
Outcomes in revision stapes surgery: ionomeric bone cement vs. malleostapedotomy in incus necrosis
Introduction
Otosclerosis is a relatively common condition, and has a reported frequency of 0.1–2.1% in the population (1). The treatment of otosclerosis has undergone considerable evolution, in particular with the advent of the stapedectomy in the mid-20th century (2). Despite recent advances however, the likelihood of requiring revision stapes surgery is as high as 20% (3). The most common indication for revision stapedectomy is delayed onset or persistent postoperative conductive hearing loss (CHL), although revision surgery may be indicated if new postoperative vestibular symptoms develop (3).
Revision surgery can present a challenge to the otologist because of the numerous causes of failure in stapes surgery and because revision surgery may necessitate a more technically complex reconstruction than in primary surgery. Mechanisms of failure include adhesions, prosthesis subluxation, incorrect prosthesis length, or incus erosion, subluxation or fixation, with incus pathology representing a particular challenge (4,5).
A wide range of techniques and materials have been reported in revision stapedectomies to address the various modes of failure, including a multitude of prostheses and bone cements. The technique of reconstruction used is, in general, determined by the status of the remaining incus and position of the existing prosthesis. Although rare, the simplest situation is a loose attachment of the existing piston which can be easily tightened by re-crimping. More commonly, the prosthesis is displaced, either from the incus long process, or from the stapedotomy, or both. If the incus is intact and normally mobile, then replacement with a new incus-vestibule prosthesis is appropriate. In the majority of cases, however, displacement is associated with partial or complete necrosis of the incus long process. In this situation the options are to attach a prosthesis to the remaining incus, or to bypass the incus with a malleus-vestibule prosthesis, or a total ossicular replacement prosthesis (TORP) with supporting graft at the footplate fenestra, dependent on the status of the remnant incus.
The literature suggests hearing results are generally poorer in revision surgery (6,7). Despite this, there is evidence to suggest that if the malleus and incus are intact, the results from revision surgery can approach those obtained in primary surgery (8-10). In cases of incus necrosis, outcomes are less well defined and may be inferior (11).
Our approach has been to utilize the remaining incus where possible. The new piston is connected to the proximal incus long process with the distal eroded portion repaired with bone cement. For this repair we have used an ionomeric bone cement, SerenoCemTM, however, we have recently changed to using a hydroxyapatite cement. We have not used other prostheses, such as the bucket handle type, nor attempted to reconstruct the incus long process with cement and then connect the prosthesis to the “new” incus. When there has been insufficient remaining incus long process, or after incus repair has already failed, we have used a malleus to vestibule reconstruction.
Since the late 1990’s it has been our preference to use Nitinol Fluoroplastic self-crimping prostheses both for primary stapedectomies and for revision procedures (12). A solid-state Green Dye 532 wavelength laser, delivered via a hand-held fibre probe, is used in all cases to divide adhesions and fibrosis at the oval window, facilitate atraumatic removal of the existing prosthesis, reopening of the stapedotomy and to activate crimping of the Nitinol prosthesis. We have found that the laser-activated crimping of the SMart Malleus Piston (Gyrus) facilitates a secure attachment to the malleus handle where conventional manual crimping is difficult and would require increased detachment of the tympanic membrane from the malleus.
Our observation has been that revision stapedectomy is usually well tolerated by the patients and can provide excellent hearing outcomes, but there is concern regarding the outcomes of revision surgery when incus necrosis is present. The technique of incudostapedotomy with glass ionomeric cement reinforcement of the incus long process, whilst providing good early results, appears to have a significant rate of delayed failure due to cement separation from the incus remnant and the prosthesis or increased erosion of the incus long process. In these cases of failure, further revision with glass ionomer cement repair of the incus has been attempted or a malleus-vestibule prosthesis has been placed. We have found that the malleostapedotomy procedure described above can provide excellent correction of the conductive loss. However, with a direct connection from the tympanic membrane and malleus handle to the vestibule, there is concern regarding possibly greater long-term risk to hearing and balance.
The aim of this study has been to review our outcomes with revision stapedectomy, in particular the long-term results using ionomeric cement repair of the incus compared with the technique of malleostapedotomy.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-83).
Methods
Study cohort
A retrospective analysis of a case series of patients undergoing revision stapes surgery between 2002–2018 by a single surgeon was performed. Potential cases were identified from a database of revision stapedectomy procedures and clinical records were reviewed. Subjects were included in the study if they had undergone a revision stapes procedure (either primary, secondary, tertiary etc. revision procedure) up to and including 2018. Subjects were excluded if (I) there was insufficient clinical details for analysis or (II) there was no record of follow-up.
Patient, surgical and outcome factors
Patient demographics such as age and sex were collated. Operative data recorded included date of surgery, operative side, type of prosthesis used in revision, cause of failure identified intra-operatively, and whether bone cement was utilised in surgery. Post-operative complications including sensorineural hearing loss (SNHL), vestibular symptoms and post-operative infections were also noted if recorded in post-operative medical notes.
Audiometry
Audiometric analysis was performed if there was both pre- and post-operative audiology and clear documentation of the prosthesis used intra-operatively. Revision stapedectomies where it was unclear what prosthesis was used, or where the prosthesis was simply left in place or repositioned were also excluded from audiometric analysis. Hearing outcomes were measured by pure tone average (PTA) and air-bone gap (ABG) pre- and post-operatively according to AAO-HNS guidelines (13). PTA was calculated using the average of hearing thresholds across four frequencies, 0.5, 1, 2, and 3 kHz frequencies for air conduction (AC) and 0.5, 1, 2, and 4 kHz frequencies for bone conduction (BC), pre-operatively and post-operatively. In some instances where recorded audiometry for BC lacked 4kHz data, 3kHz BC was used. ABG was calculated in the standard fashion using the difference in PTA at each time point (i.e., PTAair conduction – PTAbone conduction). Successful closure of the ABG postoperatively was defined as ABG ≤10 dB, while satisfactory closure was defined as 10.1–20 dB, and unsuccessful closure an ABG >20 dB. A change in ABG from pre- to post-operatively was also calculated by subtracting ABGpostop from ABGpreop (i.e., the more positive, the greater the treatment effect on the CHL). The pre-operative audiometry recorded was always the most recent audiometry prior to the surgery date. Our routine practice is for post-operative audiometry to be done 5 weeks and then approximately 6 months following surgery. For this analysis early outcomes were not used and where available, results taken as close to 6 months post-operatively as possible were used for all prostheses and also 12 months after the procedure for malleus prostheses.
The incidence of post-operative SNHL was derived by calculating the mean change in bone conduction PTA from pre- to post-operatively (BC PTApostop − BC PTApreop). This was also assessed by determining the number of prostheses which had an increase in bone conduction PTA >10 dB from pre- to post-operatively.
Prostheses
In this case series four different prostheses were used by the surgeon. The SMart Piston by Olympus which uses a heat activated Nitinol (nickel-titanium alloy) self-crimping wire loop to attach to the incus with a fluoroplastic piston. The SMart 360° by Olympus also uses a Nitinol wire that completely encircles the incus. The Eclipse piston by Grace Medical is also an incus-vestibule piston that is Nitinol-Fluoroplastic with 360° closure. The only malleus-vestibule prosthesis used in our series was the SMart Malleus piston by Olympus which was similarly composed of heat-activated Nitinol.
Statistical analysis
Data was compiled into Excel Version 16.16.22 (Microsoft Corp., Redmond, Washington, USA) for Mac (Cupertino, California, USA) and analysed using Excel’s computational functions.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics committee of the Royal Victorian Eye and Ear Hospital (ABN 81 863 814 677) and individual consent for this retrospective analysis was waived.
Results
One hundred and two revision stapedectomies performed on 80 patients were initially identified. After inclusion and exclusion criteria were applied, there were 77 patients who underwent 98 revision stapes procedures suitable for analysis of intra-operative findings. This consisted of 82 primary revisions and 16 re-revisions.
Of these, 55 patients who underwent 71 revision stapes procedures had complete data suitable for audiometric analysis. This consisted of 56 primary revisions and 15 re-revisions.
Demographic data
The average age of patients was 53 years (range, 14–80 years). The male to female ratio was 1:1.72. There were 44 operations performed on the right ear and 54 on the left ear. Of those with complete audiometry, the average age was 54 years (range, 14–75 years), with a male to female ratio of 1:1.84. There were 30 operations performed on the right ear and 41 operations performed on the left ear. The data is summarised in Table 1.
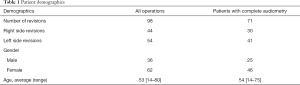
Full table
Intraoperative causes for failure
The various causes found intra-operatively for failure of primary stapes surgery are listed in Table 2. Incus necrosis was the most common finding, with or without displacement of the prosthesis or extensive adhesions, in 61 of 82 primary revision procedures (74.4%). All patients who underwent malleostapedotomy had incus necrosis, although some initially had an incus reconstruction attempted.
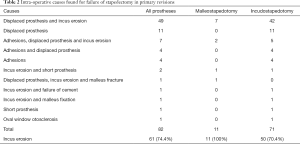
Full table
Audiometric results
The median pre-operative audiometry was performed 71 days pre-operatively (range, 1–478 days). The median post-operative audiometry was performed 210 days post-operatively (range, 8–1,383 days). For malleus-vestibule prostheses, longer term audiometric data was also collected and this was at a median of 483 days post-operatively (range, 325–962 days).
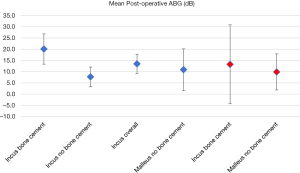
There were a total of 71 operations on 55 patients with complete audiometry and, overall, there was successful closure of the ABG in 43 (60.6%), satisfactory closure in 15 (21.1%) and unsuccessful closure in 13 (18.3%). The mean postoperative ABG for all prostheses was 12.6 dB (95% CI: 9.2–15.9 dB). The mean change in ABG from pre- to post-operative for all prostheses was 21.2 dB (95% CI: 17.1–25.3 dB).
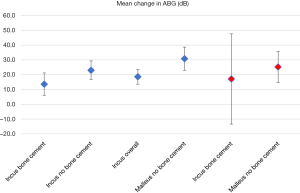
All audiometric results are listed in Table 3 and Figures 1,2.
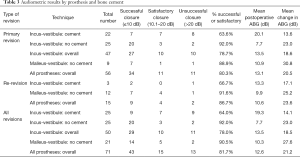
Full table
Primary revision—overall
There were 56 primary revision operations with complete audiometry. Overall, there was successful closure of the ABG in 34 (60.7%), satisfactory closure in 11 (19.6%), and unsuccessful closure in 11 (19.6%). The mean post-operative ABG was 13.1 dB (95% CI: 9.2–17.0 dB) and the mean change in ABG was 20.5 dB (95% CI: 16.0–25.1 dB).
Primary revision—incudostapedotomy
There were 47 incus-vestibule prostheses used in primary revision surgery with complete audiometry. In 22 cases SerenoCemTM bone cement was used in the revision whilst in the remaining 25 it was not.
For the bone cement group, in 7 cases (31.8%) there was successful closure of the ABG at 6 months, another 7 (31.8%) were satisfactory and 8 (36.4%) were unsuccessful. The mean post-operative ABG was 20.1 dB (95% CI: 13.4–26.9 dB) and the mean change in ABG was 13.6 dB (95% CI: 6.1–21.2 dB).
For the non-bone cement group in contrast, 20 (80.0%) were successful, 3 (12.0%) were satisfactory and only 2 (8.0%) were unsuccessful in closing the ABG. The mean post-operative ABG was 7.7 dB (95% CI: 3.3–12.1 dB) and the mean change in ABG was 23.0 dB (95% CI: 16.6–29.3 dB).
Primary revision—malleostapedotomy
There were 9 malleus-vestibule prostheses used in primary revision procedures.
For this group 7 (77.8%) were successful, 1 (11.1%) was satisfactory and 1 (11.1%) was unsuccessful in closing the ABG. The mean post-operative ABG was 10.9 dB (95% CI: 1.6–20.2 dB) and the mean change in ABG was 30.8 dB (95% CI: 22.9–38.6 dB).
Re-revisions—overall
There were 14 revisions of primary revision operations, performed on 13 patients with complete audiometry. One patient had re-revision of both ears. There was also one patient who had a third revision. Therefore, in total there were 15 operations performed on 13 patients which were re-revisions. In 12 procedures a malleus-vestibule prosthesis was used.
Overall, 9 (60.0%) were successful in closing the ABG, 4 (26.7%) were satisfactory and 2 (13.3%) were unsuccessful. The mean post-operative ABG was 10.6 dB (95% CI: 3.5–17.7 dB) and the mean change in ABG was 23.6 dB (95% CI: 13.6–33.5 dB).
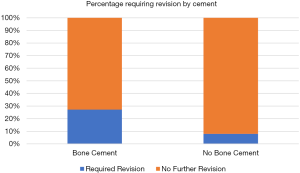
There were 47 incus-vestibule prostheses used in primary revision and 8 of these went on to have a re-revision. Of the 22 cases where SerenoCemTM was used in the primary revision, 6 (27.3%) required a subsequent revision. For the 25 cases where SerenoCemTM was not used in the primary revision, only 2 (8.0%) went on to have a subsequent revision. This is represented in Figure 3.
Re-revisions—incudostapedotomy
There were 3 incus-vestibule prostheses used in re-revisions with complete audiometry. Each of these SerenoCemTM. was used to facilitate incus long process repair and secure the prosthesis.
For this group, 2 (66.7%) had successful closure of the ABG, and 1 (33.3%) was unsuccessful. The mean post-operative ABG was 13.3 dB (95% CI: −4.2 to 30.9 dB) and the mean change in ABG was 17.1 dB (95% CI: −13.4 to 47.6 dB).
Re-revisions—malleostapedotomy
There were 12 malleus-vestibule prostheses used in re-revisions with complete audiometry. None of these used SerenoCemTM in their operation.
For this group 7 (58.3%) had successful closure of the ABG, 4 (33.3%) had satisfactory closure and 1 (8.3%) had unsuccessful closure. The mean post-operative ABG was 9.9 dB (95% CI: 1.8–17.9 dB) and the mean change in ABG was 25.2 dB (95% CI: 14.7–35.7 dB).
Long-term hearing outcomes for malleostapedotomy
There were 21 malleus-vestibule prostheses used in primary and subsequent revision operations overall and 14 (66.7%) were successful closing the ABG, 5 (23.8%) satisfactory and 2 (9.5%) unsuccessful. One unsuccessful case was subsequently revised and a short prosthesis (5.5 mm) successfully replaced with a longer prosthesis (6.0 mm). The mean post-operative ABG was 10.3 dB (95% CI: 4.4–16.3 dB) and the mean change in ABG was 27.6 dB (95% CI: 20.7–34.4 dB).
In order to study the long-term outcomes for malleus-vestibule prostheses, audiometry outcomes at 12 months and beyond were also considered. There were 7 malleus-vestibule prostheses which had both 6 months (median 252 days) and 12 months audiometry (median 483 days).
The mean postoperative ABG in the malleus-vestibule group at 6 months was 9.6 dB (95% CI: −3.7 to 23.0 dB). At 12 months, the mean post-operative ABG was 10.4 dB (95% CI: 0.6–20.1 dB). The mean change in ABG from 6 to 12 months post-operatively was 0.7 dB (95% CI: −3.6 to 5.0 dB).
Postoperative complications
The majority of procedures were performed in a day procedure setting and there were no cases of early severe vertigo or re-hospitalization.
In the initial post-operative period, there were no cases of significant SNHL. The mean change in bone conduction PTA for all prostheses was −3.6 dB (95% CI: −5.1 to −2.0 dB), for incus prostheses it was −3.2 dB (95% CI: −4.7 to −1.7 dB) and for malleus prostheses it was −4.4 dB (95% CI: −8.2 to −0.6 dB). Only two patients had an increase in bone conduction PTA >10 dB from pre-to post-operatively. One patient who received a Smart 360° had a pre-operative bone conduction PTA 15.0 dB which became 26.3 dB post-operatively (change: 11.3 dB). Another patient who received a SMart Malleus Piston had a pre-operative bone conduction PTA of 40.0 dB which became 52.5 dB post-operatively (change: 12.5 dB). One patient suffered a post-auricular wound infection at the site of fascia harvest where an underlay myringoplasty had been combined with revision incudostapedotomy.
Delayed complications were found in three patients with malleostapedotomy who suffered delayed onset of SNHL, between 1 and 4 years post-surgery. One developed positional vertigo and ear fullness 9 months post-operatively and then a sudden profound hearing loss in the operated ear 12 months post-operatively. Exploration of the ear was not possible as the patient was interstate. Another suffered vertigo induced by barotrauma when flying, 12 months post-operatively. Subsequently a steeply sloping SNHL was documented which has remained stable. A further patient had 25 dB increased low frequency SNHL 4 years post-operatively. This has also remained stable with functional hearing. In each case CT imaging confirmed satisfactory position of the malleostapedotomy prosthesis.
Another patient with far advanced otosclerosis underwent an incudostapedotomy revision. There was correction of the CHL, however subsequently the sensorineural loss progressed and cochlear implantation was performed.
Discussion
Our findings in this study highlight the particular challenges of revision stapedectomy. These include the many different mechanisms for failure after primary stapes surgery and the variety of methods available to correct them.
Despite the difficulty inherent in revision stapedectomy, our overall audiometric results were reasonable, with 81.7% achieving successful or satisfactory closure of the ABG (60.6% and 21.1% respectively), which is similar to rates reported elsewhere in the literature (6,14,15).
The most common cause of failure is necrosis of the incus long process. Whilst in some cases the residual incus can be utilized to reattach a prosthesis, with or without bone cement augmentation, the alternative is to bypass the incus with a malleostapedotomy prosthesis. A primary aim of this study was to compare the long-term results of ionomeric cement repair of the incus compared with malleostapedotomy.
Incus necrosis
The overriding mechanism of failure of primary stapes surgery, at least in part, was incus necrosis with 74.4% of patients demonstrating some element of this. Lesinski et al. also conducted a large retrospective analysis which found 31% of patients had complete incus necrosis and a further 60% had some degree of incus erosion (16). Lesinski et al. hypothesised that the preponderance of incus erosion in conjunction with a displaced prosthesis might be due to ongoing vibration of the ossicles against a prosthesis fixed against the solid otic capsule (16). Indeed, 49.0% of causes for failure in our series involved incus necrosis with a displaced prosthesis. Other retrospective analyses cite lower rates, with Blijleven et al. finding only 5% and Pitiot et al. finding 39.6% of patients had incus necrosis as the primary cause for failure (5,17). The main difference in these studies is that they reported what the surgeon deemed the primary cause of failure rather than the presence of any incus erosion and thus they may be underestimates.
Incudostapedotomy with bone cement vs. malleostapedotomy
When incudostapedotomy was the method of revision, it is clear that the use of ionomeric bone cement was associated with poorer hearing outcomes and an increased rate of further revision surgery at 6 months. Overall incudostapedotomy achieved successful or satisfactory closure of the ABG in 78.7%. However, with incudostapedotomy where bone cement was not used, this improved to 92.0% ABG ≤20 dB. This may be partly explained by case selection, with bone cement being used when there was a greater degree of incus necrosis. It is significant that in our experience, whilst usually providing early successful closure of the ABG, ionomeric bone cement reconstruction or reinforcement of the incus did not provide stable repair in approximately 30% of cases. The typical finding at further revision of these cases was that the cement had separated from the incus stump and the prosthesis was again displaced. In some cases there was further erosion of the incus with an apparent inflammatory process. The exact mechanism of failure is unknown and may be due to a technical issue at the time of application of the cement or related to biocompatibility. Ghonim et al. reported better outcomes using glass ionomer bone cements and found that they could achieve ABG closure <10 dB in 80% of cases with minimal necrosis of the long process of the incus (LPI), 81.5% in partial necrosis and with ABG closure <20 dB in all cases, but of note bone cement was only used in cases where there was minimal or partial necrosis with severe necrosis being managed by malleovestibulopexy (11).
Alternatives to glass ionomeric cements include hydroxyapatite cements with which Van Rompaey demonstrated closure of the ABG <10 dB in 20% and <20 dB in 80% (18). House, also using hydroxyapatite cement in revision stapedectomies with incus necrosis, reported closure of the ABG <10 dB in 81.1% and ABG <20 dB in 89.2% (19). Pitiot also conducted a retrospective review of hydroxyapatite bone cement used in revision stapedectomy and found that 45% had closure of the ABG <10 dB and 100% achieved closure <20 dB at 12 months post-operatively (5). Our practice has changed to utilise hydroxyapatite cement, however, long-term outcomes are not yet available.
The excellent audiometric outcomes achieved with malleostapedotomy in this series confirm that it is a reasonable option when intra-operative factors preclude the use of an incus-vestibule prosthesis. This reinforces the results of prior studies which justify the use of malleostapedotomy. Sarac et al. found malleus prostheses can achieve ABG closure <10 dB in 44% of patients and <20 dB in 72% of cases (20). Pitiot found that malleovestibulopexy could achieve ABG closure to within 10 dB in 60% of cases and to within 20 dB in 80% at 8 months post-operatively (5). These audiometric results were similar to revision stapedectomies where hydroxyapatite bone cement was used in their study (5). Fisch directly compared incudostapedotomy and malleostapedotomy and found the latter achieved an ABG <10 dB in 52.1% of cases and an ABG <21 dB in 80.2% (10). This reflected better closure of the ABG than the incus group (10). The SMart Malleus used in our study achieved similar, if not slightly better, hearing results of 66.7% with an ABG ≤10 dB and 90.5% with an ABG ≤20 dB.
Reassuringly, our study also suggests that malleus pistons offer stable hearing outcomes for patients up to 12 months post-operatively. Though subject numbers were small, the mean change in ABG was only 0.7 dB (95% CI: −3.6 to 5.0 dB) between 6 and 12 months post-operatively. These optimistic results must be counterbalanced with the fact that three patients receiving malleostapedotomy went on to have late complications involving SNHL. There are few reported studies which consider audiometric outcomes for malleostapedotomy beyond 12 months postoperatively and these have tended to include pathologies in addition to otosclerosis (21,22). Further long-term studies of hearing outcomes of incus and malleus prostheses in revision stapedectomies will be helpful in understanding the reliability and safety of both techniques. Nevertheless, our data affirms that malleostapedotomy is a reasonable option in patients with incus necrosis where incudostapedotomy is technically difficult or not possible.
Our present series demonstrates malleostapedotomy is at least comparable if not better than incudostapedotomy combined with glass ionomeric bone cement. As such, there is justification for earlier consideration of malleostapedotomy in patients where significant incus erosion means that incudostapedotomy alone will not be sufficient. However, hydroxyapatite cements may be more reliable than glass ionomeric cements in revision stapedectomy, so the use of bone cements in revision stapedectomy where incus necrosis is present should not be disregarded and is in need of further research. There is already excellent evidence showing that hydroxyapatite demonstrates good biocompatibility and has osteoconductive properties facilitating bony growth (23).
Re-revisions
Re-revisions were not common in this series, but when performed were generally successful with similar hearing outcomes to primary revision stapedectomies with 60% achieving successful ABG closure and 26.7% satisfactory closure. Only one patient had a third revision procedure. Re-revisions tended to be performed with a malleus-vestibule prosthesis in our series, again highlighting the robustness of this technique.
Post-operative complications
Whilst there were no cases of significant SNHL at 6-month follow-up, it remains a concern that several patients with malleus-vestibule prostheses developed SNHL between 1 and 4 years post-operatively. Although the mechanism in these cases is unknown, it may be that the direct connection from the tympanic membrane and malleus to the vestibule is less stable and so there is possibly greater long-term risk to hearing and balance. Whether this is a significant long-term risk of malleostapedotomy that should influence indications for its use, will require further research.
Study limitations
Limitations of this study include its retrospective nature and the small numbers in some intervention groups. While overall study numbers are large compared to similar studies in the literature, the sample size for each group of procedures was relatively small and so comparisons between different procedures have to be interpreted with caution. This is particularly relevant for the relatively small number of patients who received malleostapedotomy with 12-month audiometry data. A retrospective analysis where inclusion criteria require post-operative follow-up may also introduce selection bias with patients who had a good outcome not attending or vice versa. This study has the benefit of reducing performance bias by analysing the results of a single senior surgeon who performed all the revision procedures in this study. However, it is possible that comparisons between procedures suffer from the fact that differences in outcome may be influenced by evolution of surgical technique, availability of materials, and the underlying cause of failure. Despite these limitations, our data is consistent with and adds to the existing literature on the success of revision stapedectomy and on the utility of malleostapedotomy in complex ossicular disease.
Conclusions
Our data confirms that revision stapes surgery, despite its challenges, can provide excellent audiometric outcomes. Importantly, this research indicates that there should be less hesitation to perform malleostapedotomy in cases of incus necrosis. Better outcomes have been demonstrated with malleostapedotomy than with glass ionomeric cements in revision stapedotomies. Further research into the utility and stability of other bone cements and techniques for repair of different degrees of incus necrosis may help to guide intra-operative decision making.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-83
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-83
Peer Review File: Available at http://dx.doi.org/10.21037/ajo-20-83
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-83). RB serves as an unpaid editorial board member of the Australian Journal of Otolaryngology from Jan 2019 to Dec 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics committee of the Royal Victorian Eye and Ear Hospital (ABN 81 863 814 677) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Crompton M, Cadge BA, Ziff JL, et al. The Epidemiology of Otosclerosis in a British Cohort. Otol Neurotol 2019;40:22-30. [Crossref] [PubMed]
- Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy Versus Stapedotomy. Otolaryngol Clin North Am 2018;51:375-92. [Crossref] [PubMed]
- Ozüer MZ, Olgun L, Gültekin G. Revision stapes surgery. Otolaryngol Head Neck Surg 2012;146:109-13. [Crossref] [PubMed]
- Schmid P, Häusler R. Revision stapedectomy: an analysis of 201 operations. Otol Neurotol 2009;30:1092-100. [Crossref] [PubMed]
- Pitiot V, Hermann R, Tringali S, et al. Revision stapes surgery for lysis of the long process of the incus: comparing hydroxyapatite bone cement versus malleovestibulopexy and total ossicular replacement prosthesis. Eur Arch Otorhinolaryngol 2016;273:2515-21. [Crossref] [PubMed]
- Lippy WH, Battista RA, Berenholz L, et al. Twenty-year review of revision stapedectomy. Otol Neurotol 2003;24:560-6. [Crossref] [PubMed]
- Meyer TA, Lambert PR. Primary and revision stapedectomy in elderly patients. Curr Opin Otolaryngol Head Neck Surg 2004;12:387-92. [PubMed]
- Lesinski SG. Revision stapedectomy. Curr Opin Otolaryngol Head Neck Surg 2003;11:347-54. [Crossref] [PubMed]
- Lesinski SG. Revision surgery for otosclerosis: 1998 prospective. Oper Tech Otolayngol Head Neck Surg 1998;9:72-81. [Crossref]
- Fisch U, Acar GO, Huber AM. Malleostapedotomy in revision surgery for otosclerosis. Otol Neurotol 2001;22:776-85. [Crossref] [PubMed]
- Ghonim M, Shabana Y, Ashraf B, et al. Revision Stapedectomy with Necrosis of the Long Process of the Incus: Does the Degree of Necrosis Matter? A Retrospective Clinical Study. J Int Adv Otol 2017;13:28-31. [Crossref] [PubMed]
- Pudel EI, Briggs RJ. Laser-assisted stapedotomy with a Nitinol heat-crimping prosthesis: Outcomes compared with a platinum fluoroplastic prosthesis. Otolaryngol Head Neck Surg 2008;139:51-4. [Crossref] [PubMed]
- . Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. AmericanAcademy of Otolaryngology-Head and Neck Surgery Ffoundation, Inc. Otolaryngol Head Neck Surg 1995;113:186-7. [Crossref] [PubMed]
- Hammerschlag PE, Fishman A, Scheer AA. A review of 308 cases of revision stapedectomy. Laryngoscope 1998;108:1794-800. [Crossref] [PubMed]
- Vincent R, Rovers M, Zingade N, et al. Revision stapedotomy: operative findings and hearing results. A prospective study of 652 cases from the Otology-Neurotology Database. Otol Neurotol 2010;31:875-82. [Crossref] [PubMed]
- Lesinski SG. Causes of conductive hearing loss after stapedectomy or stapedotomy: a prospective study of 279 consecutive surgical revisions. Otol Neurotol 2002;23:281-8. [Crossref] [PubMed]
- Blijleven EE, Wegner I, Tange RA, et al. Revision Stapes Surgery in a Tertiary Referral Center: Surgical and Audiometric Outcomes. Ann Otol Rhinol Laryngol 2019;128:997-1005. [Crossref] [PubMed]
- Van Rompaey V, Claes G, Somers T, et al. Erosion of the long process of the incus in revision stapes surgery: malleovestibular prosthesis or incus reconstruction with hydroxyapatite bone cement?. Otol Neurotol 2011;32:914-8. [Crossref] [PubMed]
- House JW, Lupo JE, Goddard JC. Management of incus necrosis in revision stapedectomy using hydroxyapatite bone cement. Otol Neurotol 2014;35:1312-6. [Crossref] [PubMed]
- Sarac S, McKenna MJ, Mikulec AA, et al. Results after revision stapedectomy with malleus grip prosthesis. Ann Otol Rhinol Laryngol 2006;115:317-22. [Crossref] [PubMed]
- Rambousek A, Schlegel CH, Linder TE. From incus bypass to malleostapedotomy: technical improvements and results. J Laryngol Otol 2012;126:995-1002. [Crossref] [PubMed]
- Burggraaf J, Mylanus EAM, Pennings RJE, et al. Malleostapedotomy with the self-fixing and articulated titanium piston. Eur Arch Otorhinolaryngol 2018;275:1715-22. [Crossref] [PubMed]
- Costantino PD, Friedman CD, Jones K, et al. Hydroxyapatite cement. I. Basic chemistry and histologic properties. Arch Otolaryngol Head Neck Surg 1991;117:379-84. [Crossref] [PubMed]
Cite this article as: McOwan B, Lim JWJ, Lee WS, McOwan M, McLean T, Mitchell-Innes A, Briggs R. Outcomes in revision stapes surgery: ionomeric bone cement vs. malleostapedotomy in incus necrosis. Aust J Otolaryngol 2021;4:14.


