Paediatric airway management and simulation training: the Australian otolaryngology trainee experience
Introduction
Background
Paediatric airway emergencies are a challenging and stressful situation encountered by ear, nose and throat (ENT) surgeons and variable clinical exposure for registrars makes training difficult to teach and standardise (1). Paediatric airway emergencies are typically time sensitive and complex, involving a multidisciplinary team (2). These situations are frequently high-acuity but low-frequency events that can impact skill acquisition throughout training (2). Simulation scenarios can be used to complement surgical training to increase confidence and competence of surgical trainees and augment direct clinical exposure.
In the United States, 17% of paediatric patients presenting with airway pathology require emergency treatment in peripheral hospitals prior to arriving at a paediatric tertiary hospital (1). Adverse events in paediatric patients are significantly higher in peripheral hospitals than in tertiary paediatric emergency departments (1,3). All practicing ENT surgeons, regardless of whether they work in a paediatric tertiary hospitals, require skills in the assessment and management of the paediatric airway emergency.
Airway foreign bodies in the paediatric patient have high morbidity and mortality, responsible for 7% of accidental deaths of children under the age of 4 years (4). Trainees may have variation in exposure to the management of inhaled foreign bodies and thus there is variation in training and skill acquisition (5).
There is no known Australian data on trainee confidence levels in paediatric airway management. Studies in emergency and operating departments have supported a collaborative program between multidisciplinary teams and the role of simulation in improving paediatric airway management (1,6).
Internationally, a United Kingdom (UK) study by Awad et al. [2007] investigated the confidence levels in surgical airway emergency management for paediatric and adult patients by junior ENT staff (7). The study revealed variable results, with most of the respondents reportedly ‘not confident’ in managing airway emergencies. The authors concluded that systems of training for airway management needed to be improved (7). A United States study by Andrews et al. [2012] also found that otolaryngology and anesthesiology emergency airway management experience and training is heterogeneous and non-standardised (8).
Surveys in the UK and Canada have assessed the perceived lack of competency in ENT trainees in airway emergency management (7,9). Both studies revealed that almost half of all ENT trainees reported reduced confidence in their airway skills (7,9). Barriers to learning difficult airway management include infrequent training opportunities, early staff intervention, and workplace expectations for increased patient safety requiring senior surgeon management in airway emergencies (7,9). There is no known published Australian data assessing the exposure to and confidence levels of surgical trainees in paediatric airway management.
Simulation can complement trainee learning experience and has been associated with increased confidence and skill acquisition of training surgeons (5). Simulation-based training has been used in healthcare to develop both technical and non-technical skills, including communication, teamwork, situational awareness, and decision-making (10). Simulation incorporated into training is not a new concept within ENT. Temporal bone dissection in mastoid surgery and models for endoscopic sinus surgery are well established (11-13). Several studies have been conducted on the use of simulation in airway management, including surgical skills in tracheostomy, cricothyroidotomy, and oral intubation in paediatric patients (2). Simulation training in ENT airway management includes the use of animal models, cadavers, three-dimensional models, and virtual reality (14). The literature demonstrates an improvement in trainee with simulation of airway foreign body removal using manikins (15).
Objectives
This study primarily aims to define the clinical experience and confidence of Australian ENT trainees in paediatric airway management. Secondly, it explores the perceived utility of simulation in aiding the development of these skills. This is to identify current challenges and inform the future clinical training needs of this professional group. We present this article in accordance with the SURGE reporting checklist (available at available at https://www.theajo.com/article/view/10.21037/ajo-22-38/rc) (16).
Methods
A survey was distributed by the Australian Society of Otolaryngology-Head and Neck Surgery (ASOHNS) from April 2022 to May 2022 to all ENT-accredited registrars in Australia. A survey reminder was sent at 2 weeks and one month post initial distribution. This survey was optional, thus 21 responses were collated. The survey was developed in consultation with a statistician prior to distribution to ensure the validity. The survey consisted of four parts: (I) demographic information of the participant [level of surgical education and training (SET) (1–5) and number of completed paediatric ENT terms] to establish experience level; (II) clinical experience of trainees (i.e., number of logbook procedures); (III) confidence ratings (1—not at all confident, 2—not very confident, 3—neutral, 4—confident and 5—very confident) in technical skills and clinical situations; (IV) training and simulation experience.
Survey data were recorded in Microsoft Forms. This was encrypted and participants were non-identifiable. Relationships between trainee confidence and experience in clinical and simulation scenarios were established by conducting survey data analysis. All parts of the survey were mandatory to prevent missing data. Coverage error was minimized by inviting only ASOHNS trainees. There were no follow up surveys planned.
Survey data was analysed using Statistical Package for the Social Sciences software for statistical comparisons. A P value of <0.05 was considered significant. All analyses were performed using R (version 4.1.2). Counts and percentages were used to summarise categorical variables. Associations between categorical examples were tested using Fisher’s exact test.
Ethics exemption was obtained via the ASOHNS ethics committee and participant consent was obtained upon survey. The study was conducted following the Declaration of Helsinki (as revised in 2013). The research was performed based on the standard of Ethical Considerations in the Conduct and Reporting of Research: Privacy and Confidentiality.
Results
Part 1: demographic characteristics
The survey obtained 21 responses from across different Australian training regions and SET levels (Table 1). All of the SET 3, SET 4 and SET 5 respondents had completed a minimum of one 6-month tertiary-level accredited paediatric ENT term. All of the SET 1 and SET 2 respondents were either part way through or had not commenced their 6-month tertiary-level accredited paediatric ENT term.
Table 1
| Characteristic | Values |
|---|---|
| How many years have you been working as a doctor? | |
| 10+ | 1 (5%) |
| 5–7 | 5 (24%) |
| 8–10 | 15 (71%) |
| Which training region are you allocated to? | |
| New South Wales | 5 (24%) |
| Queensland | 7 (33%) |
| South Australia | 1 (5%) |
| Victoria | 4 (19%) |
| Western Australia | 4 (19%) |
| What is your level of SET training? | |
| SET 1 | 5 (24%) |
| SET 2 | 4 (19%) |
| SET 3 | 6 (29%) |
| SET 4 | 3 (14%) |
| SET 5 | 3 (14%) |
| How many years clinical experience as an unaccredited ENT registrar? | |
| <2 years | 3 (14%) |
| >4 years | 4 (19%) |
| 2–4 years | 14 (67%) |
| How many accredited terms (6 months) have you done of tertiary level paediatric ENT? | |
| 1 term | 6 (29%) |
| 2 terms | 5 (23%) |
| 3 or more terms | 1 (5%) |
| Less than 1 full term | 1 (5%) |
| None | 8 (38%) |
| How many unaccredited terms (6 months) have you done of tertiary level paediatric ENT? | |
| 1 term | 3 (14%) |
| 2 terms | 3 (14%) |
| Less than 1 full term | 2 (10%) |
| None | 13 (62%) |
SET, surgical education and training; ENT, ear, nose and throat.
Part 2: clinical experience
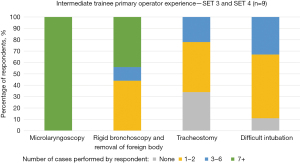
Data regarding clinical experience of each respondent was recorded. Data for primary operator, assistant/observer and experience in a simulated scenario were gathered for the most common paediatric airway procedures (microlaryngoscopy, rigid bronchoscopy/foreign body removal, paediatric tracheostomy and difficult intubation).
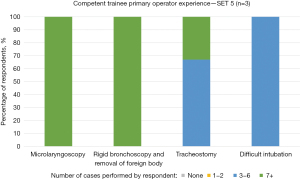
Figures 1-3 outline the primary operator numbers by each respondent and grouping to level of SET training: novice (SET 1 and SET 2), intermediate (SET 3 and SET 4) and competent (SET 5). These graphs demonstrate an increased experience with paediatric airway procedures with higher level of SET as would be expected.
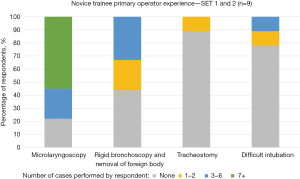
Data for novice trainee respondents showed that that 89% had assisted/observed a microlaryngoscopy, 89% had assisted/observed a rigid bronchoscopy/foreign body removal, 77% had assisted/observed a difficult intubation, whereas only 22% had assisted/observed a tracheostomy. None of the novice trainee respondents had completed a full 6-month accredited paediatric term.
Data for experience in simulation, showed only one novice trainee had performed a microlaryngoscopy and a rigid bronchoscopy in a simulated scenario. No novice trainees had performed a paediatric tracheostomy or difficult intubation in a simulation scenario. Of the total respondents (SET 1–SET 5), 29% had performed microlaryngoscopy, 27% had performed rigid bronchoscopy and foreign body removal, 9% performed paediatric tracheostomy, and 9% performed difficult intubation in a simulated scenario.
Part 3: confidence ratings
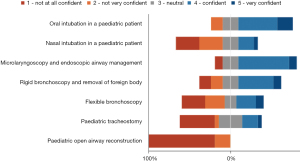
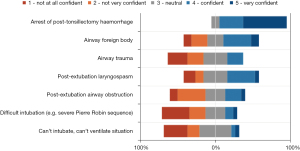
Figures 4,5 outline the response for trainee-reported self-confidence for specific technical skills and clinical situations related to paediatric airway management. Trainees could select one of five responses: ‘Not at all confident’, ‘Not very confident’, ‘Neutral’, ‘Confident’ or ‘Very Confident’.
Out of SET 1 and SET 2 respondents, 56% (n=5/9) were confident in performing oral intubation and 44% (n=4/9) in undertaking microlaryngoscopy. 56% of the SET 1 and SET 2 respondents were either not very confident or not at all confident in performing rigid bronchoscopy and 100% were not at all confident in performing a paediatric tracheostomy, although the majority had not completed an accredited 6-month paediatric term. SET 5 respondents (n=3) were confident or very confident in performing oral and nasal intubation, microlaryngoscopy, tracheostomy, rigid bronchoscopy, and airway foreign body removal.
Statistical analysis was performed using Kendall’s Tau(b) correlation. A significant P value (<0.05) indicated a significant correlation between the level of SET training and the responses. Increasing confidence was statistically significantly correlated with increasing level of SET training in paediatric technical skills of nasal intubation (τ =0.422, P=0.021), microlaryngoscopy and endoscopic airway management (τ =0.655, P<0.001), rigid bronchoscopy and airway foreign body removal (τ =0.623, P<0.001) and paediatric tracheostomy (τ =0.728, P<0.001). There was no statistical significant correlation with increasing level of SET training in technical skills of oral intubation (τ =0.354, P=0.058), flexible bronchoscopy (τ =0.250, P=0.2) and paediatric open airway reconstruction (τ =0.295, P=0.14).
Increasing confidence was statistically significantly correlated with increasing level of SET training in paediatric clinical situations of post-tonsillectomy hemorrhage (τ =0.599, P=0.002), airway foreign body removal (τ =0.625, P=0.001), airway trauma (τ =0.607, P=0.001), post-extubation airway obstruction (τ =0.691, P<0.001), difficult intubation (e.g., severe Pierre Robin sequence) (τ =0.685, P<0.001), “can’t intubate, can’t ventilate” (τ =0.639, P<0.001). There was no statistical significant correlation with increasing level of SET training in clinical situations of post-extubation laryngospasm (τ =0.525, P=0.005).
Part 4: skill development: training and simulation
Of the total respondents, 52% thought their training had provided adequate exposure to paediatric airway management and techniques. This included all SET 5 trainees (n=3/3) and a majority of SET 3 (n=5/6) and SET 4 (n=2/3). Of the participants who responded “no” (48%), most were early in training at SET 1 or 2 (n=8/9).
All respondents (n=21/21) ‘agreed’ or ’strongly agreed’ that simulation is an effective medium to learn; however, only 19% (n=4/21) had completed an airway simulation course, and 29% (n=6/21) completed a paediatric advanced life support course. All respondents (n=21/21) rated it as ‘useful’ or ‘very useful’ to practice clinical scenarios in a simulated learning environment, including foreign body removal, airway trauma, post-extubation laryngospasm, difficult intubation, can’t intubate, and can’t ventilate. Over 80% of respondents indicated it would be ‘very useful’ to practice technical skills including paediatric microlaryngoscopy, rigid bronchoscopy, intubation, and tracheostomy insertion in a simulated learning environment.
Discussion
Paediatric airway management is an acute situation where the development of technical and clinical skills is essential for ENT trainees and surgeons to provide safe and effective patient care. This is the first known published Australian data providing insight into Australian SET trainees’ experience and confidence in acute paediatric airway management.
The overall available international literature on this topic is lacking. Published data on the incidence of airway emergencies and changing outcomes over time are limited. Ongoing epidemiological research would clarify the need for improvement and the emphasis needed on trainees’ education (8).
Skills in paediatric airway management are essential for all ENT surgeons, not only those working in tertiary paediatric centres. More adverse events in paediatric airway management are reported in peripheral hospitals compared to emergency departments in tertiary paediatric centers (3). It is therefore crucial to develop competence and confidence in all trainees and practicing ENT surgeons.
The majority of training for paediatric airway management in Australia is undertaken in tertiary paediatric hospitals due to a centralised process for high-acuity situations. Non-technical skills and interdisciplinary teamwork is vital for the overall management of such patients and situations (8). A large focus of medical education in airway management has been on clinical and technical skills, rather than situation-based management and communication within the broader team (non-technical skills) (8).
This study suggests that Australian ENT trainees may have higher exposure to a range of paediatric airway management situations in comparison to international literature, with Andrews et al. [2012] reporting median emergency surgical airway exposure of just 6–10 cases (8).
Confidence levels in trainees are related to a variety of factors. Andrews et al. [2012] revealed that trainees can still have high confidence levels when supported by a skilled multidisciplinary team even in trainees with fewer airway emergency encounters (8). A large proportion of training for ENT regarding paediatric airway in Australia is in tertiary children’s hospitals and confidence may differ when a trainee or surgeon is placed outside this environment, working in non-tertiary paediatric hospitals.
This study investigated the more common technical skills and clinical scenarios faced by ENT trainees. Various technical skills and clinical situations were outlined and evaluated as part of the study survey. Information regarding both experience and confidence levels were gathered as part of the research with a specific focus on microlaryngoscopy, rigid bronchoscopy, tracheostomy and difficult airway.
This study showed that 85% of trainees across all SET levels had experience as a primary operator in microlaryngoscopy, performing more than 5 procedures. This correlated with high confidence levels in all trainees, wherein 70% of trainees were confident or very confident in performing this skill. Schwartz et al. [2018] found participants who practiced paediatric microlaryngoscopy techniques on a simulated model reported a subjective increase in confidence in performing this skill (5).
Rigid bronchoscopy and foreign body removal is currently a non-compulsory Performance Based Assessment (PBA) tool in the Australian otolaryngology training program. This study revealed that 81% of the respondents (n=17/21) performed this procedure at least once. The remaining 19% (n=4/21) were all in SET 1 or 2 and had not completed a full accredited paediatric term. This was correlated to confidence levels which showed <30% of all respondents were not confident or not at all confident (none of these respondents were in SET 4 or SET 5) as per their self-assessment. Okonkwo et al. [2016] revealed a lack of experience and confidence in the training among middle-grade ENT surgeons and emergency theatre staff in paediatric airway foreign body removal, which is consistent with our study results (4). While these situations are typically consultant-led, registrars are often the first-line practitioners to attend airway emergencies. Hence, training of junior and middle grade doctors is crucial to ensure patient safety (4). Okonkwo et al. [2016] also highlighted the importance of the multidisciplinary team in such situations and revealed that 54% of emergency theater staff had not dealt with an airway foreign body in the last year (4).
Skills and exposure to paediatric tracheostomy and difficult intubation were correlated with less experience in primary operator numbers in this study. Additionally, it correlated with less self-assessed confidence in these skills (48% not very confident or not at all confident in the paediatric tracheostomy and 62% not very confident or not at all confident in a difficult intubation scenario). With regard to difficult intubation, respondents were much more likely to be an assistant or observer rather than the primary operator (81% of respondents had exposure to difficult intubation as an observer or assistant). This is consistent with the international literature where high-acuity, time-sensitive situations are led by a consultant (5,10). The confidence level of a SET 5 trainee in a “can’t intubate, can’t ventilate” situation was neutral except for one respondent who was very confident. It is noticeable that this trainee had completed more paediatric terms than the other respondents and previously participated in a paediatric simulation course.
Training programs have had to develop innovative ways to expose trainees to critical experiences and skill sets due to limitations on trainee opportunities in airway management (2). The international literature has highlighted the potential of simulation in developing clinical and non-clinical skills with evidence supporting the effectiveness of such training in improving trainee performance (17,18).
All surveyed trainees in this study ‘agreed’ or ’strongly agreed’ that simulation is an effective medium to learn, however only 19% had attended a specific paediatric airway course. Simulation experience included microlaryngoscopy (29%), rigid bronchoscopy and foreign body removal (27%), paediatric tracheostomy (9%), and difficult intubation situation (9%). Nguyen et al. [2019] revealed a statistically significant improvement in the ENT trainees’ technical skills (paediatric tracheostomy, cricothyroidotomy, and intubation) and non-technical skills (delegation and communication) following simulation-based training modules (2).
Limitations of this study include the voluntary nature of the survey and is reflected in a smaller sample size and potential for sampling and non-response bias. Therefore, data may not be a true representation of the whole trainee cohort, as only those with an interest in paediatric otolaryngology may have responded. However, there was representation from all training regions and SET levels in the survey responses. This study did not attempt to assess the correlation between confidence and competence. Some international studies were more broadly conducted, including both adult and paediatric airway management. Andrews et al. [2012] revealed in some instances higher confidence levels but lower experience levels (8). They noted that trainees with high confidence in specific skills may be truly competent or overconfident (8). Likewise, other studies revealed a weak to moderate correlation between self-assessment and independently judged skill (19,20). This area was not assessed in our study; further research would be needed to determine the correlation between confidence and competence in Australian ENT trainees.
Conclusions
Paediatric airway management can present a challenging and stressful situation for ENT surgeons. This study provides insight into the Australian ENT trainee experience in paediatric airway management. It is reassuring that final-year trainees had good overall primary operator experience in various common technical and clinical situations. This correlated to higher confidence levels in these situations. As expected, the overall junior SET trainees had lower experience and confidence in paediatric airway management. Assessing the confidence and competence in these settings would be useful to guide further research.
Perceptions of the use of simulation were highly positive with 100% of respondents considering it as an effective medium to learn. Simulation scenarios are proven to complement surgical training, however few trainees have undertaken simulation exercises specific to the management of paediatric airway management. Access to simulation during training may provide opportunities to supplement direct clinical exposure.
Acknowledgments
The authors acknowledge the Children’s Health Queensland (CHQ) Biostatistics clinic for facilitation of the Health Biostatistics Service provided by the Queensland Cyber Infrastructure Foundation (QCIF).
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-38/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-38/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-38/coif). HB is a co-cordinator of the Annual Brisbane Paediatric Airway course. As such she is directly involved with paediatric airway simulation training for otolaryngology trainees. Storz Medical provides equipment for Brisbane paediatric airway course; Odyssey Finance sponsors Brisbane paediatric airway course; Olympus Medical provides equipment for Brisbnae paediatric airway course; Ambu Medical provides equipment and catering; Vorotex Medical provides equipment for Brisbane Paediatric airway course; Smith Medical provide financial sponsorship for the airway course. The course receives equipment and financial assistance from the industrires as above. She receives no personal financial compensation for her involvement in this teaching. She is both Queensland regional chair of training and secretary of the Australian and New Zealand Society of Paediatric Otolaryngology, both of which are unpaid positions. HB also serves as an unpaid Editorial Board Member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics exemption was obtained via the ASOHNS survey committee and participant consent was obtained upon survey. The research was performed based on the standard of Ethical Considerations in the Conduct and Reporting of Research: Privacy and Confidentiality.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Abu-Sultaneh S, Whitfill T, Rowan CM, et al. Improving Simulated Pediatric Airway Management in Community Emergency Departments Using a Collaborative Program With a Pediatric Academic Medical Center. Respir Care 2019;64:1073-81. [Crossref] [PubMed]
- Nguyen LHP, Bank I, Fisher R, et al. Managing the airway catastrophe: longitudinal simulation-based curriculum to teach airway management. J Otolaryngol Head Neck Surg 2019;48:10. [Crossref] [PubMed]
- Easley RB, Segeleon JE, Haun SE, et al. Prospective study of airway management of children requiring endotracheal intubation before admission to a pediatric intensive care unit. Crit Care Med 2000;28:2058-63. [Crossref] [PubMed]
- Okonkwo OC, Simons A, Nichani J, et al. Paediatric airway foreign body – The human factors influencing patient safety in our hospitals. Int J Pediatr Otorhinolaryngol 2016;91:100-4. [Crossref] [PubMed]
- Schwartz MA, Kavanagh KR, Frampton SJ, et al. Using simulators to teach pediatric airway procedures in an international setting. Int J Pediatr Otorhinolaryngol 2018;104:178-81. [Crossref] [PubMed]
- Johnson K, Geis G, Oehler J, et al. Simulation to implement a novel system of care for pediatric critical airway obstruction. Arch Otolaryngol Head Neck Surg 2012;138:907-11. [Crossref] [PubMed]
- Awad Z, Pothier DD. Management of surgical airway emergencies by junior ENT staff: a telephone survey. J Laryngol Otol 2007;121:57-60. [Crossref] [PubMed]
- Andrews JD, Nocon CC, Small SM, et al. Emergency airway management: training and experience of chief residents in otolaryngology and anesthesiology. Head Neck 2012;34:1720-6. [Crossref] [PubMed]
- Bouhabel S, Kay-Rivest E, Nhan C, et al. Error Detection-Based Model to Assess Educational Outcomes in Crisis Resource Management Training: A Pilot Study. Otolaryngol Head Neck Surg 2017;156:1080-3. [Crossref] [PubMed]
- Bhalla S, Beegun I, Awad Z, et al. Simulation-based ENT induction: validation of a novel mannequin training model. J Laryngol Otol 2020;134:74-80. [Crossref] [PubMed]
- Clifton N, Klingmann C, Khalil H. Teaching Otolaryngology skills through simulation. Eur Arch Otorhinolaryngol 2011;268:949-53. [Crossref] [PubMed]
- George AP, De R. Review of temporal bone dissection teaching: how it was, is and will be. J Laryngol Otol 2010;124:119-25. [Crossref] [PubMed]
- Magill JC, Tolley N. Non-technical skills simulation training. Curr Otorhinolaryngol Rep 2020;106-10. [Crossref]
- Alwani M, Bandali E, Larsen M, et al. Current state of surgical simulation training in otolaryngology: systematic review of simulation training models. Archives of Otorhinolaryngology-Head & Neck Surgery 2019;3:5. [Crossref]
- Griffin GR, Hoesli R, Thorne MC. Validity and efficacy of a pediatric airway foreign body training course in resident education. Ann Otol Rhinol Laryngol 2011;120:635-40. [Crossref] [PubMed]
- Grimshaw J. SURGE (The Survey Reporting GuidelinE). In: Moher D, Altman DG, Schulz KF, et al. editors. Guidelines for Reporting Health Research: A User’s Manual. John Wiley & Sons, Ltd.; 2014:206-13.
- Amin MR, Friedmann DR. Simulation-based training in advanced airway skills in an otolaryngology residency program. Laryngoscope 2013;123:629-34. [Crossref] [PubMed]
- Lind MM, Corridore M, Sheehan C, et al. A Multidisciplinary Approach to a Pediatric Difficult Airway Simulation Course. Otolaryngol Head Neck Surg 2018;159:127-35. [Crossref] [PubMed]
- Mandel LS, Goff BA, Lentz GM. Self-assessment of resident surgical skills: is it feasible? Am J Obstet Gynecol 2005;193:1817-22. [Crossref] [PubMed]
- Nadel FM, Lavelle JM, Fein JA, et al. Teaching resuscitation to pediatric residents: the effects of an intervention. Arch Pediatr Adolesc Med 2000;154:1049-54. [Crossref] [PubMed]
Cite this article as: Tynan T, Lloyd G, Burns H. Paediatric airway management and simulation training: the Australian otolaryngology trainee experience. Aust J Otolaryngol 2023;6:18.