
A cross-sectional study of hybrid reconstruction of the anterior skull base following extended endoscopic transnasal resection of skull base tumours
Introduction
The increase in anatomic understanding and the development of instrumentation over the past decades have facilitated the endoscopic transnasal approaches in resection of skull base lesions (1). Despite advances in endoscopic transnasal skull base surgery reconstruction of a large skull base defect can still be challenging (2). Robust techniques are essential for preventing cerebrospinal fluid (CSF) leakage and associated complications (3). Traditionally, large dural defects were reconstructed with inlay and onlay fascial grafts which were associated with a high incidence of postoperative CSF leak (4). The use of vascularized pedicled flaps has shown to be successful in reducing postoperative complications (4-6). The nasoseptal flap has gained popularity, however, this may not be viable in cases of malignant infiltration, revision or salvage procedures. Recent research has reported numerous materials and techniques used in skull base repair (7,8). There are different advantages and disadvantages to each approach and factors such as location and size of defect must be taken into consideration (9). We describe our hybrid endoscopic/open technique of using autologous fascia lata and a pedicled vascular pericranial flap to reconstruct the skull base defect following extended endoscopic skull base surgery. We present this article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-16/rc).
Methods
This is a retrospective cross-sectional study of sixteen consecutive cases of extended endoscopic transnasal resections of skull base tumours performed by a single ear, neck, and throat (ENT) surgeon and a neurosurgeon at two different major hospitals in Melbourne, Australia since December 2018. Clinical data on patient’s demographics and information on complications such as CSF leakage, postoperative infection and bleeding were recorded. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of St Vincent’s Hospital Melbourne (SVHM), Melbourne, Australia (No. QA20044). Informed consent was obtained from patients.
Results
Demographics
Sixteen patients (eleven males and five females) with a median age of 71 underwent the procedure (Table 1). There were two benign tumours and fourteen malignant tumours (Table 1). None of the patients had previous endoscopic transnasal resection of skull base or received radiotherapy prior to surgery.
Table 1
| Variables | Value |
|---|---|
| Age, median [range], years | 71 [44–86] |
| Female:male | 1:2.2 |
| Benign tumours | 2 |
| Meningioma | 2 |
| Malignant tumours | 14 |
| Sinonasal adenocarcinoma | 5 |
| Sinonasal squamous cell carcinoma | 6 |
| Basaloid carcinoma | 1 |
| Neuroblastoma | 1 |
| Melanoma | 1 |
Surgical technique
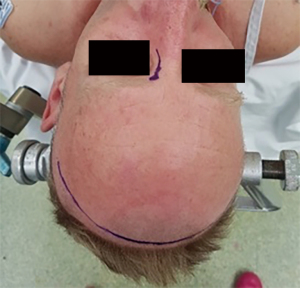
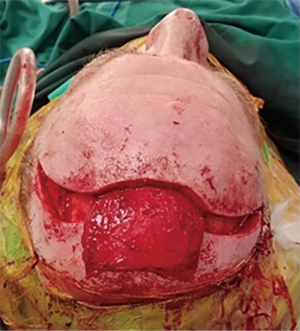
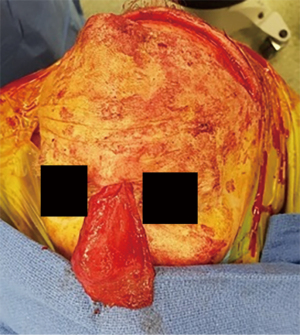
All patients were in the supine position with their head secured in Mayfield headframe. Intra-operative navigation was used in all cases. A coronal and lateral rhinotomy or Lynch incision were marked (Figure 1). Endoscopic resection of the tumour was carried out according to the position, extent and margins required. Full ablation of the ethmoid sinuses and endoscopic resection of the cribriform plate including septectomy was performed in all cases with additional ablation case dependent. Subgaleal dissection was done from a limited coronal incision to the supraobrbital ridge. The pericranial flap was then raised from the cranium (Figure 2). A scalp drain was inserted prior to the closure of the coronal incision. A modified Lynch incision was made and dissection undertaken to communicate with the harvest site in the scalp, taking care not to disturb the blood supply to the pericranium or injure the pedicle. A small external frontoethmoidectomy was then drilled to allow the flap to access the skull base defect. An autologous tensor fascia lata graft was harvested from lateral thigh and underlay in the dural defect. It is augmented externally by the vascularized pericranial flap rotated through the external bone defect (Figure 3). Surgical strips were utilized to help tack the flap in position and Tisseel was used to cover the flap edges. The flap was then supported by bilateral 7.5 nasopharyngeal airways with a Foley Balloon catheter and dissolvable packing.
Post-operative recovery
A computed tomography (CT) brain scan was performed for all patients on day-1 post operation. Minor pneumocephalus was noted in all patients. One patient had a small subdural haemorrhage that was treated conservatively and monitored with repeat scans. The scalp drain was removed by day-2. No significant scalp oedema or haematoma was reported. No other immediate post-operative complications such as CSF leakage or major bleeding were noted. All patients were followed up at 3-week post operation. Most patients had some nasal crusting which was debrided at time of review. One patient had a minor cutaneous fistula at the lateral rhinotomy incision which was conservatively managed with dressings. No patient required return to the operating theatre for post operative CSF leak.
Discussion
The aim of reconstruction after skull base resection is to provide a watertight barrier separating the intracranial contents from the sinonasal cavity to prevent postoperative CSF leakage and consequent intracranial complications (7,9). The introduction of the vascularlized flaps has significantly reduced the incidence of CSF leak as they were shown to promote faster and more complete healing (2,9,10). There has been extensive use of the pericranial flap for reconstruction of anterior skull base defects since it was first reported in 1981 (11). With the introduction of the nasoseptal flap, the pericranial flap has lost favour. The nasoseptal flap is harvested and positioned completely endoscopically without external incisions. With increasing completely endoscopic sinonasal and anterior cranial fossa tumour ablation, efforts have been made to keep the entire case endoscopic. Unfortunately, the most robust skull base repair may not be available endoscopically and external incisions for flap harvest and positioning should be considered. An external approach with the additional morbidity of the coronal incision and subgaleal dissection has its drawbacks but should not be abandoned (3,12,13). In this case series, pericranial flap was used as the vascularized pedicled flap instead of nasoseptal flap because of evidence or suspicion of tumour invasion of the nasal septum of those with malignant tumours. In the case of meningioma, the dural defect was too large to be repaired by nasoseptal flap.
The first case has 12 months of follow-up and it has been 2 months since the most recent case was done. All patients had no CSF leakage and excellent healing of the skull base. There were no complications at the harvest site. All patients with malignant tumour received post-operative radiotherapy. Similar to previous studies (10,14), the flap has shown to be robust and resistant to radiotherapy with no case reported to have any post-radiation complications thus far.
The harvest of pericranial flap is technically challenging particularly in elderly population where the tissue can be very fragile and extra caution will be required not to damage the flap. However, the morbidity of the coronal incision and dissection is minimal and haematoma can be avoided with the insertion of a scalp drain. Impairment of sensory and motor function of the scalp were not reported in any of the cases.
This case series is limited by its small sample and short-term outcomes. As research on approaches to endoscopic skull base reconstruction continues, data on long-term healing or complications can be collected to evaluate the association between risk factors and failures and to identify the population that may benefit from certain methods of endoscopic skull base reconstruction.
Conclusions
There were no post-operative complications of CSF leakage, meningitis, tension pneumocephalus or significant bleeding requiring additional packing or operative intervention. The use of pedicled pericranial flap in combination with autologous fascia lata in reconstruction of large dural defects resulting from an extended endoscopic transnasal skull base resection is a reliable method for skull base reconstruction. This technique should not be avoided simply because tumour ablation is completely endoscopic as the additional morbidity is small and it provides a robust skull base repair.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-16/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-16/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-16/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of St Vincent’s Hospital Melbourne (SVHM), Melbourne, Australia (NO: QA 20044). Informed consent was obtained from patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cavallo LM, Messina A, Cappabianca P, et al. Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus 2005;19:E2. [Crossref] [PubMed]
- Hadad G, Bassagasteguy L, Carrau RL, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 2006;116:1882-6. [Crossref] [PubMed]
- Zanation AM, Snyderman CH, Carrau RL, et al. Minimally invasive endoscopic pericranial flap: a new method for endonasal skull base reconstruction. Laryngoscope 2009;119:13-8. [Crossref] [PubMed]
- Eloy JA, Choudhry OJ, Christiano LD, et al. Double flap technique for reconstruction of anterior skull base defects after craniofacial tumor resection: technical note. Int Forum Allergy Rhinol 2013;3:425-30. [Crossref] [PubMed]
- Harvey RJ, Nogueira JF, Schlosser RJ, et al. Closure of large skull base defects after endoscopic transnasal craniotomy. Clinical article. J Neurosurg 2009;111:371-9. [Crossref] [PubMed]
- Turri-Zanoni M, Zocchi J, Lambertoni A, et al. Endoscopic Endonasal Reconstruction of Anterior Skull Base Defects: What Factors Really Affect the Outcomes? World Neurosurg 2018;116:e436-43. [Crossref] [PubMed]
- Hannan CJ, Kelleher E, Javadpour M. Methods of Skull Base Repair Following Endoscopic Endonasal Tumour Resection: A Review. Front Oncol 2020;10:1614. [Crossref] [PubMed]
- Khan DZ, Ali AMS, Koh CH, et al. Skull base repair following endonasal pituitary and skull base tumour resection: a systematic review. Pituitary 2021;24:698-713. [Crossref] [PubMed]
- Naik AN, Lancione PJ, Parikh AS, et al. Anterior skull base reconstruction: a contemporary review. Plast Aesthet Res 2021;8:22. [Crossref]
- Moon JH, Kim EH, Kim SH. Various modifications of a vascularized nasoseptal flap for repair of extensive skull base dural defects. J Neurosurg 2019;132:371-9. [Crossref] [PubMed]
- Price JC, Loury M, Carson B, et al. The pericranial flap for reconstruction of anterior skull base defects. Laryngoscope 1988;98:1159-64. [Crossref] [PubMed]
- Snyderman CH, Janecka IP, Sekhar LN, et al. Anterior cranial base reconstruction: role of galeal and pericranial flaps. Laryngoscope 1990;100:607-14. [Crossref] [PubMed]
- Solari D, Cavallo LM, Cappabianca P, et al. Skull base reconstruction after endoscopic endonasal surgery: new strategies for raising the dam. 2019 II Workshop on Metrology for Industry 4.0 and IoT (MetroInd4.0&IoT), 2019;28-32.
- Patel MR, Shah RN, Snyderman CH, et al. Pericranial flap for endoscopic anterior skull-base reconstruction: clinical outcomes and radioanatomic analysis of preoperative planning. Neurosurgery 2010;66:506-12; discussion 512. [Crossref] [PubMed]
Cite this article as: Ip F, Wang YY, Dixon B. A cross-sectional study of hybrid reconstruction of the anterior skull base following extended endoscopic transnasal resection of skull base tumours. Aust J Otolaryngol 2023;6:10.


