Establishing an endoscopic laser service within the head and neck multidisciplinary team: a tertiary centre experience
Introduction
Head and neck cancer is the 5th most common cancer in men and 11th most common cancer in women in Australia accounting for over 5,200 new cases in 2019 (1). In 2020, laryngeal cancer alone accounted for 184,000 new cases worldwide and 99,840 deaths worldwide (2). The treatment of these cancers includes surgery, radiotherapy or chemotherapy, either as single modality treatment or in combination. The aim of all treatment strategies is to maximise disease-free survival, preserve function where possible and maintain the highest quality of life. The surgical management of head and neck cancers poses particular challenges due to the difficulty in achieving complete tumour excision with clear margins while preserving the integrity of the upper aerodigestive tract given that it is anatomically and functionally highly complex. Chemo-radiotherapy offers similar challenges due to its significant rate of both early and late morbidity affecting the head and neck region (3).
Transoral surgery has gained significant popularity as an alternative to morbid and disfiguring open surgery for certain cancers of the upper aerodigestive tract, whilst avoiding the long-term complications associated with radiotherapy. In particular in recent decades, the carbon dioxide (CO2) laser has become a valuable surgical tool in the head and neck surgeon’s armamentarium due to its unique physical properties. The CO2 laser was first proposed and successfully used by Strong & Jako in the 1970s to treat selected tumours in the head and neck (4), and this minimally invasive technique has been continuously refined since then. Arguably the most important and significant pioneer in transoral CO2 laser surgery has been Professor Steiner, who over the past four decades has led the way in advocating and broadening the scope of its use (5). Furthermore, Professor Steiner’s techniques have challenged the oncologic principle by Hallstead of en-bloc tumour resection (6) by utilising the characteristics of the CO2 laser tissue interaction to allow piecemeal resection of tumours with excellent oncologic results. These surgical techniques have also increased the range and stage of tumour that can be resected with the CO2 laser, such that there is now a role for CO2 laser surgery in resecting both benign and malignant tumours from the trachea, hypopharynx, oropharynx, larynx and oral cavity (7-11).
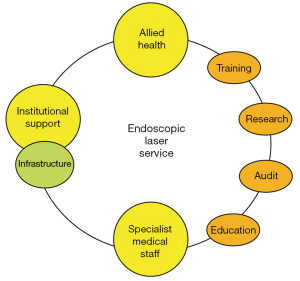
There are currently a number of barriers to the successful implementation of a comprehensive endoscopic laser service, and whilst there is an Australian and New Zealand Standard for laser safety, to date there have been no Australasian guidelines to establishing this kind of service within a multidisciplinary head and neck service (12). The current review aims to provide an overview of the considerations which in our opinion are required to set up such a service, by sharing experiences from a large Australian tertiary head and neck cancer centre (Figure 1).
Institutional support and infrastructure
Institutional support is vital in understanding and accepting the role of laser surgery in the management of upper aerodigestive tract neoplasia in order to ensure proper funding and the appropriate governance to provide this modality as part of a comprehensive and contemporary multi-disciplinary head and neck unit.
Minimally invasive transoral laser surgery (TOLS) for the management of upper aerodigestive tract cancers is a safe and oncologically proven modality with well-maintained functional and quality of life outcomes (13,14). Health economics studies demonstrate that it is cost effective and in some scenarios such as in early larynx cancer, cheaper than the historically perceived “Gold Standard” of external beam radiotherapy (15,16).
The use of a CO2 laser involves significant set-up and running costs, not only for the laser itself, but also for essential equipment such as the micromanipulator, smoke evacuator, dedicated surgical chair with arm supports, laser laryngoscopes, endoscopes and a variety of laryngeal instruments necessary to successfully perform minimally invasive surgery of the upper aerodigestive tract. Video capture technology is also a vital component of the management, particularly for laryngeal surgery in documenting the pathology, treatment, outcome and follow-up. Pre-operative assessment of all laryngeal lesions should include as a minimum an assessment of tumour location, size and spread for staging. In addition, video stroboscopy and voice recording provide essential information to educate and adequately inform both the patient and surgeon with regard to the likely functional outcomes and assists in the recovery and rehabilitation. Intra-operative recording allows for a dynamic documentation of the area of resection and highlights areas of concern. It is also important to accurately document the area of resection which allows for a correlation with the pathology report and is vital for revision, salvage or second primary surgery. Post-operative recordings can also be important to monitor healing and assess upper aerodigestive tract function. One very important aspect of proper and professional video documentation is its use in education and training of the future workforce both nationally and internationally.
The safety of any surgical technology is of paramount importance, and in the case of laser surgery there are significant risks, not only to the patient but also to all members of staff in the clinical area. There must therefore be adequate safety measures in place, including laser safety glasses, locks on operating room doors and laser-safe blinds on any windows. These protocols must be agreed at an institutional level, with input from a dedicated laser safety committee. Furthermore, training and support must be available for designated laser safety officers, whose role is to ensure the safe use of the laser on a day-to-day basis, and to ensure the competency of other laser practitioners.
Specialist medical staff
An integrated, comprehensive and high-volume multidisciplinary head and neck team who accept and support the role of TOLS is vital in order to run a successful head and neck laser service. A surgical team of at least two fellowship qualified surgeons is desirable, in order to enable peer experiential learning, facilitate case distribution and prevent long-term burnout. It also ensures continuity of service in times of illness or absence. Close working with oncology colleagues is a necessary prerequisite in order to provide prompt, personalised, empowered and informed consent and fully counsel patients regarding the risks and benefits of the varying treatment options. This is especially important when there are minimal differences in oncological outcomes when comparing TOLS with external beam radiotherapy for early glottic cancers (17,18).
TOLS presents unique anaesthetic challenges, due to the use of specialised laser-safe endotracheal tubes, or tubeless anaesthesia with jet ventilation, and the risk of airway fire. It is therefore important that the anaesthetist is competent to deal with these challenges and that good communication exists between both teams. There should be an agreed and documented airway fire protocol in all theatres using the CO2 laser that all staff are aware of. Close liaison and a good working relationship with a dedicated head and neck anaesthetist is therefore vital in order to maintain a safe and effective endoscopic laser service.
The cutting characteristics of the CO2 laser and the piecemeal nature of the resection present a particular diagnostic and unique management challenge to the tissue pathologist. This is due to the nature of the margins of resection, the intentional narrow margins, difficulty orientating the specimen, tissue dehydration and margin shrinkage. This has resulted in reports of false positive margin status rates on histopathology of up to 80% (19). These issues can be addressed by accurate photodocumentation, both of the tumour in situ and following excision, by inking the specimen margins following excision, and by fixing the specimens on a mount such as desiccated cucumber prior to immersion in formalin (20,21). Furthermore, a dedicated head and neck pathologist should be a part of any endoscopic laser service, and it is very important that there exists a close working relationship between the surgeon and pathologist to facilitate accurate labelling, surgeon input regarding the clinical scenario, and identification of critical resection margins for a successful oncologic outcome. This can be achieved by personally sitting down with the pathologist and together discussing, reviewing and auditing tissue specimens after TOLS.
Allied health staff and nursing
In addition to the staff directly involved in the procedure, many allied members of staff are involved in the patient journey. Perhaps most important is the role of the speech pathologist, due to the impact of TOLS on voice and swallowing outcomes. The impact on objective voice outcomes following TOLS for early glottic cancers is well established (18), and voice therapy has been shown to improve both subjective and objective voice outcomes post-operatively (22). It is vital that objective measures of voice quality are employed in the management of patients undergoing TOLS in order to facilitate research, as the oncological effectiveness of TOLS in many circumstances has been established and the focus moves to long term quality of life. Swallowing therapy and dietitian input may also be required following TOLS for oral, oropharyngeal and supraglottic tumours, and the relevant health professionals must have an understanding of the principles and techniques of TOLS in order to maximise the functional outcomes of patients.
Specialist operating theatre nursing staff are also vital in the provision of a safe, expedient service. They are trained not just in surgical procedural aspects, reducing unnecessary operative time and improving case turnover, but also vitally versed in laser safety to be an additional set of eyes while the surgeon is using the operating microscope.
Training and education
As with any surgical technique, adequate training is of tantamount importance, with TOLS requiring unique equipment and fundamentally different principles of tumour excision as compared to traditional open surgical approaches. Training in a high-volume centre with an experienced mentor allows for the development of a lifelong learning relationship, and to this end, fellowship training is advocated by many. This must be supplemented by simulation training on cadaveric laser surgery courses. Furthermore, surgeons, as well as operating room staff need, to be adequately trained in handling equipment and coordinating safety procedures (23). This training should be ongoing to ensure that all staff are up to date with current equipment and safety principles, and new staff are educated and trained effectively in a timely manner. Registrars and fellows entering the training pathway are sequentially progressed from case observation to assisted operating and eventually to supervised procedural independence. Our recommendation would be a minimum of 50 cases before embarking on independent case surgery with a collegial approach to case selection, allowing for scope in development of advanced skills and confidence.
Audit and research
A laser service is an ongoing and evolving treatment pathway and requires continual evaluation. All aspects of treatment should be regularly audited to ensure that optimal care is being provided. A record of all ‘near-miss’ and adverse events must be kept and discussed in order to learn from mistakes and improve safety, and a dedicated clinical database for laser surgery is advisable in order to facilitate meaningful evaluation of oncological outcomes as well as quality of life and functional outcomes. This is vital in order to effectively counsel patients regarding the risks and benefits of TOLS as opposed to alternative treatment modalities, with the added advantage that with the appropriate ethical approval, the data may be used to add to the evidence base on TOLS to the benefit of the wider medical community. Quality of life may be measured using one of the many assessment tools available, such as the Voice Related Quality of Life Tool (V-RQOL), the Voice Handicap Index (VHI) (24), University of Washington quality of life (UW-QOL) (25) or the MD Anderson Dysphagia Inventory (MDADI) (26). The Royal Australasian College of Surgeons (RACS) governance framework is utilised to facilitate improvements, benchmarking and quality assurance.
Conclusions
The oncological and functional benefits of TOLS have been studied extensively and are firmly established for selected tumours of the upper aerodigestive tract. However, the implementation of an endoscopic laser service requires not only financial and infrastructure support, but also a great deal of integration between the surgical team and a wide range of medical and allied health professionals, as well as non-medical staff.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-21-38/coif). FR serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Australian Institute of Health and Welfare (AIHW). Cancer in Australia 2019.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Machtay M, Moughan J, Trotti A, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol 2008;26:3582-9. [Crossref] [PubMed]
- Strong MS, Jako GJ. Laser surgery in the larynx. Early clinical experience with continuous CO 2 laser. Ann Otol Rhinol Laryngol 1972;81:791-8. [Crossref] [PubMed]
- Steiner W. Results of curative laser microsurgery of laryngeal carcinomas. Am J Otolaryngol 1993;14:116-21. [Crossref] [PubMed]
- Osborne MP. William Stewart Halsted: his life and contributions to surgery. Lancet Oncol 2007;8:256-65. [Crossref] [PubMed]
- Ferlito A, Silver CE, Howard DJ, et al. The role of partial laryngeal resection in current management of laryngeal cancer: a collective review. Acta Otolaryngol 2000;120:456-65. [Crossref] [PubMed]
- Ambrosch P, Kron M, Steiner W. Carbon dioxide laser microsurgery for early supraglottic carcinoma. Ann Otol Rhinol Laryngol 1998;107:680-8. [Crossref] [PubMed]
- Iro H, Waldfahrer F, Altendorf-Hofmann A, et al. Transoral laser surgery of supraglottic cancer: follow-up of 141 patients. Arch Otolaryngol Head Neck Surg 1998;124:1245-50. [Crossref] [PubMed]
- Martin A, Jäckel MC, Christiansen H, et al. Organ preserving transoral laser microsurgery for cancer of the hypopharynx. Laryngoscope 2008;118:398-402. [Crossref] [PubMed]
- Steiner W, Fierek O, Ambrosch P, et al. Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue. Arch Otolaryngol Head Neck Surg 2003;129:36-43. [Crossref] [PubMed]
- Australian/New Zealand Standard. AS/NZ 4173:2018 Safe use of lasers and intense light sources in health care. 3rd edition. Sydney: SAI Global Limited, 2018.
- Yoo J, Lacchetti C, Hammond JA, et al. Role of endolaryngeal surgery (with or without laser) versus radiotherapy in the management of early (T1) glottic cancer: a systematic review. Head Neck 2014;36:1807-19. [Crossref] [PubMed]
- Du G, Liu C, Yu W, et al. Voice outcomes after laser surgery vs. radiotherapy of early glottic carcinoma: a meta-analysis. Int J Clin Exp Med 2015;8:17206-13. [PubMed]
- Diaz-de-Cerio P, Preciado J, Santaolalla F, et al. Cost-minimisation and cost-effectiveness analysis comparing transoral CO2 laser cordectomy, laryngofissure cordectomy and radiotherapy for the treatment of T1-2, N0, M0 glottic carcinoma. Eur Arch Otorhinolaryngol 2013;270:1181-8. [Crossref] [PubMed]
- Higgins KM. What treatment for early-stage glottic carcinoma among adult patients: CO2 endolaryngeal laser excision versus standard fractionated external beam radiation is superior in terms of cost utility? Laryngoscope 2011;121:116-34. [Crossref] [PubMed]
- Warner L, Lee K, Homer JJ. Transoral laser microsurgery versus radiotherapy for T2 glottic squamous cell carcinoma: a systematic review of local control outcomes. Clin Otolaryngol 2017;42:629-36. [Crossref] [PubMed]
- Guimarães AV, Dedivitis RA, Matos LL, et al. Comparison between transoral laser surgery and radiotherapy in the treatment of early glottic cancer: A systematic review and meta-analysis. Sci Rep 2018;8:11900. [Crossref] [PubMed]
- Canis M, Ihler F, Martin A, et al. Transoral laser microsurgery for T1a glottic cancer: review of 404 cases. Head Neck 2015;37:889-95. [Crossref] [PubMed]
- Meulemans J, Hauben E, Peeperkorn S, et al. Transoral Laser Microsurgery (TLM) for Glottic Cancer: Prospective Assessment of a New Pathology Workup Protocol. Front Surg 2020;7:56. [Crossref] [PubMed]
- Robertson S, Cooper L, McPhaden A, et al. Refining the 'cucumber' technique for laryngeal biopsy. J Laryngol Otol 2011;125:626-9. [Crossref] [PubMed]
- van Gogh CD, Verdonck-de Leeuw IM, Boon-Kamma BA, et al. The efficacy of voice therapy in patients after treatment for early glottic carcinoma. Cancer 2006;106:95-105. [Crossref] [PubMed]
- O'Keefe E. Laser Safety. The Dissector 2018;46:17-8.
- Kazi R, De Cordova J, Singh A, et al. Voice-related Quality of Life in laryngectomees: assessment using the VHI and V-RQOL symptom scales. J Voice 2007;21:728-34. [Crossref] [PubMed]
- Rogers SN, Scott J, Chakrabati A, et al. The patients' account of outcome following primary surgery for oral and oropharyngeal cancer using a 'quality of life' questionnaire. Eur J Cancer Care (Engl) 2008;17:182-8. [Crossref] [PubMed]
- Gillespie MB, Brodsky MB, Day TA, et al. Swallowing-related quality of life after head and neck cancer treatment. Laryngoscope 2004;114:1362-7. [Crossref] [PubMed]
Cite this article as: Fussey J, Ahmadi N, Riffat F, Palme CE. Establishing an endoscopic laser service within the head and neck multidisciplinary team: a tertiary centre experience. Aust J Otolaryngol 2022;5:15.