
Permeatal ‘push through’ myringoplasty in the Northern Territory: a prospective cohort
Introduction
Myringoplasty is a surgical procedure that continues to evolve with the advances in technology, technique, instruments, and prostheses. Various techniques have been described to overcome the various challenges in myringoplasty surgery, especially in anterior perforations. These often involve postauricular approach, which is a longer, more complex procedure that is favoured for its exposure of the middle ear and the entire tympanic membrane. Transcanal approaches had conventionally been restricted to smaller perforations, due to the concerns of the limited visibility offered by this approach.
More recent studies using the transcanal “push-through” myringoplasty technique have demonstrated that it to be very feasible and effective. These studies have mostly described an endoscopic transcanal technique to overcome the challenges of narrow ear canals and provide a wider surgical view.
The present study was conducted in the Northernmost ‘Top End’ of the Northern Territory of Australia. The patient population comprises the catchment areas of the Royal Darwin, Katherine District and Gove District Hospitals. These hospitals serve many Indigenous communities. These communities are geographically remote and logistically isolated. Poor nutrition, poor compliance with medical treatment, lower socio-economic status and educational levels all add additional challenges to obtaining optimal outcomes for any surgical procedure.
The heavy burden of ear disease due to perforations in the Indigenous population is well established. Indigenous children suffer from higher rates of tympanic perforation than their non-Indigenous counterparts with prevalence as high as 60% at 2 years of age and continuing above 10% over the age of 16 (1-3). Previous studies assessing the efficacy of myringoplasty in the Indigenous populations, using a range of techniques and graft materials, have reported mixed outcomes with neo-tympanum integrity ranging from 30–60.1% (4-9). This differs from the results in non-Indigenous patients where a closure rate of 90% can be expected (2). The follow-up rates in these studies have generally been low (from 25–78%), attributable to the remoteness of the communities and to the challenge of accessibility to healthcare due to language and cultural barriers (2,4,5).
Our surgical unit began to adopt per-meatal myringoplasty techniques for a number of reasons. Post-auricular and endaural incisions were prone to infections (up to 38%), wound dehiscence and keloid scarring occasionally occurred (5). Compliance with analgesia post operatively was not always optimal, and a smaller incision presumed to be less painful. Anecdotally, we also noted if a complication such as wound dehiscence occurred in a community, attitudes towards ear surgery might become appreciably negative for some time.
In this study, we report our outcomes of the transcanal “push-through” myringoplasty technique, aiming to evaluate the rate of graft success, hearing outcomes, and complications.
Methods
Patients
This was a multi-centre prospective case series study of patients who underwent transcanal “push-through” myringoplasty in the Northern Territory of Australia from January 01, 2012 to January 01, 2014. The surgeries were performed at Royal Darwin Hospital (RDH), Gove District Hospital (GDH) and Katherine District Hospital (KDH). Patients were recruited via referrals from the Northern Territory Hearing Health program, the otolaryngology outpatient clinics in the aforementioned hospitals, and Otolaryngology Remote Outreach clinics in the remote communities. All patients who had tympanic membrane perforations and consented to myringoplasty surgery were recruited, unless there was insufficient rim of remnant tympanic membrane to perform the transcanal “push-through” myringoplasty. Patients with wet perforations would still receive surgery, and were included in this study. Patients who had cholesteatoma were excluded.
All patients underwent a pre-operative audiogram. A member of the ENT team, comprising of the trainee, fellow or consultant, performed the procedures and the ENT consultant supervised all procedures. The patients were assessed again post-operatively between 1–5 months (this variability is due to complex transport arrangements and difficulty in follow-up for remote patients) and again after 12 months. An assessment of the perforation closure and audiogram is performed at each follow-up interval. We recorded preoperative and postoperative audiograms of the patients at frequencies of 500 Hz, 1, 2, and 4 kHz to assess the closure of air-bone gaps.
To minimise follow-up drop-out, if patients failed to show at their follow-up appointment, invitation letters were sent and visits by clinical nurse practitioners to patient’s communities/homes were scheduled. The community primary health care provider would also be contacted to help encourage follow-up.
Surgical technique
The per-meatal ‘push through’ myringoplasty was performed as described by Tos [2009] (10). The external auditory meatus and canal is infiltrated with local anaesthetic using 2–5 mL of 2% lignocaine with 1:80,000 adrenaline. Following preparation of the sterile field with half strength betadine, the field is draped using a fenestrated sheet. The canal, tympanic membrane and the middle ear is sterilised using povidone-iodine 5% solution, then irrigated with normal saline, and lastly instilling the canal with ciprofloxacin 0.3% solution. A tragal cartilage-perichondrium composite graft (with the perichondrium stripped from one side) was used. This was harvested through a 1 cm incision medial to the free border of the tragus. The cartilage part of the graft was fashioned be just slightly larger than the perforation. A cuff of perichondrium is left around the cartilage graft. After freshening the perforation margin, the size of the perforation is measured using absorbable gelatin sponge (Gelfoam®; Pfizer) templates that are made using aural speculums of various sizes as a ‘cookie cutter’. The ‘templates’ are left in the middle ear as part of the middle ear packing. The middle ear is then packed with Gelfoam®. The same speculum that was used to make the optimally sized Gelfoam template is pushed into the harvested tragal cartilage to form the graft. The cartilage graft is “pushed through” the perforation to allow it to occlude the perforation, much like an inlay graft but with a layer of perichondrium medially. The perichondrial cuff is tucked medially under the edges of the perforation in an underlay manner. In larger perforations, a notch is made in the cartilage to accommodate the handle of malleus, but not the perichondrium. This allows the perichondrial cuff of the graft to be positioned snugly against the malleus handle. Gelfoam® soaked with antibiotic drops (ciprofloxacin 0.3%) and then dissolvable haemostatic oxidised cellulose polymer matrix (Surgicel® Fibrillar™; Ethicon, Inc) is used to splint the graft laterally.
Outcomes
The primary outcome was the overall graft success rate, measured at both time intervals as described above. Pure-tone average (PTA), which is the average of air-conduction hearing sensitivity at 500, 1,000 and 2,000 Hz, was used as the primary audiological outcome as it best approximates the speech reception threshold and hence provides a good approximate of functional hearing. The air-bone gap was also analysed.
Statistical analyses were performed using the SPSS statistics for MacOS software, version 22. Non-parametric results were expressed as median and interquartile range (IQR). Fisher’s exact test was used to compare categorical data. Related samples Wilcoxon signed-rank test was used to compare pre- and post-operative audiological outcomes. A result of P<0.05 was considered statistically significant.
Ethics
This study was reviewed and approved by the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health research (HREC reference number 2017-3020). All subject, or their caregivers if they were under 18 years old, have signed informed consent forms for participation in this study. The study outcomes will not affect the future management of the patients. The authors have no conflicts of interest to declare.
Results
Patient characteristics
A total of 241 patients were included in this study. The median age of patients was 12.7 years (IQR 10, range 5–72). Fifteen point eight percent of patients were under 8 years old. Two hundred ten (87.3%) of the patients were of Australian Indigenous ethnicity, while the rest were non-Indigenous. The follow-up rate at the first 1–5 months period is 64.7% (156 patients). Beyond 12 months, 50.6% (122 patients) of patients were available for the second follow-up. Details of these are listed in Table 1.
Table 1
| Variable | Result |
|---|---|
| Total patients (pre-operation) | n=241 |
| Australian Indigenous | 210 (87.1%) |
| Non-Indigenous | 31 (12.9%) |
| Age (years) | 12.7 (IQR, 10) |
| Pre-operative perforation size | |
| <40% of tympanic membrane | 146 (60.6%) |
| >40% of tympanic membrane | 45 (18.7%) |
| Subtotal | 50 (20.7%) |
| Pre-operative hearing | |
| PTA (dB) | 36.7 (IQR, 20) |
| >30 dB hearing loss (%) | 67.60% |
| Air-bone gap (dB) | 30.0 (IQR, 15) |
| Follow-up (number of patients) | |
| 1–5 months | 156 (64.7%) |
| >12 months | 122 (50.6%) |
| First follow-up (1–5 months) | n=156 |
| Intact tympanic membrane | 136 (87.2%) |
| Hearing outcomes | |
| PTA (dB) | 23.3 (IQR, 16) |
| >30 dB hearing loss (%) | 20.70 |
| Air-bone gap (dB) | 21.7 (IQR, 12) |
| Second follow-up (>12 months) | n=122 |
| Intact tympanic membrane | 103 (84.4%) |
| Hearing outcomes | |
| PTA (dB) | 21.7 (IQR, 14) |
| >30 dB hearing loss (%) | 14.90 |
| Air-bone gap (dB) | 21.3 (IQR, 13) |
IQR, interquartile range.
Outcomes
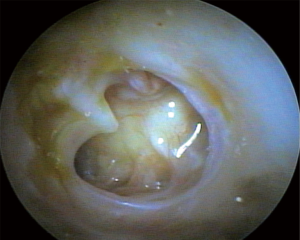
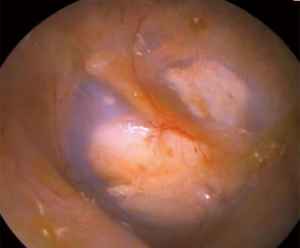
On the pre-operative assessment, 50 (20.7%) patients had subtotal perforations (Figure 1), 45 (18.7%) had a perforation occupying at least 40% of the tympanic membrane, while the other 146 (60.6%) had small perforations under 40% of the tympanic membrane. Postoperatively at 1–5 months, 87.2% of patients that were followed-up had successful grafts and intact tympanic membranes. Beyond 12 months, 84.4% of patients that were followed-up continued to have intact grafts and tympanic membranes (Figure 2). There was no significant correlation between the preoperative perforation size and graft success rate at 1–5 months (P=0.21) and beyond 12 months (P=0.29).
In the subgroup analysis by ethnicity, at the first and second follow-up intervals, Indigenous Australian patients had a graft success rate of 85.2% and 82.7%, respectively. In contrast, none of the non-Indigenous patients had graft failures. This difference was statistically significant for the 1–5 months interval (P<0.05) but not for beyond 12 months (P=0.12).
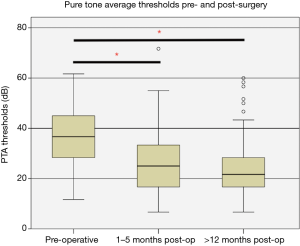
Prior to surgery, 67.6% of patients had >30 dB of hearing loss. At the first and second follow-up visits, the proportion of this had significantly reduced to 20.7% and 14.9%, respectively (P<0.01). The median preoperative PTA levels were 36.7 dB (IQR, 20). This was significantly reduced to 23.3 dB (IQR, 16) at 1–5 months (P<0.01), and then to 21.7 dB (IQR, 14) at the 12-month follow-up (Figure 3). There was no significant difference in PTA levels between the two post-operative visits (P=0.61).
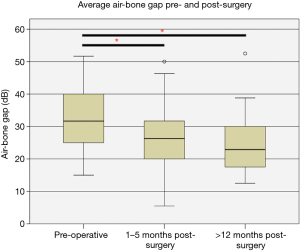
The median preoperative air-bone gap was 30.0 dB (IQR, 15). After the surgery at 1–5 months, the median air-bone gap was significantly reduced to 21.7 dB (IQR, 12) (P<0.01). The median air-bone gap was 21.3 dB (IQR, 13) beyond 12 months—not significantly changed compared to the result at 1–5 months (P=0.324) (Figure 4).
Complications
No post-operative complications were recorded in this cohort. It is likely that some patients would have experienced post-operative infection. Given that prophylactic topical antibiotics were used, many of these would have cleared by the time of follow-up.
Discussion
The graft success rate in this study is closely comparable to the success rates of recent studies that describe the push-through cartilage myringoplasty techniques (85–95%) (11-15). Tseng et al. (2017) recently compared the push-through tympanoplasty technique with transcanal technique that involves a tympanomeatal flap elevation, showing similar outcomes with either technique (15). In our experience, when combined with an endoscopic approach in select cases, per-meatal “push-through” myringoplasty can be very versatile in a variety of settings. In our study, the success rate did not vary according to the preoperative perforation size, which proves this point. Of note, most patients in this study are younger than 12 years old, with 15.8% of patients under 8 years old, demonstrating the adaptability to younger patients. These findings are different from some of the previous studies, where larger perforations and younger age were negatively correlated to success rates (12,16,17).
The rate of graft success in this cohort is relatively high when compared to previous studies involving Indigenous Australians (30–64%) (4,5). However there remains a significant gap when compared to results achievable in non-Indigenous populations. This gap had been reported in previous studies showing up to 10% more postoperative infection rates in the Northern Territory of Australia compared to international rates (18). Likewise, graft failure rate in previous studies have been very high. In the study by Guerin et al., a similar per-meatal ‘push through’ technique was employed, but the closure rate was much lower −51.3%. This was thought to be due to the high prevalence of otorrhoea pre-operatively (4). In the 1990s, Foreman et al. noted that the poor success rates (39%) of myringoplasty in the Northern Territory were associated with a high rate of post-operative infections (38%) (5). Factors that may account for the disparity in success rates include geographical isolation, the higher humidity during the wet season, poorer general health, poor socio-economic factors and overcrowding (2,4,19). Higher nasopharyngeal bacterial load and more frequent colonisation by otopathogens may influence the rate of post-operative infections, causing a higher failure rate in the Indigenous population (19). In the current study, the relatively low rate of graft failure may reflect the role of prophylactic ciprofloxacin ear drops in the pre- and post-operative period. The preoperative ear toileting with the povidone-iodine solution may also be contributory. Part of this success compared to previous studies in this population is also due to the broader ongoing public health interventions in Australia to improve Indigenous ear health.
Cartilage grafts have particular advantages that are well suited to myringoplasty in the challenging population in this study. The anatomical stability of the cartilage graft and its resistance to retraction protects against negative middle ear pressure and against reperforation. The perichondrial cuff that is tucked under the perforation helps establish contact between the cartilage and the rim of the perforation. In this operation, only one small tragal incision is required to harvest the cartilage, which speeds up the procedure time, postoperative recovery, and simplifies post-operative care. This allows the surgery to be performed as a day-case, making it particularly suited for patients from rural and remote areas with no specialist facilities. The hardy nature of the graft proved useful in the challenging patient population in this study.
Although the cartilage graft is very resilient, the thickness and hardness of it impacts upon audiological outcomes. Given the challenging patient characteristics, the primary aim of surgery in this cohort is to provide a dry, waterproof ear, with hearing improvement being a secondary outcome. Nevertheless, the hearing outcomes of this cohort were comparable to other studies (13-15,20-22). There was a significant improvement across all audiological outcomes in this study—including pure-tone average thresholds and air-bone gap closure. The magnitude of improvement is slightly lower than some of the previous studies where the authors had thinned down the cartilage graft. However, this is calculated trade-off between graft resilience and success versus hearing improvement in our population group. None of the patients had significant complications.
Limitations
The follow-up rate of our cohort (50–64%) is comparable to previous studies (32–80%) (4,5,7-9). Ensuring the follow-up of the patient in the remote Indigenous communities is inherently challenging and previous studies attributed the nomadic nature of many of the patients and lower accessibility to primary care as a hurdle to reaching high rates of follow-up (9,23). There are several tiers of service provision set up at our unit to improve access to hearing health for the Indigenous Australian communities. This including the community outreach programs and specialist visits to remote communities. The aim of these programs is to provide quality community based and culturally appropriate services to improve hearing health and post-operative outcomes (2). Despite this, a proportion of patients miss appointments or do not show for their planned surgery. MacKendrick (1999) made the observation that it is unknown whether the patients who did not return for follow-up had failed and were disappointed, or whether their hearing improved and they felt it no longer necessary, especially for the remote patients who are only accessible by flight (9). This introduces a selection bias to the study. Nevertheless, with similar follow-up rates to previous studies of similar patient populations, the relative improvement in surgical outcomes in this current study is heartening.
Conclusions
Transcanal “push-through” cartilage myringoplasty is a versatile technique that can be applied to most perforations. It is safe and effective in terms of graft success and hearing outcomes, including in a paediatric setting. Even in a challenging population like that seen in Indigenous Australian (due to remoteness, disease burden and other health barriers), the outcomes remain relatively good. The relatively simplicity of the procedure, short duration of hospital stay, and minimal post-operative care, makes it a suitable technique for use in rural and remote populations.
Acknowledgments
We thank Mr. Christian Aguilar, Ms. Kellyanne Coyle, and the Northern Territory Hearing Health Program for their assistance in the various aspects of the research on which this work is based.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health research (HREC reference number 2017-3020). Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- O’Connor TE, Perry CF, Lannigan FJ. Complications of otitis media in Indigenous and non-Indigenous children. Med J Aust 2009;191:S60-4. [PubMed]
- O’Leary SJ, Triolo RD. Surgery for otitis media among Indigenous Australians. Med J Aust 2009;191:S65-8. [PubMed]
- Coates H. Chronic suppurative otitis media in indigenous populations: the Australian aborigine. Ear Nose Throat J 2002;81:11-2. [PubMed]
- Guerin N, McConnell F. Myringoplasty: a post-operative survey of 90 aborigine patients. Rev Laryngol Otol Rhinol (Bord) 1988;109:123-7. [PubMed]
- Foreman A, Vercoe G, Aithal V. The Aboriginal Ear Health Program (1995-97) in the Northern Territory: Myringoplasties. J Otolaryngol Soc Aust 1999;3:235.
- Nienhuys TG, Boswell JB, Vercoe G. Hearing benefits from tympanoplasty in four Aboriginal adolescents. Aust J Otolaryngol 1996;2:267-71.
- Mak DB, MacKendrick A, Bulsara MK, et al. Long-term outcomes of middle-ear surgery in Aboriginal children. Med J Aust 2003;179:324-5. [PubMed]
- Mak D, MacKendrick A, Bulsara M, et al. Outcomes of myringoplasty in Australian Aboriginal children and factors associated with success: a prospective case series. Clin Otolaryngol Allied Sci 2004;29:606-11. [Crossref] [PubMed]
- Mackendrick A. Ear surgery in Australian Aboriginal children--is it indicated and when is the best time? J Otolaryngol Soc Aust 1999;3:240.
- Tos M. Cartilage tympanoplasty. 1st edition. Stuttgart: Thieme, 2009.
- Celik H, Samim E, Oztuna D. Endoscopic "Push-Trough" Technique Cartilage Myringoplasty in Anterior Tympanic Membrane Perforations. Clin Exp Otorhinolaryngol 2015;8:224-9. [Crossref] [PubMed]
- Simsek E, Ozkan O, Kucur C, et al. Evaluation of the anatomical and auditory outcomes of minimally invasive cartilage myringoplasty: Our technique and experience. Am J Otolaryngol 2016;37:517-22. [Crossref] [PubMed]
- Tseng CC, Lai MT, Wu CC, et al. Endoscopic Transcanal Myringoplasty for Anterior Perforations of the Tympanic Membrane. JAMA Otolaryngol Head Neck Surg 2016;142:1088-93. [Crossref] [PubMed]
- Tseng CC, Lai MT, Wu CC, et al. Endoscopic transcanal myringoplasty for tympanic perforations: An outpatient minimally invasive procedure. Auris Nasus Larynx 2018;45:433-9. [Crossref] [PubMed]
- Tseng CC, Lai MT, Wu CC, et al. Comparison of endoscopic transcanal myringoplasty and endoscopic type I tympanoplasty in repairing medium-sized tympanic perforations. Auris Nasus Larynx 2017;44:672-7. [Crossref] [PubMed]
- James AL. Endoscope or microscope-guided pediatric tympanoplasty? Comparison of grafting technique and outcome. Laryngoscope 2017;127:2659-64. [Crossref] [PubMed]
- Halim A, Borgstein J. Pediatric myringoplasty: postaural versus transmeatal approach. Int J Pediatr Otorhinolaryngol 2009;73:1580-3. [Crossref] [PubMed]
- Jassar P, Sibtain A, Marco D, et al. Infection rates after tympanostomy tube insertion, comparing Aboriginal and non-Aboriginal children in the Northern Territory, Australia: a retrospective, comparative study. J Laryngol Otol 2009;123:497-501. [Crossref] [PubMed]
- Jervis-Bardy J, Sanchez L, Carney AS. Otitis media in Indigenous Australian children: review of epidemiology and risk factors. J Laryngol Otol 2014;128:S16-27. [Crossref] [PubMed]
- Yung M. Cartilage tympanoplasty: literature review. J Laryngol Otol 2008;122:663-72. [Crossref] [PubMed]
- Klacansky J. Cartilage myringoplasty. Laryngoscope 2009;119:2175-7. [Crossref] [PubMed]
- Khan MM, Parab SR. Primary cartilage tympanoplasty: our technique and results. Am J Otolaryngol 2011;32:381-7. [Crossref] [PubMed]
- Gunasekera H, Morris PS, Daniels J, et al. Otitis media in Aboriginal children: the discordance between burden of illness and access to services in rural/remote and urban Australia. J Paediatr Child Health 2009;45:425-30. [Crossref] [PubMed]
Cite this article as: Loh TL, Ranguis S, Patel H, Crossland G. Permeatal ‘push through’ myringoplasty in the Northern Territory: a prospective cohort. Aust J Otolaryngol 2018;1:22.


