Harmonic scalpel versus other techniques for tonsillectomy: a systematic review and meta-analysis
Introduction
Tonsillectomy is one of the most common surgical procedures performed. It is a procedure to remove the palatine tonsils by dissection in the peritonsillar space. It is commonly performed for recurrent tonsillitis as well as adenotonsillar hypertrophy causing sleep-disordered breathing, and for other less common indications such as asymmetry or tonsilloliths. The procedure is performed in both adults and children. There are multiple techniques used in current practice. These techniques are variable and have been refined over the years. Some of the common techniques include electrocautery with monopolar or bipolar diathermy, blunt dissection (cold steel dissection), plasma-mediated radiofrequency-based ablation (coblation), and ultrasonic dissection. These techniques are often categorised into hot or cold. Hot techniques utilise instrumentation that employs heat to coagulate and dissect tissues via different methods, such as electrocautery, radiofrequency, or ultrasonic vibration. The “cold” technique refers to removal of the tonsil using traditional metal surgical instruments (scalpel, scissors, and dissecting forceps). Haemostasis is achieved by applying pressure using a gauze swab to the tonsillar fossa, heat using electrocautery or coblation, or ligatures or vessel ties. Though studies have shown positive results with the use of different surgical techniques, there is limited evidence with regards to controlled trials comparing specific techniques. In addition, there is no consensus in the literature for the recommended technique. Though a commonly-performed procedure, tonsillectomy is also associated with morbidity—mainly postoperative pain and bleeding. Bleeding can occur intraoperatively and during the immediate postoperative period, or more than 24 hours post-procedure (i.e., secondary haemorrhage).
Ultrasonic scalpel tonsillectomy is one of the more recent techniques described in the literature. The harmonic scalpel is a handheld device founded in 1992, which uses ultrasonic energy at the blade tip. The vibrations at the tip allow the blade to cut and coagulate tissue simultaneously. The theoretical advantage is that the harm is reduced with the harmonic scalpel because of lower temperature heat (50–100 degrees Celsius) compared to standard electrocautery (400 to 6,000 degrees Celsius).
Comparison of the different surgical techniques are important as they may hypothetically impact the patient’s postoperative recovery. The aim of this systematic review is to identify randomised controlled trials comparing harmonic (ultrasonic) scalpel to alternative standard techniques in both the paediatric and adult population undergoing tonsillectomy looking at postoperative pain, intraoperative blood loss, and rates of secondary haemorrhage. This review will only evaluate studies describing tonsillectomy, where the entire palatine tonsil is removed extra-capsularly leaving bare pharyngeal musculature at the base. This differs from tonsillotomy, where a rim of tonsillar tissue is left behind. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/ajo.2019.01.03).
Methods
The protocol for this systematic review was registered with PROSPERO, the international prospective register of systematic reviews (CRD42017081802). PRISMA statement guidelines were followed.
Searching
Randomised controlled trials were identified through Medline, Embase and the Cochrane Central Registry of Randomised Controlled Trials using optimally-sensitive search strategies as per the Cochrane Handbook for Systematic Reviews of Interventions (1).
Trials were considered without language restriction. Titles and abstracts from the search results were analysed, and appropriate trials identified according to the inclusion criteria. Medical subject heading terms and text words used were: tonsillectomy, tonsillitis, palatine tonsil, adenotonsillectomy, surgical procedures, harmonic scalpel, ultrasonic scalpel, and bipolar diathermy. Search strategies for major databases are provided in Table S1.
Reference lists were also searched and information sought from a clinical expert. Additional trials were searched from the internet.
Selection
Randomised controlled trials (RCTs) where the patient was the unit of randomisation were included. Trials where tonsils were randomised were excluded. Conference abstracts were excluded. The morbidity from concurrent adenoidectomy or ventilation tube insertion was considered to be much less than tonsillectomy alone, and thus trials that described concurrent procedures of this nature were not excluded for analysis. Trials that performed tonsillectomy for retropharyngeal or peritonsillar abscess, or concurrent to other procedures (such as endoscopic sinus surgery or palatoplasty) were excluded. When outcomes were expected to differ due to having a concurrent procedure versus tonsillectomy only, then subgroup analysis was planned.
Intervention & study characteristics
The intervention of interest in this review was harmonic scalpel tonsillectomy (a surgical device that uses ultrasonic vibrations rather than an electric current to cut and cauterise tissues).
The main comparator was electrocautery, specifically bipolar diathermy. Other comparators included other hot techniques (such as coblation and monopolar diathermy) and traditional ‘cold’ technique (“blunt dissection” or “cold steel”) tonsillectomy. The study design for included trials were parallel randomised controlled trials.
Participants were adults or children undergoing elective tonsillectomy for recurrent tonsillitis or sleep-disordered breathing. Where possible, trials were separated based on participants (paediatric only, adult only, or mixed population).
The primary outcome analysed in this review was postoperative pain as measured using a validated pain scale at 1, 4 and 7 days. Secondary outcomes included measure of intraoperative blood loss (mL) and presence of delayed postoperative bleeding (>24 hours from surgery). Clinical heterogeneity was assessed by comparing differences in trial participant characteristics (sex, age), intervention characteristics (setting of harmonic scalpel and bipolar diathermy where described, level of experience of proceduralist), and timing and method of outcome measurement (i.e., how pain scores were assessed, type of validated pain scale used). Thus, pre-planned subgroup analysis was performed to address heterogeneity, stratifying for similar characteristics of the intervention (i.e., grouped by hot or cold techniques).
Validity assessment
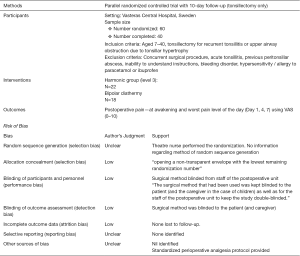
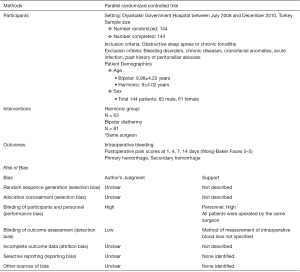
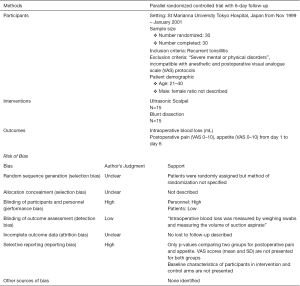
The quality of the trials identified was assessed based on pre-determined criteria, such as risk of bias (allocation concealment, random sequence generation, blinding), loss to follow-up, and intention-to-treat analysis.
Studies were assessed for risk of bias as “low”, “high”, or “unclear” using the Cochrane Handbook. Bias was assessed in: sequence generation, allocation measurement, blinding, incomplete data, selective reporting, and other sources of bias.
Data extraction
Authors extracted data from each study using a standardised collection form (see Figures S1-S11). Data extracted included: study design, study setting, patient inclusion and exclusion criteria, allocation concealment, blinding, number of participants in each group, surgical technique of each group, outcomes collected, and follow-up. The main outcome of interest was pain scores postoperative day 1, 4, and 7 (and where available, day 14 postoperative). These dates were chosen a priori. Day 1 postoperatively was expected to be a consistently collected outcome in terms of time-point from surgery. The assessment of pain at one week postoperatively is a clinically relevant time-point. The authors felt that day 4 postoperative would be a reasonable middle point to assess pain scores between day 1 and day 7. The postoperative pain scale used by the trial was also noted.
Data with respect to secondary outcomes of interest were also collected. This included mean intraoperative blood loss for each group in the trial (including method of assessment), as well as rates of delayed post-operative haemorrhage (i.e., secondary haemorrhage defined as more than 24 hours post operatively). These are consistently collected outcomes collected in tonsillectomy trials.
Where possible, the authors also collected information that may be relevant for subgroup analysis with respect to the outcomes of interest. For example, this would include information regarding the study population (paediatric and adult, paediatric only, or adult only population), whether or not there was a pre-defined perioperative analgesia protocol, and whether patients underwent tonsillectomy alone or with concurrent procedures.
Because surgical indication does not determine the choice of technique used, subgroup analysis based on clinical indication was not performed. Subgroup analysis was performed based on category of technique as hot (coblation, monopolar, bipolar diathermy, ultrasonic scalpel) versus cold (blunt dissection).
Quantitative data synthesis and statistical analysis
Treatment results were pooled across studies where the data was available. Treatment differences for dichotomous outcomes (i.e., secondary haemorrhage) were expressed as risk ratio (RR) with 95% confidence interval. Treatment effects for continuous outcome measures, such as postoperative pain score, were expressed as standardised mean difference (SMD) with 95% confidence intervals to reflect differences in pain scales used. Continuous data was pooled using inverse variance method. Pooled data for dichotomous outcomes was analysed using the Mantel-Haenszel method to calculate RR. Mean difference (MD) was used where the unit of the outcome measure was consistent (i.e., mL for intraoperative blood loss). Random-effects meta-analysis method (DerSimonian and Laird) was used for most outcomes to account for differences in patient populations, institutions, surgical techniques, and surgeon experience. Given that statistical heterogeneity was expected to be high, a random-effects method would provide a more conservative estimate.
In studies where the P value was reported for the comparison of means between intervention and control groups but the standard deviation was not presented in the study, the estimated standard deviations for each group were calculated. The reported P value was converted to a t-value based on number of participants in each group (i.e., degrees of freedom). The t-value was converted to a standard error by dividing the difference in means by the t-value. The average standard deviations of the groups were calculated using the formula: standard deviation = standard error/square root [(1/Nintervention) + (1/Ncontrol)]
Statistical heterogeneity between studies was assessed using I2 statistic and Chi2 statistic (P<0.10 considered significant). I2 values greater than 50% suggested substantial percentage of variability secondary to heterogeneity rather than due to chance. Forest plots were also inspected. Clinical heterogeneity was assessed by considering differences in study population, intervention, and outcomes. When heterogeneity was not significant, summary estimates for the intervention were presented with 95% confidence intervals.
It was determined a-priori that causes for differences in the main outcome of interest (postoperative pain) would include: age of the study population (paediatric, adult, or mixed population), presence or absence of a standardised perioperative analgesia protocol, and whether or not a concurrent procedure was performed. Subgroup analysis were planned around these factors. All meta-analyses were performed using Review Manager 5.3 jeny (2).
Results
Trial flow
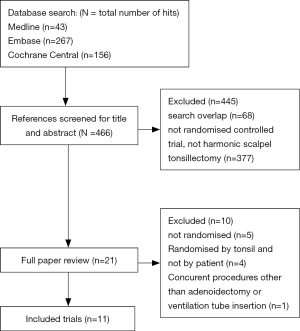
Of the 466 articles identified, 445 were excluded after review of the abstract and title. Major reasons for exclusion included: non-randomised controlled trial, duplicate publications, or not involving the intervention of interest. After assessing the full text of 21 studies, a total of 11 eligible randomised controlled trials were identified (see Figure 1 for flow diagram). Four randomised controlled trials were excluded, where the unit of randomisation was by tonsil (3-6).
Study characteristics
Characteristics of the individual trials included for analysis are listed in Figures S1-S11. A summary table of the included trials can be found in Table 1.
Table 1
| Study characteristics (study, year, country) | Study period | Design | Follow-up (days) | Participants (total number) | Age, years (range) | Intervention (concurrent operation) | Intervention | Control | Perioperative analgesia protocol | Pain scale |
|---|---|---|---|---|---|---|---|---|---|---|
| Ultrasonic scalpel versus hot techniques | ||||||||||
| Arbin 2017, Sweden | – | RCT | 7 | 40 | 7–40 | No | Harmonic scalpel (level 3) | Bipolar diathermy (16 W) | Described | VAS, 0–10 |
| Kemal 2012, Turkey | 2008–2011 | RCT | 14 | 144 | 4–18 | Adenoidectomy | Harmonic scalpel (level 2) | Bipolar diathermy (25 W) | Not described | WBF, 0–5 |
| Leaper 2006, New Zealand | – | RCT | 13 | 204 | 6–15 | No | Harmonic scalpel (level 2) | Bipolar diathermy (15 W) | Described | VAS, 0–10 |
| Parsons 2006, USA | 2002–2004 | RCT | 10 | 134 | 2–42 | Adenoidectomy | Harmonic scalpel | Monopolar diathermy, coblation | Not standardized | WBF, 0–10 |
| Ragab 2012, Egypt | 2005–2011 | RCT | 21 | 300 | 18–54 | No | Harmonic scalpel | Bipolar diathermy (30 W), Coblation, Cold steel | Described | VAS, 0–10 |
| Willging 2003, USA | – | RCT | 14 | 117 | 3–18 | Adenoidectomy, MEVTs | Harmonic scalpel (level 3) | Electrocautery (10–15 W) | Not standardized | WBF, 0–5 |
| Ali 2011, Pakistan | 2006–2008 | RCT | 7 | 60 | 18–68 | No | Harmonic scalpel | Electrocautery | Described | VAS, 0–10 |
| Ultrasonic scalpel versus cold techniques | ||||||||||
| Kamal 2005, UK | 2003–2004 | RCT | 7 | 280 | 3–69 | Adenoidectomy | Harmonic scalpel (level 2) | Cold steel | Not standardized | Grade 1–6 |
| Oko 2004, UK | – | RCT | 9 | 122 | 5–13 | No | Harmonic scalpel (level 2–3) | Cold steel | Described | WBF, 0–3 |
| Salomone 2007, Brazil | 2005–2006 | RCT | 5 | 100 | 3–10 | Adenoidectomy | Harmonic scalpel (level 2) | Cold steel | Described | VAS, 1–7 |
| Sugiura 2002, Japan | 1999–2001 | RCT | 6 | 30 | 21–40 | No | Harmonic scalpel (level 3) | Cold steel | Not described | VAS, 0–10 |
MEVT, middle ear ventilation tubes; VAS, visual analogue scale; WBF, Wong-Baker faces scale.
All studies were parallel design, single-blinded randomised controlled trials. Follow-up ranged from 5 to 21 days post-tonsillectomy, with mean of 10 days. Sample sizes ranged from 30 to 300 participants.
Participants
Most of the studies included participants undergoing tonsillectomy for tonsillitis, tonsillar hypertrophy, or both. Trials could be broadly categorised by age of participants as follows:
- Five trials focused on paediatric and adolescent population only (7-11).
- Three trials included mixed population of adult and paediatric patients (12-14).
- Three trials included an adult population only (15-17).
Intervention
All included trials evaluated the effects of the harmonic scalpel. Where specified, the setting used ranged between level 2 and 3. A variety of alternative techniques were used as control. Five studies compared harmonic scalpel to bipolar or monopolar electrocautery. Four studies compared harmonic scalpel to cold steel tonsillectomy. Parsons et al. compared harmonic scalpel tonsillectomy to monopolar diathermy and coblation techniques (14). Ragab conducted a multi-arm parallel trial with bipolar diathermy, coblation, and cold steel technique as comparators (16).
We classified alternative techniques into either “hot” or “cold”. “Cold” comparison techniques included trials that performed tonsillectomy by traditional surgical dissection (“cold steel”), with haemostasis achieved by bipolar diathermy and ties. Adenoidectomy was performed in conjunction with tonsillectomy in at least some patients for five trials (7,10,11,13,14).
Quantitative data synthesis
There was significant heterogeneity among trials in terms of the scale utilised for postoperative pain measurement. Some studies included children undergoing concurrent surgery (i.e., adenoidectomy or myringotomy and ventilation tube insertion) while others did not.
Many studies contained unclear methodology or reported insufficient data. Studies where there was insufficient data to permit calculation of standard deviation were excluded from meta-analysis. Attempt was made to contact study authors where possible to obtain critical data for meta-analysis.
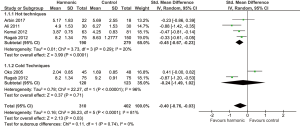
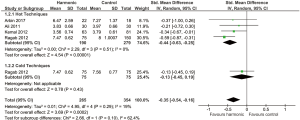
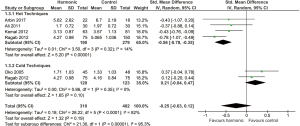
Postoperative pain
Many studies utilised previously validated pain scales, such as the Wong Baker FACES (WBF) scale (7,9,11,14) or the visual analogue scale (VAS) (8,10,12,15-17). However, several studies adapted or abbreviated the scales by changing the numeric reference points. These adapted pain scales may have invalidated them. For example, some studies changed the Wong Baker FACES (WBF) scale to 0 to 5 (7,11) or 0 to 3 (9) rather than 0 to 10. Similarly, one study changed the anchor points of the VAS to 1 to 7 (10). Kamal et al. utilised a pain assessment grading system for level of pain, ranging from no pain to very severe, in association with frequency of analgesia intake (grade 1 to 6) (13). Pain scores were compared based on a validated pain scale. It was determined a-priori that pain scores would be compared using validated pain scales only. The decision was made to also include studies that used VAS or WBF scale regardless of the anchor points assigned.
Five trials presented studies on postoperative pain at discrete time points either using VAS or WBF (7,9,12,15,16). Where possible, trial results were pooled to reflect postoperative pain scores at day 1, day 4, and day 7 postoperatively.
Some studies measured postoperative pain scores using a validated scale but presented the data in a way that did not allow for meta-analysis. For example, some trials presented insufficient amount of data (9-11,13,17) or reported an average pain score over several days. Leaper et al. (8) calculated the mean pain scores over 6 days postoperatively, rather than presenting mean scores at discrete time points. Similarly, Parsons presented mean pain scores over the 10-day period (14).
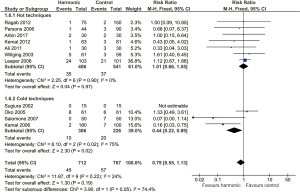
Five trials had sufficient data to be pooled for postoperative pain scores (see Figures 2-4). In comparison to hot techniques, harmonic scalpel tonsillectomy showed significant reduction in pain scores on day 1 (standard mean difference −0.45, 95% CI: −0.67 to −0.23, P<0.001), day 4 (SMD −0.44, 95% CI: −0.63 to −0.25, P<0.001), and day 7 (SMD −0.56, 95% CI: −0.78 to −0.35, P<0.001) in comparison to control. There was no statistically significant different in pain scores for harmonic tonsillectomy compared to cold steel, however there were insufficient studies with appropriate methodology in this subgroup to allow for meaningful pooled analysis.
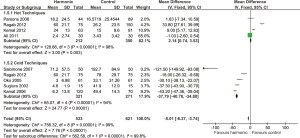
Intraoperative blood loss
A total of 8 studies reported intraoperative blood loss as an outcome (see Figure 5). The majority of studies measured intraoperative blood loss either through volume of blood aspirated in the suction bottle or by weight of tonsil swabs (9,10,13,15-17). The method of estimation was not described in two studies (7,14). Importantly, studies that included patients who underwent concurrent adenoidectomy as well as tonsillectomy did not specify the amount of blood loss related to the former procedure, and no information as to whether blood loss was measured separately for tonsillectomy versus adenoidectomy.
Intraoperative blood loss was less in alternative hot techniques versus harmonic scalpel (mean difference 2.14 mL, 95% CI: 0.74–3.53, P=0.003). But in comparison to cold steel tonsillectomy, harmonic scalpel was associated with less blood loss (mean difference −37.79, 95% CI: −40.78 to −34.80, P<0.001). Overall, harmonic scalpel was favourable in comparison to all other techniques (mean difference −5.01, 95% CI: −6.27 to −3.74, P<0.001), but there was extreme statistical heterogeneity (I2 =99%). The quality of the evidence in this outcome is considered to be low quality due to heterogeneity in methodology. None of the studies included separate measurements for blood loss in patients who underwent concurrent adenoidectomy. No comment was made in association with subtraction of saline irrigant from the reported blood loss.
Delayed bleeding
Delayed bleeding was defined as the incidence of bleeding more than 24 hours post-surgery. A total of eleven trials contributed data to this secondary outcome (see Figure 6) (7-17).
There was no statistically significant difference in delayed bleeding compared to other hot techniques (RR 1.01, 95% CI: 0.66 to 1.55, P=0.97). Whereas there was a significantly lower risk of delayed bleeding in harmonic scalpel versus cold steel (RR 0.44, 95% CI: 0.22 to 0.89, P=0.02).
Risk of bias
A summary of the risk of bias can be found in Table 2. The assessment of each of the trials can be found in the Characteristics of Included Studies.
Table 2
| Validity measure | Number of studies (%) |
|---|---|
| Randomisation method described | |
| Yes | 3 (27.3) |
| No | 8 (72.7) |
| Allocation concealment | |
| Adequate | 2 (18.2) |
| Unclear | 7 (63.6) |
| Inadequate | 2 (18.2) |
| Blinding | |
| Participants | 11 (100.0) |
| Investigators | 4 (36.4) |
| Loss to follow-up (Attrition bias) | |
| High risk | 2 (18.2) |
| Low risk | 4 (36.4) |
| Unclear | 5 (45.5) |
Allocation
Studies that did not adequately describe the method of randomisation were considered to have unclear risk for selection bias.
Blinding
Risk of performance and detection bias for each study was based on this review’s primary outcome of postoperative pain. Inability to blind operative personnel for the detection of postoperative pain was not expected to cause significant detection bias, since it is a patient-reported outcome. However, this would be a cause for potential detection bias in assessing intraoperative blood loss and delayed haemorrhage.
Blinding of personnel was not often mentioned in the methodology of the included studies. In some studies, all procedures were performed by a single surgeon. No study described any steps to address possible surgeon bias. Many studies also did not report blinding of the team involved in the postoperative care. As a result, performance bias was considered high for several studies. Detection bias was high for outcomes assessed by surgical personnel such as postoperative haemorrhage and volume of intraoperative blood loss. Given patients were blinded, detection bias was low for patient-reported outcomes (pain).
Incomplete outcome data
Studies were considered to have high risk of attrition bias with an attrition rate greater than 10%. Studies had an unclear risk if they did not report attrition rates or if there was insufficient information to determine this.
Selective reporting
There were no study protocols available to compare between planned and reported outcomes. Thus, all studies were judged as unclear risk of reporting bias unless studies did not report results for outcomes stated in the methods section.
Discussion
Summary of key findings
This review found low quality evidence that harmonic tonsillectomy may be associated with less pain postoperatively on day 1, day 4 and day 7 in comparison to other hot techniques. The magnitude of this difference was not clinically significant.
In comparison to other hot techniques harmonic scalpel was associated with higher intraoperative blood loss (mean difference 2.14, 95% CI: 0.74 to 3.53, P=0.003), but less in comparison to cold techniques (mean difference −37.97, 95% CI: −40.78 to −34.80, P<0.001). Results from meta-analysis for intraoperative blood loss was associated with extreme statistical heterogeneity (I2 =98% for hot techniques, 94% for cold techniques).
There was no statistically significant difference in rates of delayed bleeding compared to other hot techniques (RR 1.01, 95% CI: 0.66 to 1.55, P=0.97). Notably, harmonic scalpel was associated with lower rates of delayed bleeding compared to cold techniques (RR 0.44, 95% CI: 0.22 to 0.89, P=0.02; 4 studies; 532 participants; I2 =75%).
Clinical interpretation
Theoretically, the use of harmonic scalpel should be associated with decreased levels of pain in comparison to other hot techniques. The use of ultrasound allows for comparatively lower temperatures to coagulate and dissect tissues. Another benefit is that no electrical energy is transferred to the tissue with the harmonic scalpel technique. As a result, lower temperatures should also be associated with less volume of tissue damage intraoperatively. Less thermal damage in the operative field also implicates better postoperative healing. While considering the high level of clinical heterogeneity for the included trials, this review has shown the harmonic scalpel to be marginally associated with lower levels of pain postoperatively.
Intraoperative blood loss is dependent on many factors apart from the instrument used to perform the procedure. For example, the speed of surgery and experience or technique of the operating surgeon are all potential confounding factors that affect interpretability of results.
Strengths and limitations of the study
Although a total of 11 studies were included in this review, most did not report data in a way that allowed for meta-analysis. Where possible, data was pooled for planned subgroup analysis. However, a variety of data-reporting problems limited analysis. For example, some studies did not provide measures of variance (standard deviation) for intraoperative blood loss and postoperative pain scores. Other studies reported only P values for postoperative pain score comparisons, but no mean or standard deviation. Sugiura et al. reported pain scores graphically, but exact values could not be derived for meta-analysis (17).
Although subgroup analysis was also planned based on age of participants (children versus adults) and type of surgery (i.e., if concurrent adenoidectomy versus tonsillectomy alone), there was insufficient study data available to conduct these analyses in a meaningful way. The studies also did not report data that allowed separation of outcomes into these subgroups, for example in trials that had mixed patient populations and where concurrent adenoidectomy was performed. Only subgroup analysis based on type of surgical technique (hot versus cold techniques) could be performed. In addition, standard mean difference in pain scores was used because of non-standardised pain outcomes reported in the trials. This has implications for interpretability of results in trials where adult and paediatric populations were combined.
Sensitivity analysis was not performed because the risk of bias was either high or unclear for all outcomes. No meaningful sensitivity analysis could have been conducted because of insufficient studies with low risk of bias.
This review is comprehensive in its inclusion of studies with all types of comparator techniques for tonsillectomy. The studies involved relevant patient populations undergoing tonsillectomy for chronic infection and sleep-disordered breathing. The included studies evaluated clinically important outcomes, such as postoperative pain, intraoperative bleeding, and postoperative bleeding.
The results of this systematic review are limited due to low quality of the studies included. This precludes robust conclusions to be made from the available evidence.
Applicability of findings
Several methodological limitations of the included studies preclude applicability of the findings from this review. Several of the studies failed to describe method of randomisation. Other key methodological issues include: inability to blind the operating surgeon and other personnel in the trial, difficulty blinding outcome assessors reporting intraoperative blood loss and postoperative bleeding. Postoperative pain scores were inconsistently measured on different pain scales. The method for measuring intraoperative blood loss differed between included trials and failed to be mentioned in the methods for others.
Both harm (rates of postoperative bleeding, intraoperative blood loss) as well as benefits (decreased postoperative pain) were evaluated in this review for harmonic tonsillectomy. Variations in treatment effect could only be investigated through subgroup analysis for surgical technique. The results of this review reveal that the harmonic scalpel is comparable in terms of risk of delayed bleeding in comparison to other hot techniques and does show benefit over cold techniques. The number needed to treat with harmonic tonsillectomy to prevent one case of delayed bleeding from cold steel tonsillectomy is 18 (absolute risk reduction 0.06).
Comparison to previous works & future research directions
No systematic review has been conducted previously comparing harmonic scalpel tonsillectomy to alternative techniques. One protocol was found on the Cochrane Library for harmonic scalpel versus other surgical procedures for tonsillectomy (18). A similar systematic review was conducted for coblation versus other techniques for tonsillectomy (19). Thus, the results of this review have provided a comprehensive summary for the current body of evidence, where previous non-randomised prospective and retrospective studies have shown varying results comparing harmonic tonsillectomy to alternative techniques.
Given that the quality of current trials are low, further randomised control trials are required. Future studies should report outcomes using CONSORT guidelines for more consistent reporting of outcomes. This would also allow adequate data extraction to update this review. Bias must also be minimised in future trials by standardising outcome measures. A significant reason for clinical heterogeneity was the lack of consensus in reporting outcomes, especially with regards to timing and methodology. As demonstrated in this review, there were major limitations in the measurement of postoperative pain—future trials should have standardised and specific, relevant time points for this outcome measure (either as an average over time or on certain postoperative days).
Conclusions
The harmonic scalpel technique may cause less pain in the postoperative period compared to other techniques, but the difference is small and clinically irrelevant. This statistically significant difference in pain scores compared to standard techniques was observed on day 1 and day 4 postoperatively. This technique may be associated with less intraoperative blood loss, however there was significant statistical heterogeneity among included studies pooled for meta-analysis (I2 =99%). The harmonic scalpel does demonstrate evidence for superiority compared to blunt dissection (“cold steel” technique), with a 56% in reduction in delayed haemorrhage. However, there is insufficient evidence to recommend the use of harmonic scalpel over other hot techniques.
Table S1
| Central |
Acknowledgments
Presented at Australasian Society of Otolaryngology Head and Neck Surgery (ASOHNS) Annual Scientific Meeting, Perth, Australia. 9–11 March 2018.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/ajo.2019.01.03
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2019.01.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cochrane Hanbook for Systematic Reviews of Interventions. In: Higgins J, Green S, editors. The Cochrane Collaboration; 2011. Available online: www.cochrane-handbook.org.
- Review Manager (RevMan) [computer program]. Version 5.3. The Nordic Cochrane Centre: The Cochrane Collaboration; 2014.
- Akural EI, Koivunen PT, Teppo H, et al. Post-tonsillectomy pain: a prospective, randomised and double-blinded study to compare an ultrasonically activated scalpel technique with the blunt dissection technique. Anaesthesia 2001;56:1045-50. [Crossref] [PubMed]
- Collison PJ, Weiner R. Harmonic scalpel versus conventional tonsillectomy: a double-blind clinical trial. Ear Nose Throat J 2004;83:707-10. [PubMed]
- Cushing SL, Smith O, Chiodo A, et al. Evaluating postoperative pain in monopolar cautery versus harmonic scalpel tonsillectomy. Otolaryngol Head Neck Surg 2009;141:710-5.e1. [Crossref] [PubMed]
- Sheahan P, Miller I, Colreavy M, et al. The ultrasonically activated scalpel versus bipolar diathermy for tonsillectomy: a prospective, randomized trial. Clin Otolaryngol Allied Sci 2004;29:530-4. [Crossref] [PubMed]
- Kemal O. Harmonic scalpel versus bipolar tonsillectomy: a double-blind clinical trial. Eur Arch Otorhinolaryngol 2012;269:1533-6. [Crossref] [PubMed]
- Leaper M, Mahadevan M, Vokes D, et al. A prospective randomised single blinded study comparing harmonic scalpel tonsillectomy with bipolar tonsillectomy. Int J Pediatr Otorhinolaryngol 2006;70:1389-96. [Crossref] [PubMed]
- Oko MO, Ganly I, Loughran S, et al. A prospective randomized single-blind trial comparing ultrasonic scalpel tonsillectomy with tonsillectomy by blunt dissection in a pediatric age group. Otolaryngol Head Neck Surg 2005;133:579-84. [Crossref] [PubMed]
- Salomone R, Visioli A, Aquino M, et al. Ultrasonic Curved Shears in Tonsillectomy: Comparative Clinical Trial Between this New Surgical Technique and the Technique with the Cold Blade Surgical Knife. Int Arch Otorhinolaryngol 2007;11.
- Willging JP, Wiatrak BJ. Harmonic scalpel tonsillectomy in children: a randomized prospective study. Otolaryngol Head Neck Surg 2003;128:318-25. [Crossref] [PubMed]
- Arbin L, Enlund M, Knutsson J. Post-tonsillectomy pain after using bipolar diathermy scissors or the harmonic scalpel: a randomised blinded study. Eur Arch Otorhinolaryngol 2017;274:2281-5. [Crossref] [PubMed]
- Kamal SA, Basu S, Kapoor L, et al. Harmonic scalpel tonsillectomy: a prospective study. Eur Arch Otorhinolaryngol 2006;263:449-54. [Crossref] [PubMed]
- Parsons SP, Cordes SR, Comer B. Comparison of posttonsillectomy pain using the ultrasonic scalpel, coblator, and electrocautery. Otolaryngol Head Neck Surg 2006;134:106-13. [Crossref] [PubMed]
- Ali NS, Ikram M, Akhtar S, et al. Harmonic scalpel versus electrocautery tonsillectomy: a comparative study in adult patients. J Pak Med Assoc 2011;61:256-9. [PubMed]
- Ragab SM. Six years of evidence-based adult dissection tonsillectomy with ultrasonic scalpel, bipolar electrocautery, bipolar radiofrequency or 'cold steel' dissection. J Laryngol Otol 2012;126:1056-62. [Crossref] [PubMed]
- Sugiura N, Ochi K, Komatsuzaki Y, et al. Postoperative pain in tonsillectomy: comparison of ultrasonic tonsillectomy versus blunt dissection tonsillectomy. ORL J Otorhinolaryngol Relat Spec 2002;64:339-42. [Crossref] [PubMed]
- Burton M, Doree C. Harmonic scalpel versus other surgical procedures for tonsillectomy. Cochrane Database Syst Rev 2004;CD004616.
- Pynnonen M, Brinkmeier JV, Thorne MC, et al. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev 2017;8:CD004619. [PubMed]
Cite this article as: Wong DJY, Paddle P. Harmonic scalpel versus other techniques for tonsillectomy: a systematic review and meta-analysis. Aust J Otolaryngol 2019;2:3.