
Outcomes after balloon dilation of the eustachian tube in children: a systematic review and meta-analysis
Introduction
The eustachian tube (ET) is a canal that extends anteriorly, medially and inferiorly from the middle ear to the nasopharynx (1). The anteromedial two-thirds are cartilaginous, while the posterolateral one-third is bony (2). A <10 mm segment of opposing mucosal tissue within the midportion of the cartilaginous ET acts as a valve (3). The valve is closed in its resting position and opens primarily through contraction of the tensor veli palatini (4).
The ET has three primary physiological functions pertaining to the middle ear: (I) pressure equalisation and ventilation; (II) mucociliary clearance of secretions; and (III) protection from nasopharyngeal pathogens, secretions and sounds (5). ET dysfunction (ETD) is defined as failure to perform any of these three functions (2). It is classified as either obstructive (dilatory) or patulous, with further categorisation into acute or chronic depending on whether signs and symptoms last longer than 3 months (5).
Obstructive ETD (OETD) refers to inadequate opening of the tubal lumen, and can be further divided into (I) functional obstruction, (II) dynamic obstruction, and (III) anatomical obstruction. Functional obstruction refers to mucosal changes in the lumen and is often caused by inflammation from an upper respiratory tract infection (URTI) or allergic rhinitis (5). Dynamic obstruction refers to muscular failure; and anatomical obstruction refers to extraluminal growths, for example adenoidal hypertrophy or tumours of the post nasal space (6). Otitis media (OM), middle ear effusion, tympanic membrane (TM) retraction, cholesteatoma and TM perforation are features of OETD. OETD causes a constellation of symptoms such as aural fullness, altered hearing, tinnitus, and a constant need to perform jaw-thrust or Valsalva manoeuvres (VMs) to equalise pressure (5). Comparatively, patulous ETD results from inadequate closure of the tubal lumen. It is much less common than OETD, with the majority of cases being idiopathic. Patients present with aural fullness and autophony (4,5).
Treatment of ETD can be divided into medical and surgical management. Medical management can include intranasal corticosteroids, intranasal decongestants, oral antihistamines and oral antibiotics, aiming to improve mucosal inflammation within the nasal cavity and ET (7). For adults, this is typically in conjunction with medical therapy for concomitant comorbidities, for example antacids or proton pump inhibitors for laryngoesophageal reflux (8). Comparatively, first-line surgical treatment includes any combination of adenoidectomy, myringotomy/paracentesis, and ventilation tube (VT) insertion. Recently, balloon dilation of the ET (BDET) is being used when dysfunction is refractory to first-line medical and surgical management (9).
BDET involves dilation of the ET by passing a balloon catheter under transnasal endoscopic visualisation. The procedure was first reported in 2009 (10), and has since grown in popularity worldwide (8). The literature is dominated by retrospective case series without any control group on this topic, however, three randomised control trials (RCTs) have been identified that demonstrated a statistically significant improvement in symptoms and tympanometry up to 12 months post-dilation in adults (11-13). The long-term effect is less conclusive as few studies report outcomes beyond 12 months (8). In any case, the literature primarily focusses on the adult population, with few studies assessing the procedure’s safety and efficacy in children (14).
By way of their anatomical make up, children have a greater tendency to develop ETD than adults, yet there is hesitancy in performing BDET in children due to the ET being shorter and lying closer to the horizontal plane. While the majority of anatomical maturation of the ET occurs by 5 years, adult morphology is only reached in early adolescence. This is an important factor when considering the approaching angle and length of the balloon catheter, as well as the angle of the endoscope (1).
This review aims to build on the works of Saniasiaya et al. (14) and Aboueisha et al. (15). Saniasiaya et al. (14) performed a systematic review of seven studies published up to December 2020, focussing on the indications for BDET and associated complications, while touching briefly on outcomes. Comparatively, Aboueisha et al. (15) performed a meta-analysis of seven studies, collating data on complications, tympanometry, and pure tone audiometry (PTA). This is the first study to comprehensively synthesise data across a large number of objective and subjective outcomes. Objective parameters include: (I) complications; (II) otomicroscopy; (III) tympanometry; (IV) PTA; (V) pressure equalisation through VM; and (VI) tubomanometry. The first five parameters are frequently measured. Tubomanometry, however, is a less common technique that measures the latency (R) of a pressure change transmitted to the TM when pressure is applied to the nasopharynx: R =0 indicates no opening, 0< R <1 indicates immediate opening, R =1 indicates accurate opening, and R >1 indicates delayed opening (15). In contrast, subjective parameters include patient symptoms, satisfaction, and quality of life (QOL). We present this article in accordance with the PRISMA reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-38/rc).
Methods
A systematic review was performed to evaluate the literature regarding BDET in the paediatric population. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (ID: CRD42023430248). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Literature search
Articles published up to and including 24 October 2023 were identified through CINAHL, Cochrane, Embase, Medline, PubMed, and Scopus using search strategies described in the Cochrane Handbook for Systematic Reviews of Interventions (16). All searches were completed on 24 October 2023, and search terms included “balloon”, “tuboplasty”, “endonasal”, “dilation”, “eustachian”, “auditory”, “pharyngotympanic”, “tube”, “child”, “preschool”, “school age”, “paediatric”, and “adolescent”. The full search strategies are listed in Table S1.
Selection
Two reviewers screened titles and abstracts against the inclusion and exclusion criteria. Studies were included if they investigated BDET, involved patients aged 18 years old and under, and were published up to and including 24 October 2023. Studies were excluded if the safety and/or efficacy of BDET was not assessed, if segregated data was not available for patients under 18 years old, and if the full text could not be accessed. Review articles and case reports were excluded, and non-English papers were translated to English through Google Translate.
Validity assessment
The included studies were appraised by two reviewers using the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool as described in the Cochrane Handbook. This tool evaluates the risk of bias related to (I) confounding, (II) selection of participants, (III) classification of interventions, (IV) deviations from intended interventions, (V) missing data, (VI) measurement of outcomes, and (VII) selective reporting. Each domain was evaluated as low, moderate, serious, critical or no information. Discrepancies were resolved with discussion.
Data extraction
Data was extracted using a standardised collection form by one reviewer and verified by another. Extracted data included citation, aim, study population, summary statistics, sample size, region, department, setting, study design, intervention (anaesthesia, preparation, access, dilation, removal), outcomes and key findings. The outcomes evaluated were complications, otomicroscopy, tympanometry, PTA, pressure equalisation through VM, tubomanometry, ear-related symptoms, satisfaction, and QOL.
Statistical analysis
For this meta-analysis, two different summary estimates (effect sizes) were calculated: mean differences for the continuous outcomes (PTA) and odds ratios for the binary outcomes (otomicroscopy, tympanometry, and VM). For the binary outcomes, the normal outcome was set as the negative outcome and the others as positive outcomes. If studies reported outcomes across multiple follow-up periods, the measure at 12 months or less was taken to ensure a sufficient sample size.
For all outcomes, separate random-effects models were fitted using a conditional generalized linear mixed-effects model (GLMM). This framework accounts for the repeated nature of the data (pre/post paired cohorts), while also incorporating an additional random component that accurately estimates the associated variance components. The likelihood ratio test was carried out for testing residual heterogeneity. Heterogeneity was examined using the Higgins I2 statistic, where low, moderate, and high heterogeneity were indicated by I2 values in the ranges of 0–25%, >25–75%, and >75–100%, respectively. Forest plots (main text) and funnel plots (Figures S1-S6) were produced for visualization of summary effect sizes and publication bias, respectively. If heterogeneity was not significant, summary estimates were presented with 95% confidence intervals (CIs). The metafor package (version 4.0-0) in R was used to conduct the meta-analyses.
Results
Results of search
The primary search yielded 353 titles and abstracts, of which 319 were excluded after screening. Major reasons for exclusion were duplicate publications (n=205), no relevance to BDET in children (n=88), and review-type studies (n=26). Of the remaining 34 articles, eight studies were excluded for being inaccessible, eight did not present segregated data for children, three did not include paediatric patients, two were clinical trial proposals, and two were case reports. Eleven records met eligibility criteria (Figure 1).
Study characteristics
Characteristics of each study are summarised in Table 1. Eight of the eleven included studies were retrospective case series, while the remaining three were historic cohort studies. The majority of studies originated in Germany (n=5), with other contributions from Turkey (n=2), United States (n=2), China (n=1), and Finland (n=1).
Table 1
| Study | Country | Study design | Patients | Procedures | Age range | Indication for procedure | Follow-up |
|---|---|---|---|---|---|---|---|
| Maier et al. (17), 2015 | Germany | RCS | 66 | 121 | 4–14 years old | Chronic OETD AND refractory to medical/surgical therapy | Mean, 96 days |
| Jenckel et al. (18), 2015 | Germany | RCS | 33 | 56 | 5–14 years old | Recurrent OM OR chronic adhesions with poorly mobile TM | 1, 3, 6, 9, 12, and 15 months |
| Leichtle et al. (19), 2017 | Germany | RCS | 52 | 97 | 3–15 years old | Recurrent OM OR chronic adhesions with poorly mobile TM OR persistent TM perforation OR cholesteatoma | 0.5, 2, 6, and 12 months |
| Tisch et al. (20), 2017 | Germany | RCS | 94 | 90 | 28 months– 13 years old |
Chronic ETD AND refractory to medical/surgical therapy | Mean, 13 months |
| Chen et al. (21), 2020 | China | HCS | 25 [49] | 46 [92] | 4–14 years old | Chronic ETD refractory to either tympanocentesis or tympanostomy tube insertion | 6, 12, and 18 months |
| Demir & Batman (22), 2020 | Turkey | HCS | 30 [62] | 55 [105] | 3–12 years old | Chronic ETD refractory to medical therapy | Mean (range), 14.4 months (13–16 months) |
| Demir & Batman (23), 2020 | Turkey | HCS | 30 [62] | 55 [105] | 3–12 years old | Chronic ETD refractory to medical therapy | 1.5 and 12 months |
| Tisch et al. (24), 2020 | Germany | RCS | 167 | 299 | 4–12 years old | COME for >3 months OR more than three episodes of AOM in last year OR CSOM OR cholesteatoma OR mesotympanic retraction pockets, AND refractory to medical/surgical therapy | Mean (95% CI), 2.6 months (0.3–16.1) |
| Toivonen et al. (25), 2021 | United States | RCS | 26 | 46 | 7–17 years old | Chronic ETD with previous tympanostomy tube insertion OR non-fixed TM retraction, AND failing medical therapy | 1, 6, 12, 24, and 36 months |
| Howard et al. (26), 2021 | United States | RCS | 43 | 80 | 6.6–17.7 years old | ETD OR chronic serous OM OR recurrent OM, AND refractory to medical/surgical therapy | NR |
| Oehlandt et al. (27), 2022 | Finland | RCS | 23 | NR | <16 years old | Chronic ETD | Mean ± SD, 33±12 months |
“Patients” refers to the number of patients who underwent either unilateral or bilateral BDET, while “procedures” refers to the number of BDET procedures. For historic cohort studies, the total number of patients and procedures performed among the BDET and control groups is given in square brackets. RCS, retrospective case series; OETD, obstructive eustachian tube dysfunction; OM, otitis media; TM, tympanic membrane; ETD, eustachian tube dysfunction; HCS, historic (retrospective) cohort study; COME, chronic otitis media with effusion; AOM, acute otitis media; CSOM, chronic suppurative otitis media; CI, confidence interval; NR, not reported; BDET, balloon dilation of the eustachian tube.
Patients
A total of 589 patients were included in the review for an aggregate of 945 procedures. All studies included patients under the age of 18 years old. The youngest patient was 28 months (20), and the oldest patient was 18 years old (26). Chronic OETD was a diagnostic indication for BDET in all studies, but the precise eligibility criteria varied. Some studies defined otomicroscopic and tympanometry findings in their criteria, while others were more generic. Eight of the 11 studies (17,20-26) included resistance to first-line medical therapy (anti-inflammatory, decongestant, antibiotics, corticosteroids) and/or surgical management (adenoidectomy, tympanic drainage, paracentesis, VT insertion) as an eligibility criterion, but the precise therapies were again subject to variance. Table 1 provides a summary of the patient eligibility criteria for each study.
Procedure
The BDET procedure can be divided into five stages: (I) preparation; (II) access; (III) dilation; (IV) removal; and (V) post-operative care. The use of a decongestant was consistent across all studies that reported the preparation stage, with xylometazoline being the most common.
In terms of access, seven studies (18,19,21-24,27) used the Spiggle and Theis applicator system, Maier et al. (17) used Bielefeld catheters, Howard et al. (26) used AERA catheters, and Toivonen et al. (25) used a combination of AERA and Karl Storz catheters. Only Jenckel et al. (18) customised the applicator system for their paediatric patients, amending the insertion parts to be thinner. The angle of the endoscope and applicator system varied across publications and are summarised in Table 2. While many studies had the option of different angles, the frequency of each was not reported. Most studies dilated the balloon at 10 bars for 2 min, with three studies (22,23,26) repeating the procedure before removing the catheter. Toivonen et al. (25) found the guide catheter to be too acutely angulated to perform transnasal BDET in seven (13 ears) of their 26 patients (46 ears). A transoral approach was used instead for these patients. The authors also decided to vary the duration of balloon inflation based on the burden and progression of disease.
Table 2
| Study | Preparation | Endoscope | Applicator system | Dilation | Post-operative care |
|---|---|---|---|---|---|
| Maier et al. (17), 2015 | NR | NR | Bielefeld; 3.28 mm × 20 mm†; 45° or 70°† | 10 bars for 2 min | Xylometazoline spray and panthenol oil for 3 days, followed by tube ventilation through Valsalva/Otovent |
| Jenckel et al. (18), 2015 | Xylometazoline | 3 mm; 45° | Spiggle and Theis; 3.28 mm × 20 mm†; 30°, 45°, or 70° | 10 bars for 2 min | NR |
| Leichtle et al. (19), 2017 | Xylometazoline | 3 mm; 0° or 45° | Spiggle and Theis; 3.28 mm × 20 mm†; 30°, 45°, or 70° | 8 bars for 2 min | NR |
| Tisch et al. (20), 2017 | Xylometazoline | Diameter NR; 30° | NR | 10 bars for 2 min | NR |
| Chen et al. (21), 2020 | NR | NR | Spiggle and Theis; 3.28 mm × 20 mm; angle NR | 10 bars for 2 min | NR |
| Demir & Batman (22), 2020 | Xylometazoline | 2.5 mm; 0° or 45° | Spiggle and Theis; 3.28 mm × 20 mm†; 30°, 45°, or 70° | 10 bars for 2 min, repeated after 2 min | Nasal saline irrigation and xylometazoline for 5 days |
| Demir & Batman (23), 2020 | Xylometazoline | 2.5 mm; 0° or 45° | Spiggle and Theis; 3.28 mm × 20 mm†; 30°, 45° or 70° | 10 bars for 2 min, repeated after 2 min | Nasal saline irrigation and xylometazoline for 5 days |
| Tisch et al. (24), 2020 | Xylometazoline | 3.28 mm; angle NR | Spiggle and Theis; 3.28 mm × 20 mm†; angle NR | 10 bars for 2 min | Xylometazoline in recovery room |
| Toivonen et al. (25), 2021 | Xylometazoline | 3 mm; 45° | Karl Storz/70°; diameter NR; AERA/55°; 6 mm × 16 mm† | 12 bars for 2 min | VMs and continued medical therapy |
| Howard et al. (26), 2021 | Oxymetazoline | 3 mm; 0° or 30° | AERA; 6 mm × 16 mm†; angle NR | 10–12 bars for 2 min, repeated | Nasal corticosteroid for 30 days, ear drops for 5 days, and VMs |
| Oehlandt et al. (27), 2022 | Cotton-soaked epinephrine | Diameter NR; 0° to 70° | Spiggle and Theis; 3.3 mm × 20 mm; 45° or 70° | 10 bars for 2 min | NR |
†, information sourced from product catalogue as not provided within paper. BDET, balloon dilation of the eustachian tube; NR, not reported; VM, Valsalva manoeuvre.
Removal after balloon deflation was consistent across all studies, and post-operative care was only reported in six studies. Four of these studies used a decongestant (17,22-24), two used nasal saline irrigation (22,23) and three used VMs (17,25,26). The timeframe for post-operative care varied among studies and is summarised in Table 2.
Parameters
Table 3 provides a summary of which parameters each study investigated, categorised into objective and subjective parameters. A systemic review was performed on all included studies, and meta-analyses were performed where possible.
Table 3
| Study | Objective | Subjective | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Compl. | Otomic. | Tymp. | PTA | TMM | VM | Sx | Sat. | QOL | ||
| Maier et al. (17), 2015 | √ | √ | √ | √ | √ | √ | ||||
| Jenckel et al. (18), 2015 | √ | √ | √ | |||||||
| Leichtle et al. (19), 2017 | √ | √ | √ | √ | √ | √ | √ | |||
| Tisch et al. (20), 2017 | √ | √ | √ | √ | ||||||
| Chen et al. (21), 2020 | √ | √ | √ | |||||||
| Demir & Batman (22), 2020 | √ | √ | √ | √ | ||||||
| Demir & Batman (23), 2020 | √ | √ | √ | √ | ||||||
| Tisch et al. (24), 2020 | √ | √ | √ | √ | √ | |||||
| Toivonen et al. (25), 2021 | √ | √ | √ | √ | √ | |||||
| Howard et al. (26), 2021 | √ | |||||||||
| Oehlandt et al. (27), 2022 | √ | √ | √ | |||||||
Compl., complications; Otomic., otomicroscopy; Tymp., tympanometry; PTA, pure tone audiometry; TMM, tubomanometry; VM, Valsalva manoeuvre; Sx, symptoms; Sat., satisfaction; QOL, quality of life.
Complications
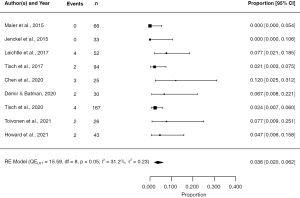
No serious complications were reported in any of the studies (Table 4). The most common minor complications were self-limiting hemotympanum and epistaxis, with post-operative otalgia, patulous ET and vestibular migraine being uncommon. The pooled estimate of the rate of complication was 3.6% (95% CI: 2.0% to 6.2%; P<0.001), as shown in Figure 2. The highest event rates were seen in studies with small sample sizes (19,21,24).
Table 4
| Study | Events | N | Event rate (%) | Description |
|---|---|---|---|---|
| Maier et al. (17), 2015 | 0 | 66 | 0.0 | – |
| Jenckel et al. (18), 2015 | 0 | 33 | 0.0 | – |
| Leichtle et al. (19), 2017 | 4 | 52 | 7.7 | Hemotympanum (n=1), epistaxis (n=3) |
| Tisch et al. (20), 2017 | 2 | 94 | 2.1 | Hemotympanum (n=1), post-operative otalgia (n=1) |
| Chen et al. (21), 2020 | 3 | 25 | 12.0 | Epistaxis (n=3) |
| Demir & Batman (22,23), 2020 | 2 | 30 | 6.7 | Hemotympanum (n=2) |
| Tisch et al. (24), 2020 | 4 | 167 | 2.4 | Epistaxis (n=4) |
| Toivonen et al. (25), 2021 | 2 | 26 | 7.7 | Patulous ET (n=2) |
| Howard et al. (26), 2021 | 2 | 43 | 4.8 | Epistaxis (n=1), vestibular migraine (n=1) |
BDET, balloon dilation of the eustachian tube; ET, eustachian tube.
Otomicroscopy
Four studies (17,24,25,27) assessed otomicroscopic findings pre- and post-operatively, while Demir and Batman (23) compared post-operative otomicroscopy between BDET and VT groups (Table 5). The incidence of normal otomicroscopy was seen to improve post-BDET in three studies (17,24,25), but was not reported by Oehlandt et al. (27). The latter study only reported a lack of significant difference in the incidence of TM retraction after BDET. All other studies reported the incidence of OM, retraction, adhesions, effusions, atrophy, perforation and cholesteatoma to decrease after BDET. This estimated average odds ratio of OM and retraction before and after BDET were 0.0033 (95% CI: 0.0010 to 0.0115; P<0.001) and 0.0073 (95% CI: 0.0007 to 0.0735; P<0.001), respectively (Figures 3,4). This indicates that the prevalence of OM and retraction are estimated to be 99.7% and 99.3% lower after undertaking BDET, respectively. Unfortunately, meta-analyses could not be performed for the otomicroscopic findings of effusion, perforation and atelectasis as the model was unable to be fit.
Table 5
| Study | Parameters | Result | P |
|---|---|---|---|
| Maier et al. (17), 2015 | Otomicroscopy | Increase in the incidence of normal TM (0% to 80%), with a correlating decrease in OM (14% to 0%), retraction/adhesions (37% to 6%), and tympanic effusions (49% to 14%), pre-operative n=84, post-operative n=66 | NP |
| Tympanometry | Increase in the incidence of type A (16% to 59%), with a correlating decrease in type B (65% to 27%) and type C (19% to 14%), pre-operative n=132, post-operative n=132 | NP | |
| PTA | AC at 1 kHz decreased from 18.39±12.29 to 10.54±11.13 dB, pre-operative n=65, post-operative n=22 | NP | |
| VM | Incidence of positive VM increased from 4% to 39%, n=39 | NP | |
| Jenckel et al. (18), 2015 | TMM | No trend towards improvement of tube opening, n=33 | NP |
| Leichtle et al. (19), 2017 | Tympanometry | Increase in the incidence of type A (14% to 50%), with a correlating decrease in type B (56% to 26%) and type C (15% to 13%), pre-operative n=52, post-operative n=14 | NP |
| TMM | Improvement in tube opening from 19% pre-operative (n=52) to 58% at 2 months (n=38) and 46% at 12 months (n=14) | NP | |
| VM | Incidence of positive VM increased from 13% (n=52) to 60% at 6 months (n=27) and 12 months (n=14) | NP | |
| Tisch et al. (20), 2017 | VM | Incidence of positive VM increased from 9% to 82%, pre-operative n=60, post-operative n=60 | NP |
| Chen et al. (21), 2020 | PTA | Decrease in ABG was more significant at 18 months in BDET (30.33±7.51 to 11.30±7.41 dB, n=25) vs. VT (32.26±7.14 to 15.87±7.10 dB, n=24) group. There was no significant difference at 6 or 12 months | 0.003 |
| Demir & Batman (23), 2020 | Otomicroscopy | Higher incidence of normal TM in BDET (93%) vs. VT (28%) group, with a correlating lower incidence of OM (7% vs. 34%), atrophy (0% vs. 16%), myringosclerosis (0% vs. 13%) and perforation (0% vs. 9%), BDET n=30, VT n=32 | NP |
| Tympanometry | Higher incidence of type A in the BDET (93%) vs. VT (65%) group, with a correlating lower incidence of type B (3% vs. 22%) and type C (3% vs. 13%), BDET n=30, VT n=32 | NP | |
| PTA | Greater decrease in ABG in BDET (27.6±7.6 to 9.6±3.6 dB) vs. VT (25.6±6.1 to 17.6±8.4 dB) group, BDET n=30, VT n=32 | 0.043 | |
| Tisch et al. (24), 2020 | Otomicroscopy | Increase in the incidence of normal TM (1% to 72%), with a correlating decrease in OM (11% to 3%), effusion (47% to 12%), and retraction (41% to 14%), pre-operative n=285, post-operative n=274 | <0.001 |
| Tympanometry | Increase in the incidence of type A (13% to 56%), with a correlating decrease in type B (60% to 29%) and type C (27% to 15%), pre-operative n=258, post-operative n=209 | <0.001 | |
| PTA | AC at 1 kHz decreased from 20±9 to 10±7 dB, pre-operative n=285, post-operative n=196 | <0.001 | |
| VM | Incidence of positive VM increased from 13% to 60%, pre-operative n=132, post-operative n=126 | NP | |
| Toivonen et al. (25), 2021 |
Otomicroscopy | Increase in the incidence of normal TM at 1 month (17%, n=42), 6 months (38%, n=39), 12 months (55%, n=29), 24 months (68%, n=19), and 36 months (93%, n=14) compared to pre-operative (9%, n=46), with a correlating decrease in perforation, retraction, effusion and atelectasis | <0.001 |
| Tympanometry | Increase in the incidence of type A at 6 months (50%, n=30), 12 months (59%, n=27), 24 months (53%, n=17), and 36 months (85%, n=13) compared to pre-operative (23%, n=40), with a correlating decrease in type B and C. There was no change at 1 month (24%, n=25) | <0.001 | |
| PTA | Decrease in ABG from pre-op (17.5±11.9 dB, n=46) to 1 month (8.5±9.5 dB, n=42), 6 months (10.8±10.8 dB, n=39), 12 months (12.4±9.2 dB, n=29), 24 months (11.5±7.7 dB, n=17), and 36 months (5.7±4.8 dB, n=14). Decrease in AC from pre-operative (21.9±13.2 dB) to 1 month (14.3±9.1 dB), 6 months (19.5±10.6 dB), 12 months (17.6±11.2 dB), 24 months (14.8±8.7 dB), and 36 months (12.4±4.9 dB) in the same groups of patients | <0.001 | |
| VM | Incidence of positive VM increased from pre-operative (27%, n=15) to 1 month (56%, n=16), 6 months (50%, n=10), 12 months (91%, n=11), 24 months (100%, n=6), and 36 months (100%, n=3) | <0.001 | |
| Oehlandt et al. (27), 2022 | Otomicroscopy | No significant difference in the incidence of TM retraction, effusion or perforation after BDET, n=23 | >0.05 |
| VM | No significant difference in the incidence of a positive VM after BDET, n=9 | >0.05 |
TM, tympanic membrane; OM, otitis media; NP, not performed; PTA, pure tone audiometry; AC, air conduction; VM, Valsalva manoeuvre; TMM, tubomanometry; ABG, air-bone gap; BDET, balloon dilation of the eustachian tube; VT, ventilation tube insertion.

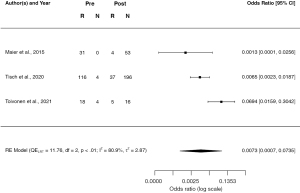
The varying post-operative follow-up periods between studies suggest that improvement can be seen as early as 3 to 36 months post-procedure (Table 5). The mean post-operative follow-up period for Maier et al. (17) and Tisch et al. (24) was 96 days and 2.6 months respectively. Improvement in otomicroscopy findings was more pronounced in both these studies when compared to the 1-month post-operative results of Toivonen et al. (25). While the incidence of normal otomicroscopy for Toivonen et al. (25) increased at 1 month, the incidence of perforated TMs more than doubled. It was only at the 6-month mark that perforations reduced. Despite a high attrition rate (70.0%), the improvement in otomicroscopic findings appears to continue to 36 months (25).
Furthermore, the results of Demir and Batman (23) suggest that normal otomicroscopy was more prevalent after BDET (93%, n=30) than VT insertion (28%, n=32) at the 12-month follow-up (Table 5). The pre-operative breakdown of otomicroscopic findings was not provided for comparison.
Tympanometry
Five studies assessed tympanometry (17,19,23-25), with Toivonen et al. (25) providing the most detailed post-operative analysis (Table 5). While models could not be fit to perform a meta-analysis, all studies found an increase in the incidence of type A tympanograms post-BDET, with a corresponding decrease in type B and C tympanograms. Toivonen et al.’s (25) study suggests that type C tympanograms convert to type B as early as 1-month post-operative, but it takes up to 6 months to see a conversion to type A tympanograms. Furthermore, Demir and Batman (23) found that type A tympanograms were more common after BDET (93%, n=30) than VT insertion (66%, n=32) at 12 months. However, pre-operative tympanogram findings were not available for comparison.
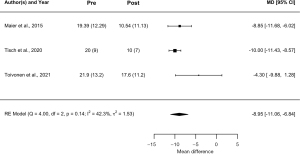
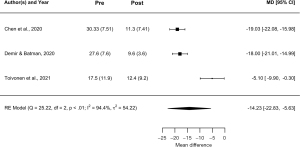
PTA
Five studies assessed PTA, where two studies measured air conduction (AC) (17,24), two studies measured air-bone gap (ABG) (21,23), and one study measured both (25) (Table 5). The frequency (1 kHz) was specified for only two studies (17,24). BDET was observed to reduce AC by a mean of 8.95 dB (95% CI: −6.84 to 11.06; P<0.001), and ABG by a mean of 14.23 dB (95% CI: 5.63 to 22.83; P<0.001) (Figures 5,6). Toivonen et al. (25) found the decrease to arise from as early as 1-month and continue until at least 36-month post-operative (P<0.001). Demir and Batman (23) compared BDET with VT insertion, where both BDET and VT insertion groups had statistically significant decreases in ABG at 12 months (P<0.05); the decrease was considerably more efficacious in the BDET group (P<0.05).
Tubomanometry
Two studies assessed tubomanometry over time. Jenckel et al. (18) found no consistent trend in results, while Leichtle et al. (19) found a reduction in obstructed ETs and an increase in tube opening (Table 5). Trends were mild at 2-week post-operative, but become significant at 2 months.
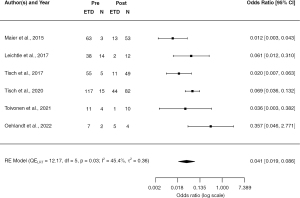
Valsalva
Five of six studies (17,19,20,24,25) found the incidence of a positive VM to improve after BDET, with Oehlandt et al. (27) the only study to find no difference with a small sample size of n=9 (Table 5). The estimated average odds ratio for the prevalence of an abnormal VM before and after BDET was 0.041 (95% CI: 0.019 to 0.086, P<0.001), suggesting the procedure improves pressure equalisation by an average of 95.9% (Figure 7). The improvement was seen as early as 2 weeks post-operative by Leichtle et al. (19), and continued for as long as 36 months post-operative with Toivonen et al.’s (25) study (Table 5).
Symptoms, satisfaction, and QOL
Five studies (18-21,26) assessed the prevalence of ear-related symptoms prior to and after BDET. Although none of the studies used validated questionnaires, an improvement was seen in the frequency of hearing loss, otalgia, ear pressure, and otalgia from as early as 2 weeks post-operative (Table 6). This improvement continued until 15 months (18), after which no data was available. Oehlandt et al. (27) obtained mixed results, finding recurrences of acute OM to cease in 12 of 14 children, but the incidence of aural fullness, otalgia, and hearing loss to be unchanged after BDET.
Table 6
| Study | Parameters | Result | P |
|---|---|---|---|
| Maier et al. (17), 2015 | Satisfaction | Patients rated their satisfaction as very satisfied (65%), satisfied (21%), neutral (14%), and unsatisfied (0%), n=66 | NP |
| Jenckel et al. (18), 2015 | Sx | Incidence of hearing loss reduced from pre-operative (21/25) to 1 month (6/15) and 15 months (4/11). Otalgia (5/19 to 2/9 to 1/13) and otorrhea (7/20 to 1/10 to 2/13) also reduced at the same timeframes | NP |
| Leichtle et al. (19), 2017 | Sx | Incidence of hearing loss reduced from pre-operative (37%) to 2 weeks (32%), 2 months (10%), 6 months (9%), and 12 months (8%). Ear pressure (84%, 44%, 16%, 9%, 12%) and otalgia (21%, 7%, 5%, 8%, 10%) also reduced at the same timeframes | NP |
| Satisfaction | Patient satisfaction increased from pre-operative (0%, n=52) to 2 weeks (72%), 2 months (76%), 6 months (68%), and 12 months (72%) | NP | |
| QOL | LADLs decreased from pre-operative (60%) to 54%, 14%, 16% and 18% at the same timeframes and sample sizes as the satisfaction data | NP | |
| Tisch et al. (20), 2017 | Sx | Hearing loss improved in 76% of patients, n=34 | NP |
| Satisfaction | Patients rated their satisfaction as very satisfied (56%), satisfied (26%), neutral (15%), and unsatisfied (3%), n=34 | NP | |
| Chen et al. (21), 2020 | Sx | Incidence of complete symptom resolution was 35% in the BDET group and 28% in the VT group | 0.116 |
| Demir & Batman (22), 2020 | Sx/satisfaction/QOL | OM-6 questionnaire scores were significantly reduced from pre-operative (BDET 31±5 vs. VT 29±4) to 6 months (BDET 15±6 vs. VT 18±7) and 12 months (BDET 8±2 vs. VT 8±2) (P<0.001). The reduction was greater in the BDET group at 6 months (P=0.018) but not 12 months (P=0.510) | 0.018 |
| Oehlandt et al. (27), 2022 | Sx | Incidence of aural fullness, otalgia and hearing loss was unchanged after BDET. However, recurrences of acute OM reportedly ceased in 12/14 children | 0.001 |
NP, not performed; Sx, symptom; QOL, quality of life; LADLs, limitation in activities of daily living; OM, otitis media; BDET, balloon dilation of the eustachian tube; VT, ventilation tube insertion.
Three studies (17,19,20) assessed the satisfaction of patients after the procedure, all finding >70% of patients to be either satisfied or very satisfied post-BDET (Table 6). Leichtle et al. (19) was the only study to assess the satisfaction and limitation in activities of daily living (LADLs) over time, finding satisfaction to remain >70% from 2 weeks post-operative and LADLs to decrease from 2 months post-operative. Lastly, Demir and Batman (22) used OM-6, a validated questionnaire about symptoms, satisfaction, and QOL, where a lower score represents a better outcome. BDET was observed to outperform VT (P<0.05) insertion at 6 months (15±6 vs. 18±7), but was equivalent at 12 months (8±2 vs. 8±2).
Validity assessment
An overview of the validity assessment is provided in Table 7. The overall risk of bias was evaluated to be low across all the included studies. However, several studies had moderate risk in one or more domains. Firstly, attrition over the follow-up period was moderate in three studies (19,20,25). This could not be assessed for Jenckel et al. [2015] and Oehlandt et al. (27) as sample sizes were not reported over the follow-up period. Additionally, the risk of selective reporting was moderate for two studies. Oehlandt et al.’s (27) study included adults and children, but only some of the outcomes were segregated for children. Toivonen et al. (25), on the other hand, had a control group where they assessed the number of failed procedures and the 2-year failure-free probability, but no other objective or subjective outcomes were reported from this control group. No explanations were provided for the omission in either paper.
Table 7
| Study | ROBINS-I | |||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | Overall | |
| Maier et al. (17), 2015 | Low | Low | Low | Low | Low | Low | Low | Low |
| Jenckel et al. (18), 2015 | Low | Low | Low | Low | NI | Low | Moderate | Low |
| Leichtle et al. (19), 2017 | Low | Low | Low | Low | Moderate | Low | Low | Low |
| Tisch et al. (20), 2017 | Low | Low | Low | Low | Moderate | Low | Low | Low |
| Chen et al. (21), 2020 | Low | Low | Low | Low | Low | Low | Low | Low |
| Demir & Batman (22), 2020 | Low | Low | Low | Low | Low | Low | Low | Low |
| Demir & Batman (23), 2020 | Low | Low | Low | Low | Low | Low | Low | Low |
| Tisch et al. (24), 2020 | Low | Low | Low | Low | Low | Low | Low | Low |
| Toivonen et al. (25), 2021 | Low | Low | Low | Low | Moderate | Low | Moderate | Low |
| Howard et al. (26), 2021 | Low | Low | Low | Low | Low | Low | Low | Low |
| Oehlandt et al. (27), 2022 | Low | Low | Low | Low | Low | Low | Moderate | Low |
ROBINS-I tool evaluates the risk of bias related to (I) confounding, (II) selection of participants, (III) classification of interventions, (IV) deviations from intended interventions, (V) missing data, (VI) measurement of outcomes, and (VII) selective reporting. Overall bias is also included in the final column. Each domain is evaluated as low, moderate, serious, critical or no information. ROBINS-I, Risk Of Bias In Non-randomized Studies of Interventions.
Discussion
ETD constitutes a large number of visits to healthcare practitioners for both adults and children. The exact pathophysiology is yet to be elucidated, but microbial overload, anatomical obstruction and negative pressure appear to play key roles (28). These are emphasised in children, who contribute 1.3 healthcare visits to every one adult visit (29). Children have shorter and more horizontal tubes, allowing pathogens and nasopharyngeal secretions to ascend easily into the middle ear. This is combined with a “floppy” cartilaginous tube that has reduced elastin and therefore restricted tube opening. Larger adenoids close to the tubal ostium can also limit the drainage of secretions (30). Although negative pressure was thought to be a by-product of hypertrophic adenoids, this does not explain the incidence of retracted TMs in patients who have undergone adenoidectomies and VT insertions. It has been postulated that chronic inflammation of the tensor tympani may be an additional factor that causes negative pressure through retraction of the malleus (28). This aetiology in children appears to be driven by developmental factors, whereas adult ETD is more commonly linked to allergic rhinitis and laryngoesophageal reflux (30,31).
BDET is becoming an increasingly popular therapy in adults who have failed standard medical and surgical therapy. However, anatomical differences in the ET of children have limited its use in this population. This review provides quantitative and qualitative evidence to support the use of BDET in children, building on the works of Saniasiaya et al. (14) and Aboueisha et al. (15). Saniasiaya et al. (14) performed a systematic review of seven studies published up to December 2020, focussing on the indications for BDET and associated complications, while touching briefly on outcomes. Comparatively, Aboueisha et al. (15) performed a meta-analysis of seven studies, collating data on complications, tympanometry and PTA. This is the first study to comprehensively synthesise data across a large number of objective and subjective outcomes.
The mechanism by which BDET works is relatively unknown, but is thought to be due to elastic deformation of the ET. In the short term, dilation of the ET causes mucosal tears and cracks in the cartilage (32). As low compliance is a feature of OETD, the subsequent increase in compliance post-procedure improves the functional obstruction and tube opening (33). In the long term, damage to the mucosa and submucosa induces regeneration of healthy ciliated pseudo-columnar epithelium. The damage appears to extend to the inflamed cell lining that comprises macrophages, lymphocytes, and lymphoid follicles, reducing the inflammatory burden (32). This correlates with reduced mucosal inflammation observed after BDET (25,34).
The predominance of research uses BDET in patients who have OETD refractory to standard medical and surgical treatment, a trend also seen in publications in this review. Demir and Batman (23) was the only study to assess BDET as a first-line surgical procedure in children, demonstrating better outcomes to VT insertion in otomicroscopy, tympanometry and PTA. A subjective assessment of ear-related symptoms, satisfaction and QOL through the OM-6 questionnaire was also more improved at 6-month, but became equivalent at 12 months. One study, however, is not sufficient to guide evidence-based management, and neither is data from uncontrolled studies. Extrapolating from adult RCTs, Siow and Tan (35) recommend BDET in patients who have aural fullness >12 weeks, a type B or C tympanogram, a score ≥2 on the Eustachian Tube Dysfunction Questionnaire (ETDQ-7), no improvement with VMs, and failure of either nasal steroids for 4 weeks or oral steroids for 1 week. Being refractory to surgical management is not a component of this indication criteria, but the recommendation was only based on two RCTs and would need further assessment in children.
In terms of the BDET procedure, the balloon catheter was dilated with 10 bars of pressure for two minutes in most studies. Demir and Batman (23) and Howard et al. (26) were the only studies that repeated dilation before catheter removal. However, Demir and Batman (23) compared BDET with VT insertion rather than pre-operative measures, and Howard et al. (26) only assessed the frequency of complications. As comparative data is not available in adult studies either, further research would be required to elucidate whether two dilations within a single procedure improves outcomes.
Interestingly, most studies used adult balloon catheters to perform BDET in children. The most common applicator system in the included studies was from Spiggle & Theis (18,19,21-24,27), which contrasts to the Stryker system being the most common in Australia. Other companies include AERA (25,26), Bielefeld (17), and Karl Storz (25). Jenckel et al. (18) was the only study to use customised insertion parts that were thinner, but the angles and length of the catheter were the same. No complications were observed in their study, but Maier et al. (17) and Toivonen et al. (25) also reported no complications with entirely adult equipment. Moreover, the complications described in other studies were minor and self-limiting. Overall, this would suggest that adult catheters are safe and effective in children.
The use of adult catheters in children conforms with Magro et al.’s (1) computed tomography (CT) study that found the 95% CI for cartilaginous ET length to be 19–21 mm in children ≤4 years old and 24–25 mm in children 5–7 years old. Despite the Spiggle and Theis balloon being 20 mm in length, it was used on children as young as 2 years old without any serious complications. Nevertheless, the AREA catheter would be more appropriate for children ≤4 years old as its balloon length is 16 mm. No lengths could be obtained for Bielefeld and Karl Storz catheters. Furthermore, the horizontal angle of the ET only increases by an average of 7° from patients ≤4 years old (17°) to >18 years old (24°) (1). As most companies offer a range of catheter angles, there would be no requirement to customise this for children. In the case that the catheter is too acutely angled, a transoral approach can be used as described by Toivonen et al. (25).
Overall, BDET was found to be effective in both objective and subjective parameters. Firstly, no serious complications were reported in any of the studies. The estimated event rate for minor complications (3.6%; 95% CI: 2.0% to 6.2%; P<0.001) was comparable to Aboueisha et al.’s (15) meta-analysis (5.1%; 95% CI: 3.2% to 8.1%; P<0.001), representing self-limiting epistaxis, hemotympanum and otalgia. Substantial improvements were noted in otomicroscopy, tympanometry, PTA and VMs when comparing pre-operative and post-operative results. These findings also aligned with Aboueisha et al. [2022], which found a 48.1% reduction in type B tympanograms (64.2% pre-operative vs. 16.1% post-operative) and a 59.7% reduction in ABG (25.3 dB pre-operative vs. 10.2 dB post-operative) on PTA. In contrast, tubomanometry was only seen to improve in Leichtle et al.’s (19) study, with Jenckel et al. (18) observing no trend. The utility of tubomanometry has been promising in adults, including patients with OM (36). Yet, Jenckel et al. (18) and Leichtle et al. (19) are the only studies to assess this technique in children. Jenckel et al. (18) claims that low compliance, narrow anatomy and excess mucous may cause inaccuracies in children. However, clear trends in Leichtle et al.’s (19) research suggests that this may not be the case. Further evaluation of tubomanometry in children is needed before evaluating its utility.
Improvements were also noted in ear-related symptoms and QOL, with the majority of patients (or their parents) reporting satisfaction with the procedure. These trends were only observed through non-validated questionnaires, with Demir and Batman (23) being the only study to use a validated questionnaire (OM-6). While the latter found a statistically significant reduction in OM-6 score post-operatively, they did not segregate data into the parameters described above. The OM-6 questionnaire is currently the only validated ETD questionnaire for children (37). While the ETDQ-7 is commonly used, it has only been validated in adults (38,39).
Furthermore, Demir and Batman (23) was the only study to assess BDET as first-line surgical management. Comparing its efficacy to VT insertion, BDET was found to be superior in otomicroscopy, tympanometry, and PTA. The OM-6 score was also found to be lower at 6 months, but became equivocal at 12 months. The results suggest that BDET may be an effective first-line surgical procedure for children refractory to medical therapy. However, as with most findings in this review, further research with prospective trials would be needed to validate this indication.
Strengths & limitations
As mentioned previously, this systematic review and meta-analysis is more comprehensive than previous publications, encompassing a larger number of objective and subjective parameters across a greater number of studies to strongly support the safety of BDET in children. This review provides a strong platform to setup prospective studies and randomised Controlled trial of BDET in children.
In spite of this, several key limitations hinder its ability to draw robust conclusions. Firstly, the reliance on a small sample size of only 11 studies raises concerns about the generalizability of findings, limiting the strength of any conclusions. Moreover, most of the included studies are retrospective case series without control groups or historic cohort studies, which are inherently susceptible to bias and confounding variables. Additionally, the variations in follow-up periods across these studies create challenges when trying to assess the effect size at different time points, making it difficult to draw a clear temporal relationship between interventions and outcomes. Heterogeneity among objective outcome measures also poses a challenge. Due to small number of studies, moderator analyses could not be performed for otomicroscopic retraction and ABG, both showing heterogeneity >50%. Lastly, the lack of a validated questionnaire to assess ETD-related symptoms and QOL in children underscores the reliability of the subjective outcomes. These limitations highlight the need for more rigorous and standardized research in this area to draw more robust conclusions regarding the effectiveness of BDET in children.
Conclusions
BDET is a safe and potentially effective procedure for the treatment of OETD. No serious complications have been reported in the literature, with most adverse events being self-limiting epistaxis and hemotympanum. Post-operative improvements were seen in otomicroscopy, tympanometry, PTA, pressure equalisation through VMs, and questionnaires relating to symptoms, satisfaction, and QOL. The findings for tubomanometry were less convincing with only one of two studies observing a positive trend in tube opening. As the current body of evidence is based on retrospective case series and historic cohort studies, further research in the form of prospective cohort studies and RCTs would be needed before BDET can be recommended as evidence-based management. Future research should also assess the utility of tubomanometry as an objective parameter, investigate BDET as first-line surgical management, and use validated questionnaires for subjective evaluation.
Acknowledgments
Our sincere thanks to Joshua Knowles and Dr. Farah Zahir from the Queensland Cyber Infrastructure Foundation Facility for Advanced Bioinformatics for conducting statistical analyses for the meta-analysis.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-23-38/rc
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-38/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (ID: CRD42023430248). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Magro I, Pastel D, Hilton J, et al. Developmental Anatomy of the Eustachian Tube: Implications for Balloon Dilation. Otolaryngol Head Neck Surg 2021;165:862-7. [Crossref] [PubMed]
- Hamrang-Yousefi S, Ng J, Andaloro C. Eustachian Tube Dysfunction. 2023. In: StatPearls. Treasure Island: StatPearls Publishing; 2024.
- Poe DS, Pyykkö I. Measurements of Eustachian tube dilation by video endoscopy. Otol Neurotol 2011;32:794-8. [Crossref] [PubMed]
- Smith ME, Scoffings DJ, Tysome JR. Imaging of the Eustachian tube and its function: a systematic review. Neuroradiology 2016;58:543-56. [Crossref] [PubMed]
- Schilder AG, Bhutta MF, Butler CC, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol 2015;40:407-11. [Crossref] [PubMed]
- Alper CM, Teixeira MS, Mandel EM, et al. Dissecting eustachian tube dysfunction: From phenotypes to endotypes. PLoS One 2023;18:e0283885. [Crossref] [PubMed]
- Mehta NK, Ma C, Nguyen SA, et al. Medical Management for Eustachian Tube Dysfunction in Adults: A Systematic Review and Meta-Analysis. Laryngoscope 2022;132:849-56. [Crossref] [PubMed]
- Huisman JML, Verdam FJ, Stegeman I, et al. Treatment of Eustachian tube dysfunction with balloon dilation: A systematic review. Laryngoscope 2018;128:237-47. [Crossref] [PubMed]
- Adil E, Poe D. What is the full range of medical and surgical treatments available for patients with Eustachian tube dysfunction? Curr Opin Otolaryngol Head Neck Surg 2014;22:8-15. [Crossref] [PubMed]
- Ockermann T, Reineke U, Upile T, et al. Balloon dilatation eustachian tuboplasty: a clinical study. Laryngoscope 2010;120:1411-6. [Crossref] [PubMed]
- Meyer TA, O'Malley EM, Schlosser RJ, et al. A Randomized Controlled Trial of Balloon Dilation as a Treatment for Persistent Eustachian Tube Dysfunction With 1-Year Follow-Up. Otol Neurotol 2018;39:894-902. [Crossref] [PubMed]
- Anand V, Poe D, Dean M, et al. Balloon Dilation of the Eustachian Tube: 12-Month Follow-up of the Randomized Controlled Trial Treatment Group. Otolaryngol Head Neck Surg 2019;160:687-94. [Crossref] [PubMed]
- Liang M, Xiong H, Cai Y, et al. Effect of the combination of balloon Eustachian tuboplasty and tympanic paracentesis on intractable chronic otitis media with effusion. Am J Otolaryngol 2016;37:442-6. [Crossref] [PubMed]
- Saniasiaya J, Kulasegarah J, Narayanan P. Outcome of Eustachian Tube Balloon Dilation in Children: A Systematic Review. Ann Otol Rhinol Laryngol 2022;131:797-804. [Crossref] [PubMed]
- Aboueisha MA, Attia AS, McCoul ED, et al. Efficacy and safety of balloon dilation of eustachian tube in children: Systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 2022;154:111048. [Crossref] [PubMed]
- Higgins JPT, Thomas J, Chandler J, et al. editors. Cochrane Handbook for Systematic Reviews of Interventions. 2019. Available online: https://onlinelibrary.wiley.com/doi/book/10.1002/9781119536604
- Maier S, Tisch M, Maier H. Balloon dilation of the Eustachian tube in pediatric chronic obstructive Eustachian tube dysfunction patients. HNO 2015;63:686-8, 690-4, 696-7. [Crossref] [PubMed]
- Jenckel F, Kappo N, Gliese A, et al. Endonasal dilatation of the Eustachian tube (EET) in children: feasibility and the role of tubomanometry (Estève) in outcomes measurement. Eur Arch Otorhinolaryngol 2015;272:3677-83. [Crossref] [PubMed]
- Leichtle A, Hollfelder D, Wollenberg B, et al. Balloon Eustachian Tuboplasty in children. Eur Arch Otorhinolaryngol 2017;274:2411-9. [Crossref] [PubMed]
- Tisch M, Maier H, Sudhoff H. Balloon dilation of the Eustachian tube: clinical experience in the management of 126 children. Acta Otorhinolaryngol Ital 2017;37:509-12. [Crossref] [PubMed]
- Chen S, Zhao M, Zheng W, et al. Myringotomy and tube insertion combined with balloon eustachian tuboplasty for the treatment of otitis media with effusion in children. Eur Arch Otorhinolaryngol 2020;277:1281-7. [Crossref] [PubMed]
- Demir B, Batman C. Efficacy of balloon Eustachian tuboplasty on the quality of life in children with Eustachian tube dysfunction. Acta Otolaryngol 2020;140:297-301. [Crossref] [PubMed]
- Demir B, Batman C. Efficacy of balloon Eustachian tuboplasty as a first line treatment for otitis media with effusion in children. J Laryngol Otol 2020; Epub ahead of print. [Crossref] [PubMed]
- Tisch M, Maier S, Preyer S, et al. Balloon Eustachian Tuboplasty (BET) in Children: A Retrospective Multicenter Analysis. Otol Neurotol 2020;41:e921-33. [Crossref] [PubMed]
- Toivonen J, Kawai K, Gurberg J, et al. Balloon Dilation for Obstructive Eustachian Tube Dysfunction in Children. Otol Neurotol 2021;42:566-72. [Crossref] [PubMed]
- Howard A, Babu S, Haupert M, et al. Balloon Eustachian Tuboplasty in Pediatric Patients: Is it Safe? Laryngoscope 2021;131:1657-62. [Crossref] [PubMed]
- Oehlandt H, Pulkkinen J, Haavisto L. Balloon Dilation of the Eustachian Tube in Chronic Eustachian Tube Dysfunction: A Retrospective Study of 107 Patients. J Int Adv Otol 2022;18:495-500. [Crossref] [PubMed]
- Urík M, Tedla M, Hurník P. Pathogenesis of Retraction Pocket of the Tympanic Membrane-A Narrative Review. Medicina (Kaunas) 2021;57:425. [Crossref] [PubMed]
- Vila PM, Thomas T, Liu C, et al. The Burden and Epidemiology of Eustachian Tube Dysfunction in Adults. Otolaryngol Head Neck Surg 2017;156:278-84. [Crossref] [PubMed]
- Bluestone CD. Studies in otitis media: Children's Hospital of Pittsburgh-University of Pittsburgh progress report--2004. Laryngoscope 2004;114:1-26. [Crossref] [PubMed]
- Grimmer JF, Poe DS. Update on eustachian tube dysfunction and the patulous eustachian tube. Curr Opin Otolaryngol Head Neck Surg 2005;13:277-82. [Crossref] [PubMed]
- Kivekäs I, Chao WC, Faquin W, et al. Histopathology of balloon-dilation Eustachian tuboplasty. Laryngoscope 2015;125:436-41. [Crossref] [PubMed]
- Smith ME, Weir AE, Prior DCC, et al. The mechanism of balloon Eustachian tuboplasty: a biomechanical study. Med Biol Eng Comput 2020;58:689-99. [Crossref] [PubMed]
- Silvola J, Kivekäs I, Poe DS. Balloon Dilation of the Cartilaginous Portion of the Eustachian Tube. Otolaryngol Head Neck Surg 2014;151:125-30. [Crossref] [PubMed]
- Siow JK, Tan JL. Indications for Eustachian tube dilation. Curr Opin Otolaryngol Head Neck Surg 2020;28:31-5. [Crossref] [PubMed]
- Liu P, Su K, Zhu B, et al. Detection of eustachian tube openings by tubomanometry in adult otitis media with effusion. Eur Arch Otorhinolaryngol 2016;273:3109-15. [Crossref] [PubMed]
- Rosenfeld RM, Goldsmith AJ, Tetlus L, et al. Quality of life for children with otitis media. Arch Otolaryngol Head Neck Surg 1997;123:1049-54. [Crossref] [PubMed]
- McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: The Eustachian Tube Dysfunction Questionnaire (ETDQ-7). Laryngoscope 2012;122:1137-41. [Crossref] [PubMed]
- Teixeira MS, Swarts JD, Alper CM. Accuracy of the ETDQ-7 for Identifying Persons with Eustachian Tube Dysfunction. Otolaryngol Head Neck Surg 2018;158:83-9. [Crossref] [PubMed]
Cite this article as: Ramagiri B, Lynch A, Lloyd G, Chang A. Outcomes after balloon dilation of the eustachian tube in children: a systematic review and meta-analysis. Aust J Otolaryngol 2024;7:10.



