
Otalgia from temporomandibular disorder in Ear, Nose and Throat surgery: a literature review and diagnostic algorithm
Introduction
Patients with otalgia will commonly be referred to Ear, Nose and Throat (ENT) surgeons. Whilst otalgia is often due to primary pathology affecting the ear itself, secondary causes where the pain is referred from other head and neck sites can be just as frequent (1,2). Temporomandibular disorder (TMD) describes a group of conditions characterised by pain or dysfunction in the temporomandibular joint (TMJ) and the muscles that control its movement. Patients with TMD experience impaired quality of life with evidence demonstrating increased rates of chronic pain, social dysfunction, sleep disruption, and restriction on daily activities (3,4). Whilst TMD is not classically thought of as an ENT pathology, patients with pain-related TMD frequently report pain in or in front of the ear in addition to other otological symptoms including tinnitus, hearing loss, aural fullness, and vertigo (2,5-7). Consequently, many patients suffering from otalgia will naturally be referred to an ENT surgeon for additional workup following a normal otoscopic examination but without appropriate recognition of TMD (8).
ENT surgeons play a pivotal role in diagnosing and commencing early multidisciplinary treatment in patients presenting with otalgia from TMD to their clinic (9,10). The Committee on Temporomandibular Disorders recently highlighted numerous pertinent challenges affecting patient care including a continuing notion that TMD is primarily a dental issue despite patients presenting to diverse healthcare providers, substantial delays in diagnosis and treatment due to the complex origin and pathophysiology of pain in the head and neck region, and a lack of coordinated and multidisciplinary treatment (11,12). These challenges are especially notable in ENT settings but can be ameliorated by an understanding and utilisation of the simple, clear, and reliable diagnostic definition for TMD as published in the dual-axis Diagnostic Criteria for TMD (DC/TMD) (7). The aim of this study is to review and synthesise the current evidence to outline the role of the otolaryngologist in the diagnosis and multidisciplinary management of otalgia from TMD. We present this article in accordance with the Narrative Review reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-42/rc).
Methods
A review of the literature was performed based on the intended population, context, and outcome (PCO) outlined in Table 1. A search was performed in the PubMed, EMBASE, Web of Science, and Cochrane databases for articles in English on otalgia from TMD from inception until March 20, 2023. A combination of the following search terms was used in each database: (“otalgia” OR “earache” OR “ear pain”) AND (“temporomandibular joint dysfunction syndrome” OR “TMJ*” OR “TMD*” OR “temporomandibular joint*”).
Table 1
| Item | Description |
|---|---|
| Population | Patients with otalgia |
| Context | Co-existing or causative temporomandibular disorder |
| Outcome | The role of the otolaryngologist in the diagnosis and management |
Following the removal of duplicates, two authors independently reviewed the titles and abstracts of studies using the Rayyan web application (13) (Rayyan Systems Inc., United States) for potential relevance. The eligibility of these article’s full texts were evaluated and their reference lists were screened for any additional relevant articles. Consensus was obtained by discussion between the authors where disagreement arose. The inclusion criteria included: English language, subjects of all ages, subjects with otalgia relating to TMD, and full-text availability. Animal studies, case reports, and narrative reviews were excluded. The selected articles were read in full and their salient findings were incorporated into an evidence-based discussion of the prevalence, diagnosis, and multidisciplinary management of otalgia from TMD.
Results
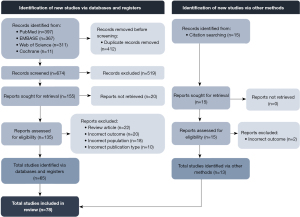
A total of 1,086 articles were identified using the search terms listed above (Figure 1). Only 674 articles remained after the removal of duplicates. There were 155 articles discussing otalgia from TMD in their title of abstract and following the removal of 20 articles where no full text was available, the full text of the remaining 135 were evaluated. Another 15 articles were identified from the citation lists of these articles. Seventy-eight studies were finally included in this review. The reasons for exclusion of studies included: narrative review articles (n=22), incorrect outcome (n=20), incorrect population (n=18), and incorrect publication type (n=10).
Discussion
The prevalence of otalgia from TMD
It is pivotal that ENT surgeons recognise the prevalence of otalgia from TMD to enable prompt diagnosis. Pain-related TMD affects approximately 10% of the general population over the age of 18 (14). The proportion of these patients reporting otalgia varies considerably in published studies with rates ranging from 3% to 100% of the total TMD population (9,15-30). Still, the statistically significant association between TMD and the presence of otalgia has been repeatedly evidenced (31-36). The explanation for the substantial variability is not completely clear but may reflect the subjective nature of assessing TMD and its symptoms and multiple studies with very small sample sizes (31,37-49), introducing cognitive bias. Instead, those studies with larger cohorts and systematic reviews synthesising multiple cohort studies provide higher level evidence on the overall prevalence. Cooper and Kleinberg (50) found that 82.4% of 4,528 subjects with TMD suffered from at least one otological symptom with otalgia being the most common in 52.2% of the total population. Ramirez et al. (51) reviewed 46 studies in 2008 and noted otalgia to affect 51.1% of those with TMD, again the most prevalent otological symptom. Interestingly, Porto De Toledo et al. (52) instead found ear fullness to be the more common (74.8%), however, they nevertheless highlighted a rate of otalgia from TMD in 55.1% of patients. It can be ascertained from this that roughly half of the patients with TMD will experience otalgia.
As the patients comprising the aforementioned studies included those presenting to a variety of clinicians ranging from primary care physicians to medical and surgical specialists, these findings may not be generalisable to ENT surgeons (43,53). Only a few studies have investigated this population specifically but have also found considerable rates of otalgia from TMD. For example, Brookes et al. (42) and Adegbiji et al. (43) concluded that 82.2% and 100% of patients diagnosed with TMD in their ENT clinic suffered from otalgia, respectively. Cox (54) instead found the ear to be one of and the most painful sites in only 35% and 6% of patients with TMD presenting to their private ENT practice. When evaluating those who present with otalgia to their clinic, Anwar et al. (55) and Fenton et al. (53) illustrated that 10% and 15% fulfilled the diagnosis for TMD, respectively. Moreover, when only including those with referred otalgia, Sumitha and Joseph (56) demonstrated that TMD comprised approximately half of all subjects. ENT surgeons should maintain a high index of suspicion for TMD in patients presenting with otalgia to their clinics, particularly where primary ear disease is excluded (56-58).
A diagnostic algorithm for patients with suspected otalgia from TMD
The diagnosis of pain-related TMD is made on history and physical examination findings alone (7,52). In the clinical evaluation of patients presenting with suspected otalgia from TMD, it is the role of the ENT surgeon to not only confirm the diagnosis of TMD but to also exclude alternative or co-existing causes of otalgia. An evidence-based diagnostic algorithm for otolaryngologists that can be applied in clinical settings and facilitate prompt treatment is presented in Figure 2. Each component of the diagnostic algorithm is expanded upon in the following sections.

History
ENT surgeons should first characterise the patient’s otalgia in more detail by taking a history. For a diagnosis to be made, it is required that this pain be modified—meaning elicited, exacerbated, or alleviated—by movements of the jaw such as those with chewing, clenching, talking, or yawning (7,59). This pain will be unilateral in most cases and bilateral symptoms should prompt suspicion for an alternate pathology (30,43). In addition to ear pain, patients may also report co-existing pain at other sites including the TMJ, masseter, pre-auricular, and temporal regions (59). The nature and timing of otalgia are unreliable indicators of TMD, as exemplified through inconsistencies in these descriptions in the literature and should not be used to inform the diagnosis (36,60). These differences may reflect the multitude of unique theorised pathophysiological pathways underlying otalgia from TMD (50). Despite these differences, the pain in those with otalgia from TMD is significantly more severe than other forms of painful TMD, translating to a greater proportion of patients seeking help and requiring treatment (19,21,28,36,50,61-65). Every ENT surgeon should familiarise themselves with and routinely apply the six-item TMD-pain in their clinical practice to rapidly and confidently diagnose TMD (Table 2) (66). A score greater than or equal to three demonstrates a 99.1% sensitivity and 96.9% specificity for differentiating pain-related TMD from healthy controls
Table 2
| 1. In the last 30 days, how long did any pain last in your jaw or temple area on either side? |
| a) No pain |
| b) Pain comes and goes |
| c) Pain is always present |
| 2. In the last 30 days, have you had pain or stiffness in your jaw on awakening? |
| a) No |
| b) Yes |
| 3. In the last 30 days, did the following activities change any pain (that is, make it better or make it worse) in your jaw or temple area on either side? |
| A. Chewing hard or tough food |
| a) Yes |
| b) No |
| B. Opening your mouth or moving your jaw forward or to the side |
| a) Yes |
| b) No |
| C. Jaw habits such as holding teeth together, clenching, grinding, or chewing gum |
| a) Yes |
| b) No |
| D. Other jaw activities such as talking, kissing, or yawning |
| a) Yes |
| b) No |
An “a” response receives 0 points; a “b” response 1 point; a “c” response 2 points. A total score greater than or equal to 3 demonstrates a 99.1% sensitivity and 96.9% specificity for differentiating pain-related TMD from healthy controls. Adapted with permission from Gonzalez YM, Schiffman E, Gordon SM, et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc 2011;142:1183-91. Copyright 2011 by American Dental Association. TMD, temporomandibular disorder.
Although non-pain symptoms are not needed to diagnose TMD, they should still be screened for as they help to characterise disease burden and may illuminate alternative or additional pathologies. Functional symptoms including jaw stiffness and adventitious sounds such as clicking, popping, and crepitus may support the presence of intra-articular TMD such as disc displacement, degenerative joint disease, or subluxation (7). However, these symptoms may be present in a large proportion of asymptomatic patients. It is increasingly recognised that TMD is frequently associated with additional otological symptoms (18,33-35,37,39,51,67-73). Therefore, patients should be asked about the presence of aural fullness, hearing loss, vertigo, and tinnitus with clinicians appreciating that the presence of these do not necessarily suggest an alternate diagnosis and may instead actually represent more severe forms of TMD (63).
It is critical to not miss alternative or co-existent red-flag diagnoses contributing to the patient’s otalgia. Those with TMD alone should not report swelling, warmth, and redness over the TMJ site or any motor and sensory difficulties (8). The presence of a previous medical or surgical otological history increases the likelihood of primary otalgia. Systemic symptoms including fever, nausea and vomiting, and reduced level of activity in the context of an underlying middle or outer ear infection should be ruled out, particularly in the paediatric population where acute otitis media is especially common (30). In older patients with significant risk factors, additional symptoms from head and neck malignancies including throat pain, dysphagia, oral cavity ulcers, and neck lumps must be assessed (53,74). Anwar et al. (55) showed that 3.3% of hypopharyngeal and 2% of laryngeal carcinomas present with otalgia as the primary complaint. In a cohort of 52 patients with nasopharyngeal carcinoma, Epstein and Jones (75) demonstrated that 15.4% presented with otalgia with one diagnosis being missed in a patient incorrectly diagnosed with TMD.
The population groups frequently experiencing otalgia seem to reflect the epidemiology of TMD overall. Studies consistently evidence that females more often report and report a larger number of otological symptoms than males (15,16,27-29,61). Moreover, those commonly affected tend to be middle-aged (15,27). This reflects higher rates of self-reported life stress and, hence, bruxism in these groups (16,20,32,48). Although children are less likely to suffer from TMD compared to adults, ENT surgeons must appreciate the substantial likelihood of its presence in the context of otalgia with normal ear examination. This is supported by Blake et al. (49) who showed that 67% of children presenting to ENT clinics with otalgia and normal ear drums had evidence of TMD.
As described in the Axis II (contributing factors) of the DC/TMD, clinicians should apply the biopsychosocial model to their patient’s pain and evaluate for the resulting distress and disability from TMD (8). TMD alone is strongly correlated with increased rates of somatisation, anxiety, and depression and notably, this may even be more prominent in those experiencing otalgia (27,76,77). Lam et al. (21) demonstrated that TMD had a statistically significantly greater negative impact on normal life functions in subjects with otological symptoms compared to those without. Kuttila et al. (20) showed that subjects with otalgia were more likely to have an obvious treatment need, and hence were more likely to pay more visits to a physician than other groups. In settings where pain has persisted beyond 6 months, prior treatment has been unsuccessful, and/or there is concern for significant distress, ENT surgeons should utilise core Axis II instruments including The Patient Health Questionnaire-4 (PHQ-4), Graded Chronic Pain Scale (GCPS), and the Jaw Function Limitation Scale (JFLS) (7,78). These questionnaires ultimately assist in identifying potential barriers to treatment response, contributors to chronicity, and targets for further intervention. Positive findings may indicate referral to a qualified mental health professional as part of the treatment plan.
Physical examination
The role of the physical examination is to confirm or reject the diagnosis of TMD in patients suspected based on historical findings. However, even in patients with symptoms highly suggestive of TMD, ENT surgeons must firstly exclude primary causes of otalgia through inspection of the external auditory canal (EAC) and tympanic membrane with otoscopy, where a standard evaluation of its colour and mobility and for the presence of scarring or perforation is performed. Additional examination for any cranial nerve dysfunction and abnormalities on nasopharyngoscopy is paramount to avoid a missed diagnosis of a head and neck lesion that may explain the patient’s pain and require urgent intervention (53,59,75).
The TMJ, oral cavity, and masticatory muscles should then be assessed using inspection and palpation (51,64). Facial asymmetry and mild deviation of the chin on inspection may be consistent with TMD, however, considerable swelling, erythema, or deviation indicate alternative diagnoses (59,79). Inspection of the oral cavity may reveal features consistent with bruxism such as worn incisal edges, flattened occlusal surfaces of the molar teeth, and scalloping of the lateral borders of the tongue (60). The essential examination criteria for the diagnosis of TMD is the elicitation of familiar pain—which is like or akin to the otalgia the patient has been experiencing—on palpation of the muscles of mastication and active opening of the jaw (7). Studies have demonstrated the correlation between otalgia from TMD and more severe tenderness over muscles including the temporalis, masseter, geniohyoid, digastric, sternocleidomastoid, trapezius, posterior cervical muscles, and medial and lateral pterygoids (17,30,40,43,65,79). However, the DC/TMD states that only the temporalis and masseter muscles are reliable, with other locations such as the lateral pterygoid and palpation of the posterior TMJ through the EAC commonly tender in unaffected patients, resulting in false positives (7,80). In addition to familiar pain on jaw opening, patients with TMD may exhibit abnormal mandibular movement, decreased range of motion, or clicking/popping noises. However, as previously described, this tends to be less common amongst the pain-related TMD population and instead represents a patient experiencing a TMJ joint disorder (37,43,79).
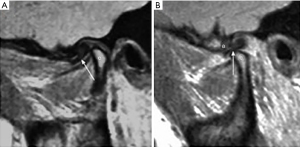
Investigations
As TMD is a clinical diagnosis, few studies explore the utility of diagnostic studies in otalgia from TMD. Nevertheless, there remains a role for imaging in certain instances (81). One such scenario is where primary otalgia has been excluded but no clear secondary cause of otalgia, including TMD, can be confidently diagnosed (82). ENT surgeons can utilise imaging in patients suspected of having severe intra-articular TMD based on clinical history or examination findings including abnormal mandibular movement, decreased range of motion, or clicking/popping noises. Imaging is also of particular importance in selected patients with persistent symptoms despite conservative management who may require referral to oral and maxillofacial surgeons for potential operative intervention. Whilst plain radiography can identify any acute fractures, dislocations, or severe degenerative disease, the more useful imaging modalities for detecting subtle degenerative changes and soft-tissue abnormalities are computed tomography (CT) and magnetic resonance imaging (MRI), respectively (59). These may reveal alternate pathology or increase the likelihood of otalgia from TMD by evidencing exposure of bone, overgrowth of synovium, or internal derangement of the joint including intra-articular effusion or a malpositioned articular disc (Figure 3) (83,84).
The ENT surgeon in the multidisciplinary team
Although ENT surgeons will not personally initiate surgical treatment once the diagnosis of TMD has been made, they are integral in commencing conservative management and involving a multidisciplinary care team (12). Non-operative treatment modalities should be offered to the patient in the first instance and include patient counselling, dietary modification, stress-reduction techniques, pharmacotherapy (such as non-steroidal anti-inflammatory drugs, muscle relaxants, and intra-articular injections), and early referral to a physiotherapist for muscular massage and provision of TMJ mobilisation and stability exercises (85). The detailed aspects and evidence surrounding these approaches are outside the scope of this study and are not discussed here. Still, it is important to highlight that these conservative therapies have been repeatedly evidenced to significantly improve or resolve the symptoms of TMD, including otalgia (26,38,86,87).
The aetiology of otalgia from TMD is multifactorial and the ENT surgeon should acknowledge the beneficial role of collaborating with other healthcare disciplines (52). With the substantial correlation between dental malocclusion and bruxism and TMD defined in the literature, referral to a dentist or orthodontist for a more detailed assessment of dentition and provision of an occlusal appliance where indicated is critical (88). Kutilla et al. (88) demonstrated through a randomised-control study that TMD patients who received a stabilisation splint had a statistically significant reduction in the intensity of secondary otalgia whilst the control group did not. However, it is important to note that evidence on splint therapy to manage TMD symptoms and bruxism from available randomised control studies remains mixed and further studies are required (89,90). Dentists are still in a valuable position where routine follow-up facilitates the regular review of treatment adherence and degree of symptom improvement as well as the identification of those who may require further intervention. As emphasised as part of the clinical evaluation, the psychological component of otalgia from TMD must not be neglected, particularly in patients with chronic symptoms or in those where initial therapy has been unsuccessful. Failure to appropriately address stress and anxiety as a contributing factor and consequences of TMD can negatively influence treatment adherence and overall outcomes. In these patients, ENT surgeons should take an active role in suggesting to the patient’s primary care physician or independently making the referral to a qualified mental health professional such as a psychologist or psychiatrist (7,91).
In scenarios where conservative management is ineffective, patients are suffering from severe pain or impacted quality of life, or if severe intra-articular disease is suspected, the ENT surgeon should coordinate imaging and referral to an oral and maxillofacial surgeon for surgical consideration (58). Surgical approaches depend on the type of TMD and severity of articular changes and include TMJ arthrocentesis, arthroscopic lavage, arthroplasty, discectomy, condylar surgery, and total joint replacement. Additionally, in patients suffering from otalgia and/or other orofacial symptoms but where TMD and other ENT pathologies are ruled out, ENT surgeons should consider the referral to other clinicians including neurologists and chronic pain specialists to generate a list of potential differential diagnoses (50).
Strengths and limitations
The primary strength of this review related to its comprehensive and exhaustive nature as facilitated by a broad research question and inclusion of many studies. As a result, evidence from the perspective of the numerous specialities and locations typically involved in the care of patients from TMD was incorporated. However, as this was not strictly a systematic review, the quality of evidence is prone to bias from subjectivity and a lack of critical appraisal.
Conclusions
ENT surgeons should maintain a high index of suspicion for TMD in patients presenting with otalgia at their clinics. The diagnosis of TMD can be made easily using the TMD-pain screener based on the presence of otalgia modified by movement of the jaw and elicitation of familiar pain on palpation of the temporalis and masseter muscles. Still, it is the role of the ENT surgeon to also consider and exclude alternative or co-existing causes of otalgia in these patients, particularly head and neck malignancy. To ensure the alleviation of the patient’s symptoms, ENT surgeons are responsible for commencing conservative management and involving a multidisciplinary care team of physiotherapists, dental practitioners, mental health professionals, and oral and maxillofacial surgeons.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-23-42/rc
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-42/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-42/coif). C.M. serves as an unpaid Editorial Board Member of the Australian Journal of Otolaryngology from November 2022 to October 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Taziki MH, Behnampour N. A study of the etiology of referred otalgia. Iran J Otorhinolaryngol 2012;24:171-6. [PubMed]
- Taboo ZAA, Buraa MF. Etiology of referred otalgia. Iraqi Postgraduate Medical Journal 2013;12:436-42.
- Bitiniene D, Zamaliauskiene R, Kubilius R, et al. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija 2018;20:3-9. [PubMed]
- Tjakkes GH, Reinders JJ, Tenvergert EM, et al. TMD pain: the effect on health related quality of life and the influence of pain duration. Health Qual Life Outcomes 2010;8:46. [Crossref] [PubMed]
- Musat G, Neaga LF, Enache R. Otologic symptomatology associated with the temporomandibular joint disorder. Romanian Journal of Rhinology 2017;7:215-24. [Crossref]
- Ash MM. Current concepts in the aetiology, diagnosis and treatment of TMJ and muscle dysfunction. J Oral Rehabil 1986;13:1-20. [Crossref] [PubMed]
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 2014;28:6-27. [Crossref] [PubMed]
- Behnoud F, Zandi M. Survey etiologic factor in otalgia and correlation with temporo mandibular joint in patient referred to ENT clinic in Emam Khomani hospital in Hamedan Jul–Nov 2000. MD Dissertation. Hamedan, Iran: Hamedan University of Medical Sciences, College of Medicine 2000;141.
- Ferendiuk E, Zajdel K, Pihut M. Incidence of otolaryngological symptoms in patients with temporomandibular joint dysfunctions. Biomed Res Int 2014;2014:824684. [Crossref] [PubMed]
- Patnaik U, Sood A, K S, et al. Manual of Contemporary Otological Practice. CRC Press, Taylor & Francis Group; 2021.
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Divison, Board on Health Care Services, Board on Health Sciences Policy, Committee on Temporomandibular Disorders. Temporomandibular Disorders: Priorities for Research and Care. Washington (DC): National Academies Press (US); 2020.
- Ramírez LM, Sandoval GP, Ballesteros LE. Temporomandibular disorders: referred cranio-cervico-facial clinic. Med Oral Patol Oral Cir Bucal 2005;10:E18-26. [PubMed]
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. [Crossref] [PubMed]
- LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med 1997;8:291-305. [Crossref] [PubMed]
- Kusdra PM, Stechman-Neto J, Leão BLC, et al. Relationship between Otological Symptoms and TMD. Int Tinnitus J 2018;22:30-4. [Crossref] [PubMed]
- Gaballah K, Alkubaisy A, Baker AA, et al. Revisiting the risk factors for multiple symptoms of temporomandibular disorders: A structured cross-sectional study. Open Dent J 2020;14:503-10. [Crossref]
- Maciejewska-Szaniec Z, Maciejewska B, Mehr K, et al. Incidence of Otologic Symptoms and Evaluation of the Organ of Hearing in Patients with Temporomandibular Disorders (TDM). Med Sci Monit 2017;23:5123-9. [Crossref] [PubMed]
- Effat KG. Otological symptoms and audiometric findings in patients with temporomandibular disorders: Costen's syndrome revisited. J Laryngol Otol 2016;130:1137-41. [Crossref] [PubMed]
- Tuz HH, Onder EM, Kisnisci RS. Prevalence of otologic complaints in patients with temporomandibular disorder. Am J Orthod Dentofacial Orthop 2003;123:620-3. [Crossref] [PubMed]
- Kuttila SJ, Kuttila MH, Niemi PM, et al. Secondary otalgia in an adult population. Arch Otolaryngol Head Neck Surg 2001;127:401-5. [Crossref] [PubMed]
- Lam DK, Lawrence HP, Tenenbaum HC. Aural symptoms in temporomandibular disorder patients attending a craniofacial pain unit. J Orofac Pain 2001;15:146-57. [PubMed]
- Cooper BC, Cooper DL. Recognizing otolaryngologic symptoms in patients with temporomandibular disorders. Cranio 1993;11:260-7. [Crossref] [PubMed]
- Hodges JM. Managing temporomandibular joint syndrome. Laryngoscope 1990;100:60-6. [Crossref] [PubMed]
- Bush FM. Tinnitus and otalgia in temporomandibular disorders. J Prosthet Dent 1987;58:495-8. [Crossref] [PubMed]
- Akhter R, Morita M, Ekuni D, et al. Self-reported aural symptoms, headache and temporomandibular disorders in Japanese young adults. BMC Musculoskelet Disord 2013;14:58. [Crossref] [PubMed]
- Ally M, Moinie A, Lomas J, et al. Aetiology and management options for secondary referred otalgia: a systematic review and meta-analyses. Eur Arch Otorhinolaryngol 2023;280:47-59. [Crossref] [PubMed]
- Mejersjö C, Pauli N. Ear symptoms in patients with orofacial pain and dysfunction - An explorative study on different TMD symptoms, occlusion and habits. Clin Exp Dent Res 2021;7:1167-74. [Crossref] [PubMed]
- Vasconcelos BC, Barbosa LM, Barbalho JC, et al. Ear pruritus: a new otologic finding related to temporomandibular disorder. Gen Dent 2016;64:39-43. [PubMed]
- Luz JG, Maragno IC, Martin MC. Characteristics of chief complaints of patients with temporomandibular disorders in a Brazilian population. J Oral Rehabil 1997;24:240-3. [Crossref] [PubMed]
- Magalhães BG, Freitas JLM, Barbosa ACDS, et al. Temporomandibular disorder: otologic implications and its relationship to sleep bruxism. Braz J Otorhinolaryngol 2018;84:614-9. [Crossref] [PubMed]
- Macedo J, Doi M, Oltramari-Navarro PV, et al. Association between Ear Fullness, Earache, and Temporomandibular Joint Disorders in the Elderly. Int Arch Otorhinolaryngol 2014;18:383-6. [Crossref] [PubMed]
- Allen JD, Rivera-Morales WC, Zwemer JD. Occurrence of temporomandibular disorder symptoms in healthy young adults with and without evidence of bruxism. Cranio 1990;8:312-8. [Crossref] [PubMed]
- Honorato MCM, Tavares LF, Bedaque HP, et al. Otoneurological assessment and quality of life of individuals with complaints of dizziness and temporomandibular disorders: a case-control study. Braz J Otorhinolaryngol 2022;88:S185-91. [Crossref] [PubMed]
- Chew AQA, Saigo L, Yap AU. Is there a comorbid relationship between temporomandibular disorders and otologic signs/symptoms?: An umbrella review. Cranio 2022; Epub ahead of print. [Crossref] [PubMed]
- Chole RA, Parker WS. Tinnitus and vertigo in patients with temporomandibular disorder. Arch Otolaryngol Head Neck Surg 1992;118:817-21. [Crossref] [PubMed]
- Alketbi N, Talaat W. Prevalence and characteristics of referred pain in patients diagnosed with temporomandibular disorders according to the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) in Sharjah, United Arab Emirates. F1000Res 2022;11:656. [Crossref] [PubMed]
- Pekkan G, Aksoy S, Hekimoglu C, et al. Comparative audiometric evaluation of temporomandibular disorder patients with otological symptoms. J Craniomaxillofac Surg 2010;38:231-4. [Crossref] [PubMed]
- Ramirez Aristeguieta LM, Sandoval Ortiz GP, Ballesteros LE, et al. Treatment and follow-up of referred otic symptomatology in 23 patients with diagnosed temporomandibular disorders. Audiol Med 2006;4:73-81. [Crossref]
- de Felício CM, Melchior Mde O, Ferreira CL, et al. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio 2008;26:118-25. [Crossref] [PubMed]
- Campbell CD, Loft GH, Davis H, et al. TMJ symptoms and referred pain patterns. J Prosthet Dent 1982;47:430-3. [Crossref] [PubMed]
- Ward JR, Dolowitz DA, Baukol JL, et al. Painful dysfunction of temporomandibular joint. Arch Intern Med 1963;112:693-8. [Crossref] [PubMed]
- Brookes GB, Maw AR, Coleman MJ. 'Costen's syndrome'--correlation or coincidence: a review of 45 patients with temporomandibular joint dysfunction, otalgia and other aural symptoms. Clin Otolaryngol Allied Sci 1980;5:23-36. [Crossref] [PubMed]
- Adegbiji WA, Olajide GT, Agbesanwa AT, et al. Otological manifestation of temporomandibular joint disorder in Ekiti, a sub-Saharan African country. J Int Med Res 2021;49:300060521996517. [Crossref] [PubMed]
- Atkinson TA, Vossler S, Hart DL. The evaluation of facial, head, neck, and temporomandibular joint pain patients. J Orthop Sports Phys Ther 1982;3:193-9. [Crossref] [PubMed]
- Bonjardim LR, Gaviao MB, Carmagnani FG, et al. Signs and symptoms of temporomandibular joint dysfunction in children with primary dentition. J Clin Pediatr Dent 2003;28:53-8. [Crossref] [PubMed]
- Toller MO, Juniper RP. Audiological evaluation of the aural symptoms in temporomandibular joint dysfunction. J Craniomaxillofac Surg 1993;21:2-8. [Crossref] [PubMed]
- Sobhy OA, Koutb AR, Abdel-Baki FA, et al. Evaluation of aural manifestations in temporo-mandibular joint dysfunction. Clin Otolaryngol Allied Sci 2004;29:382-5. [Crossref] [PubMed]
- Machado IM, Pialarissi PR, Minici TD, et al. Relation of the otological symptoms in the temporomandibular dysfunctions. Int Arch Otorhinolaryngol 2010;14:274-9.
- Blake P, Thorburn DN, Stewart IA. Temporomandibular joint dysfunction in children presenting as otalgia. Clin Otolaryngol Allied Sci 1982;7:237-44. [Crossref] [PubMed]
- Cooper BC, Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio 2007;25:114-26. [Crossref] [PubMed]
- Ramirez LM, Ballesteros LE, Sandoval GP. Topical review: temporomandibular disorders in an integral otic symptom model. Int J Audiol 2008;47:215-27. [Crossref] [PubMed]
- Porto De Toledo I, Stefani FM, Porporatti AL, et al. Prevalence of otologic signs and symptoms in adult patients with temporomandibular disorders: a systematic review and meta-analysis. Clin Oral Investig 2017;21:597-605. [Crossref] [PubMed]
- Fenton JE, Uzomefuna V, O'Rourke C, et al. Applying the Ts of referred otalgia to a cohort of 226 patients. Clin Otolaryngol 2018;43:937-40. [Crossref] [PubMed]
- Cox KW. Temporomandibular disorder and new aural symptoms. Arch Otolaryngol Head Neck Surg 2008;134:389-93. [Crossref] [PubMed]
- Anwar K, Khan S, Shahabi I, et al. The frequency of involvement of head & neck sites in referred otalgia - An experience at a tertiary care hospital. Pak J Med Sci 2019;35:1138-42. [Crossref] [PubMed]
- Sumitha R, Joseph NA. Referred otalgia - A case series. Asian J Pharm Clin Res 2015;8:343-5.
- Silveira AM, Feltrin PP, Zanetti RV, et al. Prevalence of patients harboring temporomandibular disorders in an otorhinolaryngology department. Braz J Otorhinolaryngol 2007;73:528-32. [Crossref] [PubMed]
- Wright EF, Syms CA 3rd, Bifano SL. Tinnitus, dizziness, and nonotologic otalgia improvement through temporomandibular disorder therapy. Mil Med 2000;165:733-6. [Crossref] [PubMed]
- Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician 2015;91:378-86. [PubMed]
- Kim DS, Cheang P, Dover S, et al. Dental otalgia. J Laryngol Otol 2007;121:1129-34. [Crossref] [PubMed]
- Keersmaekers K, De Boever JA, Van Den Berghe L. Otalgia in patients with temporomandibular joint disorders. J Prosthet Dent 1996;75:72-6. [Crossref] [PubMed]
- Yap AU, Peng BMH, Lim SY, et al. Association of temporomandibular disorders severity with otologic and concomitant pain symptoms in Asian youths. Cranio 2022; Epub ahead of print. [Crossref] [PubMed]
- Maciel LFO, Landim FS, Vasconcelos BC. Otological findings and other symptoms related to temporomandibular disorders in young people. Br J Oral Maxillofac Surg 2018;56:739-43. [Crossref] [PubMed]
- Kitsoulis P, Marini A, Iliou K, et al. Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. BMC Ear Nose Throat Disord 2011;11:5. [Crossref] [PubMed]
- Kuttila S, Kuttila M, Le Bell Y, et al. Aural symptoms and signs of temporomandibular disorder in association with treatment need and visits to a physician. Laryngoscope 1999;109:1669-73. [Crossref] [PubMed]
- Gonzalez YM, Schiffman E, Gordon SM, et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc 2011;142:1183-91. [Crossref] [PubMed]
- Baldursson G, Blackmer ER. Temporomandibular joint symptoms in patients with midfrequency sensorineural hearing loss. Ear Hear 1987;8:63-7. [Crossref] [PubMed]
- Chan SW, Reade PC. Tinnitus and temporomandibular pain-dysfunction disorder. Clin Otolaryngol Allied Sci 1994;19:37o-80. [Crossref] [PubMed]
- Buergers R, Kleinjung T, Behr M, et al. Is there a link between tinnitus and temporomandibular disorders? J Prosthet Dent 2014;111:222-7. [Crossref] [PubMed]
- Ciancaglini R, Loreti P, Radaelli G. Ear, nose, and throat symptoms in patients with TMD: the association of symptoms according to severity of arthropathy. J Orofac Pain 1994;8:293-7. [PubMed]
- Lacerda AB, Facco C, Zeigelboim BS, et al. The impact of tinnitus on the quality of life in patients with temporomandibular dysfunction. Int Tinnitus J 2016;20:24-30. [Crossref] [PubMed]
- Algieri GMA, Leonardi A, Arangio P, et al. Tinnitus in Temporomandibular Joint Disorders: Is it a Specific Somatosensory Tinnitus Subtype? Int Tinnitus J 2017;20:83-7. [PubMed]
- Hilgenberg PB, Saldanha AD, Cunha CO, et al. Temporomandibular disorders, otologic symptoms and depression levels in tinnitus patients. J Oral Rehabil 2012;39:239-44. [Crossref] [PubMed]
- Hernández-Nuño de la Rosa MF, Keith DA, Siegel NS, et al. Is there an association between otologic symptoms and temporomandibular disorders?: An evidence-based review. J Am Dent Assoc 2022;153:1096-103. [Crossref] [PubMed]
- Epstein JB, Jones CK. Presenting signs and symptoms of nasopharyngeal carcinoma. Oral Surg Oral Med Oral Pathol 1993;75:32-6. [Crossref] [PubMed]
- De La Torre Canales G, Câmara-Souza MB, Muñoz Lora VRM, et al. Prevalence of psychosocial impairment in temporomandibular disorder patients: A systematic review. J Oral Rehabil 2018;45:881-9. [Crossref] [PubMed]
- Rugh JD, Woods BJ, Dahlström L. Temporomandibular disorders: assessment of psychological factors. Adv Dent Res 1993;7:127-36. [Crossref] [PubMed]
- Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613-21. [PubMed]
- Eweka OM, Ogundana OM, Agbelusi GA. Temporomandibular pain dysfunction syndrome in patients attending Lagos University Teaching Hospital, Lagos, Nigeria. J West Afr Coll Surg 2016;6:70-87. [PubMed]
- Merino-Galvez E, Merino-Coy G, Gomez-Hervas J. The anterior wall sign: A new tool in the diagnosis of temporomandibular disorders. Indian J Otol 2022;28:235-8. [Crossref]
- Greene CS. Managing patients with temporomandibular disorders: a new "standard of care". Am J Orthod Dentofacial Orthop 2010;138:3-4. [Crossref] [PubMed]
- Pulickal GG. Imaging Approach to Otalgia. Springer International Publishing; 2021:45-8
- Weissman JL. A pain in the ear: the radiology of otalgia. AJNR Am J Neuroradiol 1997;18:1641-51. [PubMed]
- Bag AK, Gaddikeri S, Singhal A, et al. Imaging of the temporomandibular joint: An update. World J Radiol 2014;6:567-82. [Crossref] [PubMed]
- Ahmed N, Poate T, Nacher-Garcia C, et al. Temporomandibular joint multidisciplinary team clinic. Br J Oral Maxillofac Surg 2014;52:827-30. [Crossref] [PubMed]
- Tozoglu S, Bayramoglu Z, Ozkan O. Outcome of Otologic Symptoms after Temporomandibular Joint Arthrocentesis. J Craniofac Surg 2015;26:e344-7. [Crossref] [PubMed]
- Stechman-Neto J, Porporatti AL, Porto de Toledo I, et al. Effect of temporomandibular disorder therapy on otologic signs and symptoms: a systematic review. J Oral Rehabil 2016;43:468-79. [Crossref] [PubMed]
- Kuttila M, Le Bell Y, Savolainen-Niemi E, et al. Efficiency of occlusal appliance therapy in secondary otalgia and temporomandibular disorders. Acta Odontol Scand 2002;60:248-54. [Crossref] [PubMed]
- Ebrahim S, Montoya L, Busse JW, et al. The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. J Am Dent Assoc 2012;143:847-57. [Crossref] [PubMed]
- Fouda AAH. No evidence on the effectiveness of oral splints for the management of temporomandibular joint dysfunction pain in both short and long-term follow-up systematic reviews and meta-analysis studies. J Korean Assoc Oral Maxillofac Surg 2020;46:87-98. [Crossref] [PubMed]
- Penlington C, Bowes C, Taylor G, et al. Psychological therapies for temporomandibular disorders (TMDs). Cochrane Database Syst Rev 2022;8:CD013515. [PubMed]
Cite this article as: Petrides GA, Fadhil M, Meller C. Otalgia from temporomandibular disorder in Ear, Nose and Throat surgery: a literature review and diagnostic algorithm. Aust J Otolaryngol 2024;7:12.


