
Cernea Manoeuvre—abdominal compression to detect chyle leak
Introduction
Chyle leak is an uncommon, but morbid, complication of head and neck surgery. Aides to identify the thoracic duct can reduce incidence of leaks. We describe the Cernea manoeuvre as an adjunctive measure in recognising the duct and leaks intraoperatively.
Methods
Following head and neck surgery in proximity to the left cervical thoracic duct, careful inspection for chyle leak is performed, concurrent with haemostasis. We perform a Valsalva manoeuvre to increase intrathoracic pressure and examine for chyle leak. Trendelenburg positioning may also facilitate identification of chyle. Particular attention is paid to the region near level IV which may be involved in complex thyroidectomies and low or lateral neck dissections.
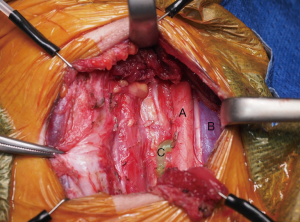
Firstly, the anaesthetist disconnects the ventilator to prevent chest splinting and keep intrathoracic venous pressure low. During this, the surgical assistant applies continuous pressure on the abdomen whilst the thoracic duct and adjacent soft tissues are paid particular attention (Figure 1). This promotes propulsion of chyle through the chest and into the cervical thoracic duct. Surgical magnified loupes can aid with detailed inspection. The duct will dilate (Video 1) and unsealed lymphatic vessels should be prompted to extrude milky-white fluid to enable identification and ligation. This manoeuvre is repeated with intervening periods of normal ventilation to ensure adequate occlusion of any offending lymph ducts.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from the patient for publication of this study and any accompanying images.
Discussion
Iatrogenic chyle fistulas from cervical thoracic duct injury is an uncommon complication of head and neck surgery that carries significant morbidity and rarely, mortality (1,2). Intraoperatively, the thoracic duct should be carefully visualised and any identified chyle leak should be repaired. Increase in intraluminal pressure is thought to dilate the vessel and aides to assist visualisation of the duct ensure meticulous ligation and reduce complication rates.
Intraoperative thoracic duct identification is important to prevent injury and complications from post-operative chyle fistula (1). Sequelae following chyle leaks include protein and fat malabsorption, which can result in malnutrition, weight loss, electrolyte disturbance and immunosuppression (3). Wound healing may be compromised from persistent high-volume chyle extravasation as well as secondary infection that may result in skin flap failure (4). In very rare cases, usually in high volume leaks, life threatening chylothorax can occur (5).
Several alternative options exist to assist operative thoracic duct identification though evidence for sensitivity is sparse. The mechanism for cervical thoracic duct dilatation is proposed to be secondary to increased hydrostatic pressure. Raising intrathoracic pressure with a Valsalva manoeuvre (6) and subsequent increased intraabdominal pressure with the Cernea manoeuvre can aid in dilating the duct. In a single study, the abdominal compression manoeuvre identified occult intraoperative chyle leak in 6.3% of patients (7). Lymphangiography has also been suggested with use of an infrared camera and intravenous Indocyanine Green (ICG). In the only small series on neck dissections, ICG identified five of six thoracic ducts (83.3%). Its application is limited by poor fine tissue penetration of ICG, additional equipment requirement and cost, and added anaesthetic time (8).
Conclusions
The Cernea manoeuvre is a readily available, quick and reliable intraoperative technique for any head and neck surgeon to identify the cervical thoracic duct and prevent post-operative chyle leak.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-64). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Delaney SW, Shi H, Shokrani A, et al. Management of Chyle Leak after Head and Neck Surgery: Review of Current Treatment Strategies. Int J Otolaryngol 2017;2017:8362874 [Crossref] [PubMed]
- Hong YT, Hong KH. Identification of lymphatic channels in the tracheoesophageal groove during central neck dissection for thyroid cancer. Head Neck 2018;40:E87-90. [Crossref] [PubMed]
- Sriram K, Meguid RA, Meguid MM. Nutritional support in adults with chyle leaks. Nutrition 2016;32:281-6. [Crossref] [PubMed]
- Broughton G 2nd, Janis JE, Attinger CE. The basic science of wound healing. Plast Reconstr Surg 2006;117:12S-34S. [Crossref] [PubMed]
- Prabhu V, Passant C. Left-sided neck dissection and chylothorax: a rare complication and its management. J Laryngol Otol 2012;126:648-50. [Crossref] [PubMed]
- Kumar CM, Van Zundert AAJ. Intraoperative Valsalva maneuver: a narrative review. Manœuvre de Valsalva peropératoire: une revue narrative. Can J Anaesth 2018;65:578-85. [Crossref] [PubMed]
- Cernea CR, Hojaij FC, De Carlucci D Jr, et al. Abdominal compression: a new intraoperative maneuver to detect chyle fistulas during left neck dissections that include level IV. Head Neck 2012;34:1570-3. [Crossref] [PubMed]
- Chakedis J, Shirley LA, Terando AM, et al. Identification of the Thoracic Duct Using Indocyanine Green During Cervical Lymphadenectomy. Ann Surg Oncol 2018;25:3711-7. [Crossref] [PubMed]
Cite this article as: Phung D, Palme CE. Cernea Manoeuvre—abdominal compression to detect chyle leak. Aust J Otolaryngol 2021;4:15.


