
Uvulopalatopharyngoplasty: a specific surgical technique aimed at minimising patient morbidity, with outcomes over 5 years in a regional centre
Introduction
Uvulopalatopharyngoplasty (UPPP) is an operation performed for obstructive sleep apnoea (OSA) patients that aims to improve sleep quality, snoring and reduce obstructive events. It is considered a second line treatment of this disease, for which continuous positive airway pressure (CPAP) is the gold standard (1-3). However, CPAP compliance is variable and long-term utilisation ranges between 30% and 60% (4). CPAP is not tolerated in a significant number of patients due to device discomfort, psychological and social impacts of wearing a mask and being connected to a machine (5,6). Alternative therapeutic options including oral appliances, lifestyle interventions and surgical procedures should be advised when patients are unable to comply with CPAP, if it fails to improve their condition (2,7). There is a present evolution of the surgical approach to UPPP with multiple techniques described. Recent randomised and cohort studies show that UPPP can reduce the severity of OSA, decrease the number of obstructive events and apnoea hypopnoea index (AHI), decrease the pressure requirements of CPAP, and increase patients’ tolerance of CPAP (5,8,9). Importantly, surgical intervention is being shown to alter patients subjective experience of the disease, improving snoring, daytime sleepiness and quality of life (10-12), as well as cardiovascular outcomes and mortality (13). Quality of life outcomes studied in the literature on OSA surgery cover alertness, fatigue, mental health, daytime performance and productivity.
The UPPP is a relatively new procedure, being first described in 1981 (14) with an evolution in techniques occurring subsequently and there is currently no consensus regarding the most efficacious and appropriate technique. The variations have developed with the motive of reducing complications and improving airway outcomes (15). The overall concept is to reduce upper airway resistance by modifying the oropharyngeal airway. All oropharyngeal surgery carries with it a clinically significant level of post-operative pain, due to laceration of sensitive mucosa and mobile muscle. There are only 22 described surgical techniques of UPPP in the literature that have case series with analysed outcomes. Associated side effects with current techniques include post-operative pain which is almost universal but also acute and chronic dysphagia, velopharyngeal incompetence, voice change, taste change and long-term problems of nasopharyngeal stenosis and altered pharyngeal sensation (15-17).
The aim of this study was to investigate the patient acceptability and efficacy of a single surgeon cold steel technique that does not resect muscle of the soft palate, and preserves some uvula mucosa. We sought to evaluate the subjective patient experience with this technique. Specifically, the quality of life impact, including elements of their sleep quality, snoring, partner reported snoring and daytime symptoms. In addition, if patients considered these long-term benefits of surgery to outweigh the peri-operative morbidity, we wanted to ultimately ask, if the experience was overall worthwhile.
Methods
Study design
Ethics approval was obtained by the Albury Wodonga Human Research Ethics Committee (HREC reference number HREC/17/AWHEC/21), for a retrospective case series of a single surgeon’s outcomes with a specific technique of performing UPPP in the Albury Wodonga area. The patient service reports from our practice software of a single surgeon from January 1st 2012 to December 31st 2017 were screened for the UPPP Medicare service items on the 24th January 2018. Ninety-eight patient encounters were identified of adults (18 years and older) competent to consent. Clinical records from the private consulting rooms, public hospital and private hospital were used to collect patient information and outcomes. Prior to contacting patients, an information and consent sheet was mailed to all patients, explaining they will be contacted for voluntary phone interviews. Consent was confirmed verbally at the time of phone interview.
Setting
Albury Wodonga is a regional centre servicing a mixed urban and rural population of 250,000 people.
Phone interviews were conducted from June 2018 to January 2019. They were conducted by the one interviewer for consistency and as information was collected it was deidentified when entered into the dataset. The interview was structured including: confirmation of receipt of consent and information sheet, verbal consent then demographics including clarification of age, timing of procedure, sleep study results and comorbidities. Patients were then asked a series of questions and the Functional Outcome of Sleep Questionnaire 10 (FOSQ-10) on their experience of their disease before and after their UPPP, the recovery period and complications. All qualitative questions were graded on a global scale from one to four (one being no impact, two little, three moderate and four extreme), pain was graded from one to five (one being no pain, five being the worst pain imaginable). Patients were finally asked to answer only yes or no whether the procedure was overall worthwhile.
Variables
We collected information from the medical record on patient age, gender, comorbidities, timing of surgery, AHI pre and post-operative, previous airway surgery and additional indications. This was confirmed, and where necessary, deficiencies filled during the phone interview.
Outcome measures
Subjects were asked three specific questions about their experience of the impact of their disease: daytime symptoms including somnolence, sleep quality and the impact of their snoring on their partner. We asked patients to rate qualitatively their experience in each domain on a global scale from one to four currently (post operatively) and what they would have rated it pre operatively. This global scale from one to four was consistent with the quality of life tool we used which was the FOSQ-10. We collected information from the medical record of complications, clinician recorded improvement at 4–6 week follow up, days spent in hospital and days spent off work.
We chose to use an OSA-specific quality of life tool which has been validated in this research context (18). The FOSQ-10 is a short version of the FOSQ which is a thirty question long OSA-specific questionnaire designed to assess the impact of sleepiness on a patient’s functional status, by asking questions relating to specific activities of daily living. It has proven validity and reliability in clinical trials to assess quality of life as well as treatment outcomes, and has been used in similar studies (3,19,20). It produces a score of 0–20 with a higher score correlating to a greater quality of life.
Surgical technique
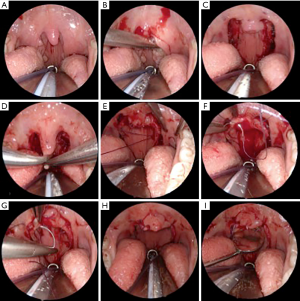
Involves initial cold steel dissection tonsillectomy when applicable with the modification of extending the component of peri-tonsillar mucosal resection by 5mm at the palatal margin and upper pillars. The uvula is then trimmed, resecting the lower third to half anteriorly and most of its length of mucosa posteriorly; usually a small element of mucosa of palatal margin remains intact on each side. Compared to other UPPP techniques, there is no dissection into mucosa of the soft palate or musculature of the palatopharyngeal arch at all. The tonsillar pillars are then closed with a series of mattress sutures with the first of these on each side passing antero-laterally to anchor in the mandibular gingival mucosa and submucosal tissues of the lateral soft palate. Relocation of the palatal margin anteriorly and the upper tonsillar pillars laterally is evident. Then the mucosal line of resection of the uvula is closed (still employing mattress sutures), creating a small mucosal neo-uvula. Usually the element of intact palatal mucosa is then seen stretched between the neo-uvula and the lateralised pharyngeal wall. The technique does not involve transecting muscle, minimising risk of palatal dysfunction and probably hastening post-operative healing, and the absence of cut mucosa at the palatal margin and anterior uvula should reduce the pain from oral intake. Creation of a neo-uvula may maintain a more natural distribution of nasal secretions into the pharynx, reducing post-surgical changes in pharyngeal sensation (Figure 1, see online Video 1).
Statistical methods
Data was analysed qualitatively and quantitatively using Microsoft® Excel® Version 12.0 (California, 2008). Student’s t-test was used to compare unpaired continuous variables, and the chi squared test to compare categorical variables.
Results
Ninety-eight patient encounters were returned from practice Medicare claims data as having had a UPPP with Dr Fogarty as their primary surgeon from January 1st 2012 to December 31st 2017. The patient sample consisted of mainly overweight middle-aged men with a mean age of 40 ranging from 19 to 72 years old (Table 1).
Table 1
| Variable | Incidence |
|---|---|
| Age, mean ± SD (range) | 40.0±11.8 (19–72) |
| Gender (male/female), n (%) | 71 (72.4)/27 (27.6) |
| Overweight, n (%) | 39 (39.9) |
| Airways disease, n (%) | 17 (17.3) |
| Cardiovascular disease, n (%) | 13 (13.2) |
| Smoker, n (%) | 13 (13.2) |
Less than half of patients had a pre-operative sleep study (38/98), most of whom were confirmed to have sleep apnoea (33/38), with a mean AHI of 26.5. Twenty-two patients had already tried CPAP and were intolerant (22.4%), three had tried a mandibular advancement splint (MAS). According to the pre-operative clinical assessment, 51.0% of patients had also had historical tonsillitis, and 15.3% had a background of already having nasal airway surgery including septoplasty, turbinoplasty or turbinate cautery (Table 2).
Table 2
| Variable | Frequency |
|---|---|
| Sleep Study, mean ± SD (range) | 26.5±29.6 (0–130) |
| Normal PSG, n (%) | 5 (5.1) |
| Mild OSA, n (%) | 11 (11.2) |
| Moderate OSA, n (%) | 14 (14.3) |
| Severe OSA, n (%) | 8 (8.2) |
| Failed CPAP, n (%) | 22 (22.4) |
| Failed MAS, n (%) | 3 (3.1) |
| Previous nasal airway surgery, n (%) | 15 (15.3) |
| Tonsillitis, n (%) | 50 (51.0) |
Not mutually exclusive.
Out of 98 subjects 51 were lost to follow up, but only two declined to participate so a total of 47 interviews were completed over the phone. There were no significant differences between the age (P=0.1225), gender (P=0.3533) or pre-operative AHI (P=0.1281) of those who participated in the study, compared to those who were lost to follow up. The follow up period at the time of phone interview ranged from 1 to 6 years.
Our surgical technique was associated with a low rate of complications. There were only two bleeds in the cohort of 98 and only one required surgical arrest (1.0%). There were four readmissions for pain management or dehydration (4.1%). Five patients reported (at post-operative intervals between 14 and 32 months) that they had an alteration of pharyngeal sensation including globus and altered swallow sensation.
Most patients described their experience of having a UPPP as overall ‘worth it’ (93.6%), only three patients thought otherwise. Only a third of patients described the post-operative pain to be the worst pain, rated as 5 out of 5 (16/47), leaving 66% of patients describing that the pain was at the most moderate and manageable (rated up to 4 out of 5). Out of the whole cohort, the largest group stayed in hospital only 1 night (40.3%), with a mean of 2.1 nights in hospital. Most patients took the recommended 14 days off work (51.2%), with a mean of 13.2 days lost from work (Table 3).
Table 3
| Outcomes | Range, frequency | Mean ± SD |
|---|---|---|
| Pain | 5 (n=16), 4 (n=14), 3 (n=11), 2 (n=3), 1 (n=3) | 3.8±1.2 |
| Days in hospital | 1–10 (n=67) | 2.1±1.5 |
| Days off work | 1–28 | 13.2±6.1 |
There was an improvement in the mean quality of life of patients post operatively, as measured by their FOSQ-10, from 16.5 (SD ±3) to 18.1 (SD ±1.7), the mean change was an increase in score by 2.3 points (SD ±2.7).
Forty-one had significant daytime somnolence pre-operatively (41/47), and out of these, 31 out of 47 rated their daytime symptoms as moderate or extreme. Daytime somnolence was reported to be improved post UPPP, with 50% of patients reporting no daytime somnolence post procedure (Table 4). All patients reported that their bed fellow was disturbed by their snoring pre-operatively, with more than half (54.3%) reporting that this was an extreme problem for them. Snoring was overall improved post-operatively, with 36.4% of partners now reporting no snoring and 34.1% reporting only little impact to their partner from snoring.
Table 4
| Outcome measure | Pre-operative, n (%) | Post-operative, n (%) | Mean change ± SD |
|---|---|---|---|
| Daytime symptoms | |||
| None | 6 (14.3) | 23 (54.8) | |
| Little | 8 (19) | 13 (31) | |
| Moderate | 22 (52.4) | 5 (11.9) | |
| Extreme | 6 (14.3) | 1 (2.4) | 1.02±1.06 |
| Sleep quality | |||
| No problem | 9 (21.4) | 30 (71.4) | |
| Little | 8 (19) | 7 (16.7) | |
| Moderate | 20 (47.6) | 5 (11.9) | |
| Extreme | 5 (11.9) | 0 | 1.15±0.97 |
| Partner rated snoring | |||
| None | 0 | 14 (34.1) | |
| Little | 1 (2.4) | 15 (36.6) | |
| Moderate | 18 (43.9) | 9 (22) | |
| Extreme | 22 (53.7) | 2 (4.9) | 1.5±0.96 |
Discussion
Patients were overall satisfied with our surgical technique, with almost all (93.6%) describing the experience as having been worthwhile. Our series had short hospital stays, with acceptable time off work and acceptable post-operative pain. There was an improvement in daytime symptoms, sleep quality and partner-reported snoring overall as well as quality of life as measured by an OSA specific tool, the FOSQ-10. Our mean change of +2.3 in FOSQ-10 is comparable to Weaver et al.’s series, who found a mean change of 2.7 at three months post UPPP (19). A randomised control trail of CPAP versus sham CPAP found a mean change of only +0.89 in FOSQ scores for OSA patients who used CPAP after 8 weeks (2). Quality of life improvements have been demonstrated in few other similar case series (11,21-23), which all used a subjective patient rated global scale to assess quality of life. Few papers have used a disease specific quality of life measure such as the FOSQ-10, which enables objective comparison between interventions.
We had a high rate of patient acceptability (93.6%) compared with other published series, where patient satisfaction ranges greatly from one data set in which only 39% of patients said they would have the procedure again due to the post-operative pain involved (21). But Browaldh et al. reported 78% were satisfied with the procedure with 88% having improved daytime symptoms (10). Only 34% of patients rated the pain as maximal being five out of five, with the remainder finding it to be moderate at the most. We believe this is consequent to the preservation of intact muscle and reduced mucosal incision lines. Sommer et al. also reported a similarly high rate of patient satisfaction using Pirsig’s technique (11) which also preserves the velopharyngeal musculature, similar to our technique (24). Less ablative UPPP techniques, such as described by Mantovani et al., have also shown to decrease snoring, daytime sleepiness and be associated with shorter post-operative pain durations (25).
The greatest effect we identified was on the impact of their snoring on their partner. Few papers have discussed the importance of socially unacceptable snoring on motivating patients to seek medical intervention for OSA (26). Recent analysis of CPAP adherence points to the importance of family and social support in disease management (6), and our study reflects this. One hundred percent of our questionnaire cohort reported that their snoring had some impact on their partner, and at least a fifth (22.4%) had already trailed and were unable to comply with CPAP.
Partner reported snoring was also an effective outcome of our intervention. All patients in our series described that their partner had some complaint about their snoring that disrupted their sleep, with all but one categorising this impact as moderate or extreme. Post UPPP, 70.7% of patients said their partner now had no or little compliant about their snoring at night. Eight patients were found to have no change in their quality of life as measured by the FOSQ-10, however, all of these patients reported significant reduction in the impact of their snoring on their partner.
Concern about snoring appeared to be the strongest motivating factor for patients pursing a surgical intervention. Patterns of preoperative symptomatology highlight the importance of the partner in the diagnosis and management of OSA in our unique cohort. In our series, patients reported a higher rate of partner sleep disruption by their snoring (100%), than personal sleep disruption (78.6%). Furthermore, 14.3% of patients denied having any daytime somnolence. Our population of patients considered their partners concerns about their snoring motivation enough to seek out surgical treatment; or that it was solely the partners concerns about OSA that brought them to medical attention. Recent research in OSA also highlights that partners play a significant role in diagnosis and management of OSA (27).
Our surgical technique was safe with no mortality, one post-operative haemorrhage requiring surgical arrest, and a low incidence of long-term pharyngeal disturbance. Though limited in reporting, the literature reflects a high incidence of post-operative swallowing complaints in patients undergoing UPPP. This includes non-specific symptoms including dysphagia, odynophagia, globus, voice change and mucous alteration which significantly impact patients’ quality of life. A systematic review found the incidence of persistent side effects to range from 42–62% with dysphagia being the most common (29–25%) (28). This is reflected in more recent case series of upper airway surgery for OSA, where the incidence of dysphagia at long term follow up was 19.8% (29) and up to 38% (17). Our technique recorded a significantly lower rate of all pharyngeal symptoms at 5.1%.
In our rural patient group we experienced a low rate of polysomnogram diagnosis of OSA, which certainly lent the study design towards a quality of life analysis. Our patient selection was mostly clinical and patient-symptom driven. The use of the polysomnogram in our clinical context is to identify patients at a high perioperative risk, and to further evaluate patients who appeared to have a poor clinical response to surgery. This is reflected in the high preoperative AHI of our patient series (mean of 26.5) and correlates with the limited improvement in AHI in the five patients who had both pre and post-operative sleep studies (mean improvement of 12.8 points).
One patient in our series scored a worse quality of life outcome post operatively, but interestingly they did describe that the overall surgical experience was worth it. This patient had tried and failed CPAP use on a significant AHI of 100, then had a septoplasty and UPPP. Subsequently a post-operative PSG demonstrated their need for ongoing CPAP. This illustrates the complex problems with CPAP adherence and patient motivation in seeking a personalised approach to the management of their OSA (4,6). All seven participants in the questionnaire who had significant sleep apnoea on post-operative PSG remarked that the surgical experience was worth it. It is documented in the literature that airway surgery has utility in facilitating better tolerance with CPAP devices (15). Furthermore, a recent cohort study of patients undergoing surgery for OSA found that a reduction in sleepiness scores, not OSA severity, was predictive of improvement in depression scores (30).
We acknowledge this surgical series is limited in case numbers. This prevented evaluating the trends that we observed in improved quality of life by statistical analysis. The retrospective design and questionnaire format may create inaccuracy in patient reporting of preoperative disease impacts and some patients were asked to recall their subjective experience up to 6 years prior. It was not possible to comment on the long-term impact of outcomes or sequelae of this technique as our follow up period ranged from 1 to 6 years. The authors are designing a prospective study.
Acknowledgments
We thank E Tweddle (Albury Wodonga Health) for her support in the editing of this manuscript. The authors thank V Kumar for editing the media and video content. The College of Nursing at the University of Illinois at Chicago provided us with a quality of life measure, the FOSQ-10 at no financial cost.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2020.03.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained by the Albury Wodonga Human Research Ethics Committee (HREC reference number HREC/17/AWHEC/21). Prior to contacting patients, an information and consent sheet was mailed to all patients, explaining they will be contacted for voluntary phone interviews. Consent was confirmed verbally at the time of phone interview.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep 2010;33:1396-407. [Crossref] [PubMed]
- Epstein LJ, Kristo D, Strollo PJ Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5:263-76. [Crossref] [PubMed]
- Weaver TE, Mancini C, Maislin G, et al. Continuous positive airway pressure treatment of sleepy patients with milder obstructive sleep apnea: results of the CPAP apnea trial north american program (CATNAP) randomized clinical trial. Am J Respir Crit Care Med 2012;186:677-83. [Crossref] [PubMed]
- Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res 2010;131:245-58. [PubMed]
- Chandrashekariah R, Shaman Z, Auckley D. Impact of upper airway surgery on CPAP complicance in difficult-to-manage obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 2008;134:926-30. [Crossref] [PubMed]
- Ward K, Hoare KJ, Gott M. What is known about the experience of using CPAP for OSA from the users’ perspective? A systematic integrative literature review. Sleep Med Rev 2014;18:357-66. [Crossref] [PubMed]
- Weaver EM. Judging sleep apnea surgery. Sleep Med Rev 2010;14:283-5. [Crossref] [PubMed]
- MacKay SG, Carney AS, Woods C, et al. Modified uvulopalatopharyngoplasty and coblation channelling of the tongue for obstructive sleep apnea: a multi-centre Australian trial. J Clin Sleep Med 2013;9:117-24. [Crossref] [PubMed]
- Robinson S, Chia M, Carney AS, et al. Upper airway reconstructive surgery long-term quality-of-life outcomes compared with CPAP for adult obstructive sleep apnea. Otolaryngol Head Neck Surg 2009;141:257-63. [Crossref] [PubMed]
- Browaldh N, Friberg D, Svanborg E, et al. 15-year efficacy of uvulopalatopharyngoplasty based on objective and subjective data. Acta Otolaryngol 2011;131:1303-10. [Crossref] [PubMed]
- Sommer UJ, Heiser C, Gahleitner C, et al. Tonsillectomy with uvulopalatopharyngoplasty in obstructive sleep apnea. Dtsch Arztebl Int 2016;113:1-8. [PubMed]
- MacKay SG, Weaver EM. Surgery for adult obstructive sleep apnoea. Med J Aust 2013;199:450-1. [Crossref] [PubMed]
- Marti S, Sampol G, Munoz X, et al. Mortality in severe sleep apnoea/hypopnoea syndrome patients: impact of treatment. Eur Respir J 2002;20:1511-8. [Crossref] [PubMed]
- Fujita S, Conway W, Zorick F, et al. Surgical correction of anatomic abnormalities in obstructive sleep apnoea syndrome: uvulopalatopharygoplasty. Otolaryngol Head Neck Surg 1981;89:923-34. [Crossref] [PubMed]
- MacKay SG, Chan L. Surgical approaches to obstructive sleep apnea. Sleep Med Clin 2016;11:331-41. [Crossref] [PubMed]
- Levring-Jäghagen E, Nilsson M, Isberg A. Persisting dysphagia after uvulopalatoplasty performed with steel scalpel. Laryngoscope 1999;109:86-90. [Crossref] [PubMed]
- Friberg D, Sundman J, Browaldh N. Long-term evaluation of satisfaction and side effects after modified uvulopalatopharyngoplasty. Laryngoscope 2020;130:263-8. [Crossref] [PubMed]
- Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the functional outcomes of sleep questionnaire. Sleep 2009;32:915-9. [Crossref] [PubMed]
- Weaver EM, Woodson BT, Yueh B, et al. Studying life effects & effectiveness of palatopharyngoplasty (SLEEP) study: subjective outcomes of isolated uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 2011;144:623-31. [Crossref] [PubMed]
- Smith MM, Peterson E, Yaremchuk KL. The role of tonsillectomy in adults with tonsillar hypertrophy and obstructive sleep apnea. Otolaryngol Head Neck Surg 2017;157:331-5. [Crossref] [PubMed]
- Hicklin LA, Tostevin P, Dasan S. Retrospective survey of long-term results and patient satisfaction with uvulopalatopharyngoplasty for snoring. J Laryngol Otol 2000;114:675-81. [Crossref] [PubMed]
- Dizdar D, Civelek S, Calis ZA, et al. Comparative analysis of lateral pharyngoplasty and uvulopalatopharyngoplasty techniques with polysomnography and epworth sleepiness scales. J Craniofac Surg 2015;26:e647-51. [Crossref] [PubMed]
- Vukoje NJ, Enoz M, Cvetinov M, et al. Arco-palato-uvular flap: a new surgical technique for the treatment of palatal snoring in tonsillectomized patients. Kulak Burun Bogaz Ihtis Derg 2011;21:261-5. [Crossref] [PubMed]
- Pirsig W, Schafer J, Yildiz F, et al. Uvulopalatopharyngoplasty without complication: a Fujita complication. Laryngorhinootologie 1989;68:585-90. [Crossref] [PubMed]
- Mantovani M, Minetti A, Torretta S, et al. The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital 2012;32:48-53. [PubMed]
- Hessel NS, de Vries N. Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol 2003;260:91-5. [Crossref] [PubMed]
- Ye L, Antonelli MT, Willis DG, et al. Couples’ experiences with continuous positive airway pressure treatment: a dyadic perspective. Sleep Health 2017;3:362-7. [Crossref] [PubMed]
- Franklin KA, Anttilla H, Axelsson S, et al. Effects and side-effects of surgery for snoring and obstructive sleep apnea – a systematic review. Sleep 2009;32:27-36. [PubMed]
- Kato MG, Isaac MJ, Gillespie MB, et al. The incidence and characterization of globus sensation, dysphagia, and odynophagia following surgery for obstructive sleep apnea. J Clin Sleep Med 2018;14:127-32. [Crossref] [PubMed]
- Ishman SL, Benke JR, Cohen AP, et al. Does surgery for obstructive sleep apnea improve depression and sleepiness? Laryngoscope 2014;124:2829-36. [Crossref] [PubMed]
Cite this article as: Wadhera V, Fogarty G. Uvulopalatopharyngoplasty: a specific surgical technique aimed at minimising patient morbidity, with outcomes over 5 years in a regional centre. Aust J Otolaryngol 2020;3:11.


