A comparison of tonsillectomy techniques: a 10-year retrospective audit of a large regional hospital in Australia
Introduction
Extracapsular tonsillectomy is defined as a surgical procedure that completely removes the palatine tonsils, including its capsule, by dissecting the peritonsillar space between the tonsil capsule and the muscular wall (1). Tonsillectomy remains one of the most common ear, nose and throat (ENT) procedures performed worldwide (2). Recurrent tonsillitis and obstructive sleep apnoea (OSA) are the most common indications for tonsillectomy (3).
Despite being considered a low-risk operation, tonsillectomy in Australian public hospitals had the highest readmission rates in 2017–2018 compared to other frequently performed surgeries (4). Readmissions to hospital are most often due to postoperative haemorrhage, pain and/or fever. Post-tonsillectomy haemorrhage (PTH) can be classified as either primary (within 24 hours of surgery) or secondary (occurring after 24 hours). Rates of primary and secondary PTH have been reported to be 0.2–3.2% and 0.1–9.4%, respectively (5-9).
There is ongoing debate as to which technique yields the best postoperative recovery. Tonsillectomy techniques are traditionally categorised as “cold” (cold steel dissection with suture or diathermy haemostasis) or “hot” (the use of an instrument delivering thermal energy for both dissection and haemostasis such as coblation, bipolar diathermy and Harmonic scalpel) (10).
In Australia, approximately 7 million people (29% of the population) live outside major cities (11). Dubbo Base Hospital is located within Western NSW Local Health District (WNSWLHD) covering an area of 246,676 sq/km, greater than the land size of Great Britain, serving an estimated population of 276,000. Furthermore, 11.1% of the population are Aboriginal and/or Torres Strait Islander people, which is significantly higher than the NSW average of 2.1% (12). Performing tonsillectomies in such regional areas remains challenging due to availability of ENT surgeons and the increased responsibility of general practitioners and emergency physicians in managing its complications. Therefore, identifying the most suitable surgical technique and risk factors for readmission is essential in ameliorating the rates of PTH. This study aims to investigate the rate of PTH with regards to hot and cold tonsillectomy techniques in a regional Australian hospital, and its associated patient demographics. We present the following article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-21-52/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and after being approved by the Research Ethics and Governance Office at Royal Prince Alfred Hospital (X21-0037 & 2021/ETH00257). Informed consent for this retrospective analysis was waived.
A retrospective medical records review was undertaken on all patients who underwent tonsillectomy between January 1, 2010, and September 30, 2020, at Dubbo Base Hospital, a regional hospital in New South Wales, Australia. All procedures were performed by one of four ENT surgeons or by an ENT registrar under the direct supervision of the consultant ENT surgeon. The data on demographics, operation performed, technique used, length of operation, primary and/or secondary haemorrhage encountered, and readmission reasons were all collected.
The procedures performed were divided into tonsillectomy, adenotonsillectomy, and adenotonsillectomy with other operations (i.e., grommet insertion, turbinate reduction and/or septoplasty). All tonsillectomies regardless of technique were extracapsular. The techniques utilised were one of cold steel tonsillectomy and suction diathermy (10W) haemostasis (“cold dissection” tonsillectomy, which will be referred to as “cold tonsillectomy”), monopolar (10W) tonsillectomy with bipolar (12W) haemostasis (“hot dissection” tonsillectomy, which will be referred to as “hot tonsillectomy”), or coblation (7W) tonsillectomy with coagulation (3W) haemostasis (“hot dissection” tonsillectomy which will also be referred to as “hot tonsillectomy”). Sutures were used for haemostasis for cold steel tonsillectomy, with only scant use of suction diathermy if needed. The routine postoperative management of tonsillectomy patients included an overnight stay with multimodal analgesia and follow up in 6 weeks. No tranexamic acid or antibiotics were routinely administered. The minimum age cut off was 10 months old. All patients regardless of age were required to reside within 30 minutes of Dubbo Base Hospital for the first 2 weeks after the operation.
The hospital’s routine management of post tonsillectomy haemorrhage included urgent ENT review and baseline bloods (including group and screen) with administration of intravenous tranexamic acid (if not contraindicated) and antibiotics, and hydrogen peroxide gargles. If the patient did not have any active bleeding, they were admitted overnight for observations, however if they exhibited active bleeding, the patient was taken to the operating theatres for arrest of the haemorrhage with or without blood transfusion.
Statistical analysis
All statistical analyses were performed using IBM’s SPSS Statistics program Version 28. Statistical significance was set at P<0.05. Univariate logistic regression was used to compare the variables between those who had PTH (primary or secondary) and those who did not. Furthermore, multivariate logistic regression was used to assess the association between the independent variables and PTH.
Results
Patient demographics
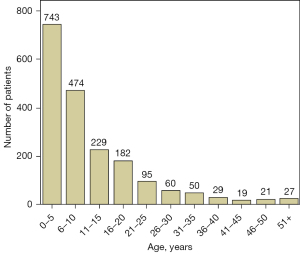
A total of 1,929 patients (902 male and 1,027 female) were identified over the 10-year period, with almost one-third of patients identifying as Aboriginal and/or Torres Strait Islander (Table 1). The youngest patient was 10 months old and the oldest 88 years of age (median 7 years; mean 11.6 years; SD 11.5 years; Figure 1). Individuals with PTH were likely to be older with mean age of 18 years compared to 11 years for those without a PTH. A 1-year increase in age (OR 1.04; 95% CI: 1.02, 1.05; P<0.001) was associated with a significantly increased risk of secondary PTH.
Table 1
| Patient demographics | N [%] |
|---|---|
| Sex | |
| Male | 902 [47] |
| Female | 1,027 [53] |
| Aboriginal and/or Torres Strait Islander | |
| Yes | 625 [32] |
| No | 1,304 [68] |
Operative details
Operations performed were divided into tonsillectomy (28%), adenotonsillectomy (47%), and adenotonsillectomy with other procedures (25%), as outlined in Table 2. Techniques employed were either hot (29%) or cold (71%) tonsillectomy (Table 3). There was no statistically significant association with operation performed or technique employed and secondary PTH (Table 4). The mean operative time was 56 minutes (55 minutes for cold tonsillectomy and 59 minutes for hot tonsillectomy, Table 5).
Table 2
| Operations performed | N [%] |
|---|---|
| Tonsillectomy | 538 [28] |
| Adenotonsillectomy | 912 [47] |
| Adenotonsillectomy + other* | 479 [25] |
*, grommet insertion, turbinate reduction, and/or septoplasty.
Table 3
| Operative techniques | N [%] |
|---|---|
| Cold steel tonsillectomy + suction diathermy haemostasis* | 1,384 [71] |
| Monopolar tonsillectomy + bipolar haemostasis# | 514 [27] |
| Coblation tonsillectomy + coagulation haemostasis# | 31 [2] |
*, cold tonsillectomy; #, hot tonsillectomy.
Table 4
| Variable | OR | 95% CI lower | 95% CI higher | P value |
|---|---|---|---|---|
| Operation performed | 1.11 | 0.83 | 1.50 | 0.48 |
| Technique | 1.41 | 0.84 | 2.37 | 0.19 |
| Duration | 1.01 | 0.99 | 1.12 | 0.36 |
Operation performed, technique employed, and length of operation were not statistically significant for secondary PTH. PTH, post tonsillectomy haemorrhage; OR, odds ratio; CI, confidence interval.
Table 5
| Operation | Mean duration (minutes) |
|---|---|
| Tonsillectomy | 53 |
| Adenotonsillectomy | 52 |
| Adenotonsillectomy + other* | 67 |
*, other operations include grommet insertion, turbinate reduction and/or septoplasty.
Post tonsillectomy haemorrhage
The overall PTH rate was 3.9% (75 patients). The primary PTH rate was 0.7% (13 patients), while the secondary PTH rate was 3.4% (65 patients). The primary and secondary PTH rates were not associated with variations in tonsillectomy technique as detailed in Table 6. Furthermore, the secondary PTH rate for cold tonsillectomy was 3%, while for hot tonsillectomy was 4.2% (P=0.19). Primary PTH was shown to be associated with a five-fold increase in secondary PTH rate (Table 7). Of the 65 patients with secondary PTH, 19 (29%) required operative management, while the rest were treated with medical management and observation.
Table 6
| PTH | Cold steel tonsillectomy + suction diathermy haemostasis | Monopolar tonsillectomy + bipolar haemostasis | Coblation tonsillectomy + coagulation haemostasis | P value |
|---|---|---|---|---|
| Primary | 11 (0.8%) | 2 (0.4%) | 0 (0%) | 0.46 |
| Secondary | 42 (3.0%) | 19 (3.7%) | 4 (12.9%) | 0.19 |
Data is presented as numbers and percentages. PTH, post tonsillectomy haemorrhage.
Table 7
| OR | 95% CI lower | 95% CI higher | P value | |
|---|---|---|---|---|
| Primary PTH | 5.35 | 1.16 | 24.63 | 0.03 |
PTH, post tonsillectomy haemorrhage; OR, odds ratio; CI, confidence interval.
Readmission
The overall readmission rate was 5.5% (106 patients) as shown in Table 8. The readmission rates for hot and cold tonsillectomy were 6.4% and 5.1%, respectively (P=0.27).
Table 8
| Reason | N [%] |
|---|---|
| Pain/dehydration | 43 [41] |
| Haemorrhage | 55 [52] |
| Infection | 8 [7] |
Multivariate analysis
Multivariate analysis showed increasing age (OR 1.04; 95% CI: 1.03, 1.06; P<0.001) and primary PTH (OR 7.73; 95% CI: 1.62, 36.97; P=0.01) to be associated with secondary PTH. Patient’s sex, length of operation, type of operation, technique employed or Aboriginal and/or Torres Strait Islander status were not significantly associated with secondary PTH (Table 9).
Table 9
| Variable | OR | 95% CI lower | 95% CI higher | P value |
|---|---|---|---|---|
| Age* | 1.04 | 1.03 | 1.06 | <0.001 |
| Sex | 0.95 | 0.57 | 1.59 | 0.88 |
| Duration | 1.00 | 0.98 | 1.01 | 0.57 |
| Aboriginal and/or Torres Strait Islander | 0.63 | 0.38 | 1.08 | 0.09 |
| Operation | 1.01 | 0.71 | 1.44 | 0.95 |
| Technique | 1.54 | 0.90 | 2.62 | 0.11 |
| Primary PTH* | 7.73 | 1.62 | 36.97 | 0.01 |
*, a 1-year increase in age and primary PTH are associated with secondary PTH. PTH, post tonsillectomy haemorrhage; OR, odds ratio; CI, confidence interval.
Discussion
Tonsillectomy is one of the most common ENT procedures, with over 30,000 cases performed between 2015 and 2016 in Australia alone (13). Although recurrent tonsillitis and OSA are the most common indications for tonsillectomy, other indications include recurrent peritonsillar abscess and tonsillar malignancy, amongst others (3,14). This procedure is commonly performed concurrently with adenoidectomy (surgical ablation of adenoid tissue), especially for the surgical management of sleep-disordered breathing (15).
This investigation represents the largest Australian regional study with almost two thousand patients over a 10-year period, of which 32% identified as Aboriginal and/or Torres Strait Islander. Performing tonsillectomy in a rural or regional setting has always been challenging due to the scarcity of ENT surgeons and the large catchment area that needs to be covered. Although uncommon, some ENT surgeons visit these regions for 24 to 48 hours to perform such operations before returning to their metropolitan practices (16). Due to these reasons, the complications that arise may need to be initially managed by the local general practitioner or emergency physician.
In this Australian regional hospital, the overall primary and secondary PTH rates were 0.7% and 3.4%, respectively, being comparable to a recent study by Jones et al. who described rates of 1% for primary PTH and 3% for secondary PTH, in a different regional locality in NSW (17). Conversely, in contrast to the National Tonsil Surgery Register in Sweden which analysed over 15,000 patients, our study showed cold steel dissection with suction diathermy to have much lower primary and secondary PTH rates (0.8% and 3.0% compared with 3.4% and 8.8%, respectively) (7).
Primary PTH is generally acknowledged to be caused by inadequate haemostasis during the surgery, however the exact cause of secondary PTH is yet to be definitively established, although the sloughing of eschar, tonsil bed infection, postoperative nonsteroidal anti-inflammatory drug (NSAID) usage, or idiopathic causes have all been postulated (18,19). Furthermore, secondary PTH has been linked with several risk factors such as a history of recurrent tonsillitis, attention deficit hyperactivity disorder (ADHD), excessive intraoperative blood loss and elevated postoperative mean arterial pressure (20,21). Additionally, it has been shown that patients older than 12 years have a 3-fold increase in the likelihood of secondary PTH (22). This study supports a 1-year increase in age to be a risk factor for secondary PTH. This is most likely related to the increased tonsillar scarring, with older patients mostly undergoing tonsillectomy for recurrent tonsillitis (23). However, in this study, secondary PTH was not associated with lengthier operations, an indirect proxy for intraoperative blood loss and haemostasis. Additionally, the mean length of operation of 53 minutes for tonsillectomy could be explained by the fact that the majority of these operations were performed by junior ENT registrars, under the direct supervision of the ENT consultant.
Interestingly, primary PTH was shown to be associated with secondary PTH, which has previously not been reported. The authors recommend a longer observation period for patients who develop primary PTH with the addition of a course of tranexamic acid and hydrogen peroxide gargles whilst an inpatient and on discharge. Furthermore, a shorter postoperative follow up time is recommended.
Readmissions to hospital are most often due to haemorrhage, pain, dehydration and/or fever. The readmission rate at this regional hospital was 5.5%, with no significant difference between hot and cold tonsillectomy. It has been postulated that cold tonsillectomy yields less thermal injury and therefore reduced postoperative pain and dehydration, whereas hot tonsillectomy achieves better haemostasis and shorter operating time (24,25). Cold tonsillectomy was performed for the vast majority (71%) of these procedures with no statistically significant difference in the rate of PTH between cold and hot techniques. Furthermore, although coblation tonsillectomy with coagulation haemostasis had low number of patients, it resulted in 4 times as many secondary PTH when compared to the other two techniques. This may have been a possible reason why this technique has not been utilised more often in this hospital.
Limitations
One of the main limitations of this study is that of retrospective audits; their inherent risk for bias. For example, patient and surgeon factors could in turn influence the technique used for the operation. Secondly, over seventy percent of cases were combined with other procedures such as adenoidectomy, grommet insertion, turbinate reduction, and septoplasty. This can skew results as performing more procedures would naturally take more time. Conversely, allowing more time for haemorrhages to declare themselves ensures adequate intraoperative haemostasis. Finally, although most operations were performed by the junior ENT registrar under the direct supervision of the consultant, exact data on the primary operator was not available which could influence factors such as PTH rate and operative time.
Conclusions
The primary and secondary post tonsillectomy haemorrhage rates in this regional Australian hospital was 0.7% and 3.4%, respectively, with no significant difference between hot and cold tonsillectomy techniques. There was also no significant difference between Indigenous and non-indigenous populations. Increasing age and primary post tonsillectomy haemorrhage were associated with secondary post tonsillectomy haemorrhage and hence the authors recommend closer observation for these patients.
Acknowledgments
The authors would like to sincerely thank Dr. Gary Low for his valuable statistical contribution.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-21-52/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-21-52/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-21-52/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-21-52/coif).The authors have no conflict of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and after being approved by the Research Ethics and Governance Office at Royal Prince Alfred Hospital (X21-0037 & 2021/ETH00257). Informed consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mitchell RB, Archer SM, Ishman SL, et al. Clinical Practice Guideline: Tonsillectomy in Children (Update). Otolaryngol Head Neck Surg 2019;160:S1-S42. [Crossref] [PubMed]
- Derkay CS, Darrow DH, Welch C, et al. Post-tonsillectomy morbidity and quality of life in pediatric patients with obstructive tonsils and adenoid: microdebrider vs electrocautery. Otolaryngol Head Neck Surg 2006;134:114-20. [Crossref] [PubMed]
- Patel HH, Straight CE, Lehman EB, et al. Indications for tonsillectomy: a 10 year retrospective review. Int J Pediatr Otorhinolaryngol 2014;78:2151-5. [Crossref] [PubMed]
- Australian Institute of Health and Welfare 2019. Admitted patient care 2017-2018: Australian hospital statistics. Health services series no. 90. Cat. no. HSE 225. Canberra: AIHW, 2019.
- Windfuhr JP, Chen YS, Remmert S. Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients. Otolaryngol Head Neck Surg 2005;132:281-6. [Crossref] [PubMed]
- Baugh RF, Archer SM, Mitchell RB, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg 2011;144:S1-30. [Crossref] [PubMed]
- Söderman AC, Odhagen E, Ericsson E, et al. Post-tonsillectomy haemorrhage rates are related to technique for dissection and for haemostasis. An analysis of 15734 patients in the National Tonsil Surgery Register in Sweden. Clin Otolaryngol 2015;40:248-54. [Crossref] [PubMed]
- Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope 2007;117:717-24. [Crossref] [PubMed]
- Tran AHL, Chin KL, Horne RSC, et al. Hospital revisits after paediatric tonsillectomy: a cohort study. J Otolaryngol Head Neck Surg 2022;51:1. [Crossref] [PubMed]
- Liu G, Xiao C, Zhou X, et al. Plasma Ablation vs Other Hot Techniques for Tonsillectomy: A Meta-analysis. Otolaryngol Head Neck Surg 2020;163:860-9. [Crossref] [PubMed]
- Australia's Health 2018 Australia's Health and Welfare. 2018. Available online: https://www.aihw.gov.au/getmedia/7c42913d-295f-4bc9-9c24-4e44eff4a04a/aihw-aus-221.pdf. Accessed 4th April 2022.
- Western NSW Local Health District. 2015. Available online: https://wnswlhd.health.nsw.gov.au/our-organisation/our-story/welcome. Accessed 01/04/2022.
- Kwok MM, Subramaniyan M, Rimmer J, et al. Post-tonsillectomy haemorrhage in Australia—a multivariable analysis of risk factors. Aust J Otolaryngol 2018;1:2. [Crossref]
- Wetmore RF. Surgical management of the tonsillectomy and adenoidectomy patient. World J Otorhinolaryngol Head Neck Surg 2017;3:176-82. [Crossref] [PubMed]
- Pynnonen M, Brinkmeier JV, Thorne MC, et al. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev 2017;8:CD004619. [Crossref] [PubMed]
- Macfarlane PL, Nasser S, Coman WB, et al. Tonsillectomy in Australia: an audit of surgical technique and postoperative care. Otolaryngol Head Neck Surg 2008;139:109-14. [Crossref] [PubMed]
- Jones A, Grant A, Saputra L, et al. Tonsillectomy in regional Australia: management and outcomes. Aust J Otolaryngol 2021;4:41. [Crossref]
- Liu JH, Anderson KE, Willging JP, et al. Posttonsillectomy hemorrhage: what is it and what should be recorded? Arch Otolaryngol Head Neck Surg 2001;127:1271-5. [Crossref] [PubMed]
- Ikoma R, Sakane S, Niwa K, et al. Risk factors for post-tonsillectomy hemorrhage. Auris Nasus Larynx 2014;41:376-9. [Crossref] [PubMed]
- Myssiorek D, Alvi A. Post-tonsillectomy hemorrhage: an assessment of risk factors. Int J Pediatr Otorhinolaryngol 1996;37:35-43. [Crossref] [PubMed]
- Spektor Z, Saint-Victor S, Kay DJ, et al. Risk factors for pediatric post-tonsillectomy hemorrhage. Int J Pediatr Otorhinolaryngol 2016;84:151-5. [Crossref] [PubMed]
- Tomkinson A, Harrison W, Owens D, et al. Risk factors for postoperative hemorrhage following tonsillectomy. Laryngoscope 2011;121:279-88. [Crossref] [PubMed]
- Parker NP, Walner DL. Trends in the indications for pediatric tonsillectomy or adenotonsillectomy. Int J Pediatr Otorhinolaryngol 2011;75:282-5. [Crossref] [PubMed]
- Magdy EA, Elwany S, el-Daly AS, et al. Coblation tonsillectomy: a prospective, double-blind, randomised, clinical and histopathological comparison with dissection-ligation, monopolar electrocautery and laser tonsillectomies. J Laryngol Otol 2008;122:282-90. [Crossref] [PubMed]
- Leinbach RF, Markwell SJ, Colliver JA, et al. Hot versus cold tonsillectomy: a systematic review of the literature. Otolaryngol Head Neck Surg 2003;129:360-4. [Crossref] [PubMed]
Cite this article as: Bigdeli R, Jabbour J, Budiono G, Agostinho N, Grassby J, Sirigiri R, Ridha H. A comparison of tonsillectomy techniques: a 10-year retrospective audit of a large regional hospital in Australia. Aust J Otolaryngol 2022;5:13.