Three patients with a unilateral SNHL, which included the patient with mixed hearing loss, were referred for consideration for a cochlear implantation. Of note, all patients with a CSF leak at time of injury were recorded to have a persistent SNHL at time of audiometric testing (Table 2, Figure 2).
Table 2
| Complications | Values |
|---|---|
| Subjects (n) | N=36 |
| FNP | 3 (8%) |
| CSF leak | 3 (8%) |
| Hearing loss at 3 months | 7 (19%) |
| Conductive hearing loss | 2 (6%) |
| Sensorineural hearing loss | 4 (11%) |
| Mixed hearing loss | 1 (3%) |
| Associated intracranial injury | 28 (78%) |
Discussion
This is the first paper to our knowledge to investigate PTB fractures in an Australian paediatric population. The overall prevalence of PTB fractures in paediatric patients who presented with a skull fracture was 7% in this study. The most common mechanism of injury was fall from height. This differs from previous studies that report motor vehicle accidents (MVAs) account for the most common cause of paediatric temporal bone fractures (3,11-13). A study by Waissbluth et al. found that MVAs made up the majority cause for temporal bone fractures and in particular, a large proportion was made up of uncommon vehicles types such as All-Terrain Vehicles (3). This was not apparent in our study and may relate to increased Australian public awareness about helmet use, road safety, and the dangers of quadbikes and farming equipment from national public health initiatives such as the Farmsafe guidelines on “Safety of quad bikes and side-by-side vehicles on Australian farms: a practical management guide” and the Royal Australasian College of Surgeons “Quad Bikes—Trauma prevention” position paper (14,15).
The majority of patients in our study had longitudinal PTB fractures and otic capsule sparing fractures. This is consistent with current literature (12,16). All the patients with otic capsule violating PTB fractures suffered at least one direct otological or neurological complication. This is similar to previous studies by Little et al. and Frisenda et al., who described that those with otic capsule violating fractures were more likely to develop SNHL, facial nerve injury and CSF otorrhea (4,17).
Only seven subjects (19%) were noted to have hearing loss at 3 months post injury in our study. This is lower than previously reported studies. Sheehan et al. previously showed that temporal bone fractures caused by MVA in recreational vehicles were associated with higher rates of otic capsule violation (21% vs. 5%) and hearing loss (30% vs. 16%) compared to other causes of head trauma (18). Therefore, the lack of MVAs accounting for injury mechanisms in this study may be a reason for our lower prevalence of hearing loss.
Bowman et al. showed that hearing loss in children was strongly associated with a temporal bone fracture compared to other head trauma, and suggested that any child with head trauma and clinical or radiological evidence of temporal bone fracture should have early hearing evaluation (19). It is currently not routine practice at our institution to get an audiogram in the acute setting of a PTB fracture. This is due to several reasons. Firstly, many of these patients have an associated neurological injury and therefore they are not clinically appropriate to participate in audiometric testing. Secondly, of those who are clinically appropriate in the acute setting, the observation has been that the majority of acute paediatric trauma patients are unwilling to actively engage in audiometric testing. It is standard practice at our institution for all paediatric patients with a PTB fracture to be given a course of intravenous and oral steroids. This practice has been extrapolated from studies which have shown that steroids help to reduce long term risk of SNHL in other forms of labyrinthine trauma such as cochlear implantation and sudden SNHL (20-23). Our institution also aims for patients with a PTB fracture to be seen within 3 months by the Otolaryngology, Head and Neck unit with audiometric testing. This is ideally followed audiometric testing at 6 and 12 months to ensure hearing remains stable. The low prevalence of hearing loss at 3 months in our study may stand to show that although hearing loss may be observed acutely, as seen with previous studies, that long term hearing outcomes in paediatric patients are good, the majority are self-resolving, and that empirical treatment with steroids may be beneficial. However, of the seven patients who did have a persistent hearing loss, three had a sensorineural hearing loss significant enough to warrant referral for a cochlear implant.
All patients with a FNP in this study were acutely treated with empirical steroids, as part of our institution’s standard practice of steroid use for sensorineural hearing preservation. There were no complete facial nerve palsies observed in our cohort and all facial nerve palsies had resolved at time of outpatient review. The use of steroids is likely to be useful in the setting of FNP based on its anti-inflammatory effect and the assumption that neural swelling is the primary driver for FNP in the traumatised but intact nerve (24). However, there is currently no strong evidence to substantiate this management in paediatric PTB fractures.
A study by Adepoju et al. reported a CSF leak rate of 2.3% in the setting of paediatric skull fractures (not specific to PTBs), whereas the prevalence of CSF leak in this study specific to PTBs was 8% (25). There are two potential reasons for this higher prevalence in our study. Firstly, the petrous portion of the temporal bone forms the majority of the lateral skull base and therefore a fracture running through this region is more likely to result in direct communication between the ear and the subarachnoid space compared to fractures going through any other portion of the temporal bone. The second reason is related to the density of the PTB and the large force required resulting in a significant fracture (2). This reason may also account for the large proportion of associated intracranial injuries seen in this study (78%), which is consistent with a previous study by Ort et al., who showed that the prevalence of concomitant intracranial injury was 75% (26). Despite the higher prevalence of CSF leaks in our study, all resolved over a short time period with either close clinical observation or insertion of a lumbar drain. No otological surgery was required for any patient with a CSF leak. The findings of this study appear to reflect current literature in that CSF otorrhea caused by temporal bone trauma usually resolves within 2 weeks without intervention and that surgical exploration is rarely required (27).
Based on the results of this study, we found that PTBs fractures are uncommon in children, but when present, they are a hallmark for a high-energy mechanism of trauma. They do not commonly occur in isolation, but rather are likely to be associated with a multisystem injury, in particular, intracranial injuries. As such, we recommend that all paediatric PTB fractures should be managed at a tertiary paediatric trauma centre. The direct complications associated with paediatric PTB fractures are overall uncommon, but when present, can have serious lifelong morbidity, and therefore early referral and multidisciplinary care is recommended (Table 3).
Table 3
| General recommendations for the early management of paediatric PTB fractures |
| • A paediatric PTB fracture is a hallmark for high energy trauma, and other associated injuries should be identified early, in particular intracranial complications; |
| • Early collaborative multidisciplinary management by trauma, neurosurgical and Otolaryngology, Head & Neck services are essential for appropriate and timely management of paediatric PTB fractures; |
| • Empirical steroids may be beneficial in reducing the risk of long term SNHL. |
| • Most complications directly related to a PTB fracture in paediatric patients will not require any acute surgical intervention; |
| • Follow up with an Otolaryngology, Head & Neck unit with audiometric testing is essential in paediatric patients with a PTB fracture; |
| • All paediatric PTB fractures should be managed at a tertiary paediatric trauma centre given the association with intracranial complications and the need for multidisciplinary team input. |
Limitations
The main limitation to this study was the small sample size. The small sample size was not conducive to any meaningful statistical analyses and therefore, it is difficult to draw definitive conclusions. A multi-centre study and a larger sample size over a longer time period would allow for greater analysis of the long term sequalae of paediatric PTB fractures and a better understanding of their true implications in the paediatric population.
Conclusions
PTB fractures are uncommon but are likely to be associated with intracranial complications, when observed in paediatric trauma. FNP and persistent hearing loss are infrequent debilitating complications of PTB fractures. Most otologic and neurologic complications directly related to PTB fractures will resolve with non-surgical management. No patients in our study population required otological surgery in the acute setting. Specific attention to the management of FNP and hearing loss are critical in the care of the child with a PTB fracture. Multidisciplinary care of the child with PTB fracture is recommended due to the significant related multisystem complications, and therefore all paediatric PTB fractures should be managed at a tertiary paediatric trauma centre.
Acknowledgments
We would like to thank the Trauma Services and Database Manager at the Royal Children’s Hospital for their assistance in data collection.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo.2020.03.05
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2020.03.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Royal Children’s Hospital Ethics Committee as a low-risk project and the requirement for consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Collins JM, Krishnamoorthy AK, Kubal WS, et al. Multidetector CT of temporal bone fractures. Semin Ultrasound CT MR 2012;33:418-31. [Crossref] [PubMed]
- Frisch T, Sørensen MS, Overgaard S, et al. Volume-referent bone turnover estimated from the interlabel area fraction after sequential labeling. Bone 1998;22:677-82. [Crossref] [PubMed]
- Waissbluth S, Ywakim R, Al Qassabi B, et al. Pediatric temporal bone fractures: A case series. Int J Pediatr Otorhinolaryngol 2016;84:106-9. [Crossref] [PubMed]
- Little SC, Kesser BW. Radiographic classification of temporal bone fractures: clinical predictability using a new system. Arch Otolaryngol Head Neck Surg 2006;132:1300-4. [Crossref] [PubMed]
- Leigh G, Ching TYC, Crowe K, et al. Factors Affecting Psychosocial and Motor Development in 3-Year-Old Children Who Are Deaf or Hard of Hearing. J Deaf Stud Deaf Educ 2015;20:331-42. [Crossref] [PubMed]
- Moeller MP, Tomblin JB. An Introduction to the Outcomes of Children with Hearing Loss Study. Ear Hear 2015;36:4S-13S. [Crossref] [PubMed]
- Eisenberg LS, Johnson KC, Martinez AS, et al. Studies in Pediatric Hearing Loss at the House Research Institute. J Am Acad Audiol 2012;23:412-21. [Crossref] [PubMed]
- Bogart KR, Tickle-Degnen L, Ambady N. Compensatory Expressive Behavior for Facial Paralysis: Adaptation to Congenital or Acquired Disability. Rehabil Psychol 2012;57:43-51. [Crossref] [PubMed]
- Masnari O, Schiestl C, Rössler J, et al. Stigmatization predicts psychological adjustment and quality of life in children and adolescents with a facial difference. J Pediatr Psychol 2013;38:162-72. [Crossref] [PubMed]
- VanSwearingen JM, Cohn JF, Bajaj-Luthra A. Specific impairment of smiling increases the severity of depressive symptoms in patients with facial neuromuscular disorders. Aesthetic Plast Surg 1999;23:416-23. [Crossref] [PubMed]
- Kang HM, Kim MG, Hong SM, et al. Comparison of temporal bone fractures in children and adults. Acta Otolaryngol 2013;133:469-74. [Crossref] [PubMed]
- Dunklebarger J, Branstetter B, Lincoln A, et al. Pediatric temporal bone fractures: current trends and comparison of classification schemes. The Laryngoscope 2014;124:781-4. [Crossref] [PubMed]
- Williams WT, Ghorayeb BY, Yeakley JW. Pediatric temporal bone fractures. The Laryngoscope 1992;102:600-3. [Crossref] [PubMed]
- Australian Centre for Agricultural Health and Safety, Farmsafe Australia. Safety of quad bikes and side-by-side vehicles on Australian farms: a practical management guide. Moree, N.S.W.: Australian Centre for Agricultural Health and Safety; 2011. [published 2016, accessed 23 December 2019]. Available online: http://keo-cms.appspot.com.storage.googleapis.com/sites/farmsafe/assets/bb5b4bee-7228-4fb5-85cf-ad81ad2ac444/Safe%20use%20of%20Quads%20and%20Side%20by%20Side%20Vehicles%20on%20Australian%20Farms%20Revised%202016.pdf
- The Royal Australasian College of Surgeons. RACS Position Paper: Trauma Prevention (Version 2) 2017. [published April 2017, accessed 23 December 2019]. Available online: https://umbraco.surgeons.org/media/1625/2017-04-12_pos_fes-fel-047_trauma_prevention.pdf
- Schell A, Kitsko D. Audiometric Outcomes in Pediatric Temporal Bone Trauma. Otolaryngol Head Neck Surg 2016;154:175-80. [Crossref] [PubMed]
- Frisenda JL, Schroeder JW, Ryan ME, et al. Cost effective use of audiograms after pediatric temporal bone fractures. Int J Pediatr Otorhinolaryngol 2015;79:1926-31. [Crossref] [PubMed]
- Sheehan CC, Lind M, Mahida JB, et al. Outcomes in pediatric patients with recreational vehicle related forceful head impact. Int J Pediatr Otorhinolaryngol 2016;84:97-100. [Crossref] [PubMed]
- Bowman MK, Mantle B, Accortt N, et al. Appropriate hearing screening in the pediatric patient with head trauma. Int J Pediatr Otorhinolaryngol 2011;75:468-71. [Crossref] [PubMed]
- Rajan GP, Kuthubutheen J, Hedne N, et al. The role of preoperative, intratympanic glucocorticoids for hearing preservation in cochlear implantation: a prospective clinical study. The Laryngoscope 2012;122:190-5. [Crossref] [PubMed]
- Eastwood H, Chang A, Kel G, et al. Round window delivery of dexamethasone ameliorates local and remote hearing loss produced by cochlear implantation into the second turn of the guinea pig cochlea. Hear Res 2010;265:25-9. [Crossref] [PubMed]
- Hu A, Parnes LS. Intratympanic steroids for inner ear disorders: a review. Audiol Neurootol 2009;14:373-82. [Crossref] [PubMed]
- Zadeh MH, Storper IS, Spitzer JB. Diagnosis and treatment of sudden-onset sensorineural hearing loss: a study of 51 patients. Otolaryngol Head Neck Surg 2003;128:92-8. [Crossref] [PubMed]
- Diaz RC, Cervenka B, Brodie HA. Treatment of Temporal Bone Fractures. J Neurol Surg B Skull Base 2016;77:419-29. [Crossref] [PubMed]
- Adepoju A, Adamo MA. Posttraumatic complications in pediatric skull fracture: dural sinus thrombosis, arterial dissection, and cerebrospinal fluid leakage. J Neurosurg Pediatr 2017;20:598-603. [Crossref] [PubMed]
- Ort S, Beus K, Isaacson J. Pediatric temporal bone fractures in a rural population. Otolaryngol Head Neck Surg 2004;131:433-7. [Crossref] [PubMed]
- Patel A, Groppo E. Management of Temporal Bone Trauma. Craniomaxillofac Trauma Reconstr 2010;3:105-13. [Crossref] [PubMed]
Cite this article as: Leung J, Levi E. Paediatric petrous temporal bone fractures: a 5-year experience at an Australian paediatric trauma centre. Aust J Otolaryngol 2020;3:6.


