The early history and development of endoscopic sinonasal surgery in Australia: 1985–2005
Introduction
When endoscopic sinus surgery was introduced to Australia in 1986 it was severely criticized by Australian Otolaryngologists as being unproven, a new fad, dangerous and specious. In fact none of those criticisms were true. Endoscopic sinus surgery had been researched and practiced in Europe particularly in Germany and Austria since the 1950’s and 1960’s. However it was new to the Anglophone countries.
Discussion
It was Walter Messerklinger (Figure 1) working in the city of Graz, the capital of the Austrian state of Styria who performed the basic research and developed the surgical principles that would later become known as the Messerklinger technique of endoscopic sinus surgery (1).
From the 1950’s and 1960’s Messerklinger in his Department mapped the mucus transport routes in the nose on cadavers whose cilia continued to beat for 48 hours after death thus providing an excellent model for this type of research. He carefully noted using Indian ink particles that the maxillary sinus mucus flow was always towards the natural ostium and then backwards through the middle meatus to the posterior nasal space. These observations explained the failure of traditional gravitational surgical techniques such as inferior meatal antrostomies and Caldwell-Luc procedures. The essential issue was to clear and facilitate drainage towards the natural ostia.
Messerklinger in the 1960’s initially using a modified cystoscope and operating under local anaesthetic developed the technique of operating in a near bloodless field and performing surgery that was tailored to each individual depending on the cause of the obstruction and what was required to establish normal ventilation of the sinuses. Thus the surgery was minimalist in nature and concept.
Further Messerklinger developed the theory that the major sinuses such as the frontal and maxillary sinuses were dependent sinuses, namely dependent on a clear anterior ethmoid cell structure in the middle meatus. This middle meatal zone, later termed ‘the ostiomeatal unit’ was originally coined by Naumann (2) and popularized by David Kennedy in the United States.
The Messerklinger technique changed operations on the frontal sinus into operations on the frontal recess and operations on the maxillary sinus into operations on the ethmoidal infundibulum.
In other European centres various workers were developing similar concepts most prominent among them was Professor Malte Wigand (3) from Erlangen and Wolfgang Draf (4) from Fulda, both in Germany. Draf utilized a combination of rigid telescopes and the operating microscope to drill out the frontal sinus in recalcitrant cases and Malte Wigand introduced an alternative parallel school of endoscopic surgical concepts or functional compartment surgery utilizing wider surgical resection. He used both headlight and suction endoscopy in a gun-like instrument with a handle arrangement opening up the sphenoid first and then performing a retrograde resection from posterior to anterior. Disease was pursued and removed rather than left to resolve spontaneously unlike the Messerklinger ventilation concept.
These early diagnostic and surgical possibilities were given a tremendous thrust forward by Professor H. H. Hopkins’ development of miniaturized telescopes at Reading University between 1951 and 1956 in the UK and the development of the EMI scan in the early 1970’s by Sir Godfrey Hounsfield at Hayes, West London, which was the first computed tomography (CT) scanner.
The introduction of endoscopic sinus surgery to the English-speaking world was hampered by the fact that Messerklinger did not speak English and delivered his lectures to European audiences in his native tongue of German. His young Assistant, Heinz Stammberger (Figure 1), who had spent a year in the United States spoke English perfectly but was unknown outside the Graz department.
David Kennedy, an ENT surgical Resident at Johns Hopkins Medical School in Baltimore US was asked to review the newly published English edition ‘Endoscopy of the Nose’ by Messerklinger in 1978 (1) and immediately realized the importance of this new technique and made it his mission to learn and propagate this new surgical field.
It was through the influence of Heinz Stammberger and David Kennedy that the Messerklinger School of endoscopic diagnosis and surgery became adopted and established in Australia.
Draf did speak English as he was married to Julia, a British anaesthetist. He was invited to Adelaide to attend the AGM of the RACS in May 1986. This was the first time that the use of nasal endoscopes had been discussed in Australia. Only 6 or 7 participants attended his small instructional session in a side room. He advocated the use of a sucker irrigator attached to a telescope thus following the Wigand School of endoscopic surgery rather than Messerklinger’s.
At that session he spoke of canine fossa puncture to the antrum and frontal sinus inspection through an incision in the eyebrow using a supraorbital nerve block. He advocated the use of the inferior meatus in children because of dangers to the developing dentition. He also advocated as a further departure from the Messerklinger School an inferior meatal antrostomy as well as a middle meatal opening because of recurrent and persistent disease. He described the use of an inferior meatal antrostomy prosthesis, rather like a large grommet, made by Xomed which he inserted into the antrostomy for 3 weeks to 2 months. He described his frontal sinus drilling technique (Draf 1, 2, 3) using a microscope and drill.
At this session, the author of this article asked Draf if he could visit him in Fulda which he did later that year in the week of 3 August, 1986. Draf, as always, was most gracious in his hospitality and after days of teaching sent the author home with a full set of telescopes and surgical instruments.
Endoscopic surgery then commenced at the Royal Victorian Eye and Ear Hospital on the author’s return from Fulda and the Hospital rapidly acquired their own equipment. Total and generous support was given by the Hospital for the advancement of this technique and diagnostic system. This reinforced the importance of the major teaching hospitals being in the vanguard of the development of new surgical innovations and systems.
At this time, tomography was used at the Royal Victorian Eye and Ear Hospital for radiological diagnosis before CT scans became available. Tomograms, although vastly superior to plain sinus X-rays, were poor in defining the detailed sinus anatomy so important in this surgery for the avoidance of complications. However they did show, although somewhat blurred, the ethmoidal infundibulum and osteomeatal complex and thus the precise diagnosis of obstruction was possible.
The surgery at the hospital was initially carried out with the use of a Wittmoser side arm attached to a beam splitter placed on the eye-piece of the telescope (Figure 2) so that an observer could view the surgery. The observer standing on the opposite side of the table to the surgeon held the eye-piece of the side arm with his right hand and supported the weight of the bulky side arm with his left hand. The system, despite its awkwardness, was effective. In 1987 the hospital purchased the first of the miniaturized cameras that came on the market trialing a Stryker, later to be replaced with the single chip Richards.

From July 26–31, 1987 the 7th British Academic Conference in Otolaryngology took place in Glasgow, Scotland. On Thursday July 30, Stammberger conducted an instructional session on ‘Endoscopy of the Sinuses’ and although it was poorly attended with only a dozen or so attendees it gave the author an opportunity to invite him to speak in Melbourne.
The 37th General Scientific Meeting of the Otolaryngological Society of Australia was held in Brisbane on its Expo year on 1–6 May1988. This meeting was held as a joint meeting with the RACS; the Royal Australian College of Anaesthetists and the Royal Australian and New Zealand College of Ophthalmologists. Russell Bird, Otolaryngologist, Brisbane, was the Secretary of the Meeting and Karl Storz was organized to sponsor Stammberger who had been invited. At this meeting in the morning session on Tuesday 3 May at the Hilton Hotel Brisbane with John Quayle as Chairman of the Session, Stammberger gave a lecture on ‘Sinus Headache: The Endoscopic Approach’. In the afternoon with Don Jobbins as Chairman, Stammberger lectured on ‘Endoscopic Sinus Surgery’ and later with David Cronin as Chairman he lectured on ‘Endoscopic Diagnosis’.
On Wednesday morning 4 May at the Wesley Hospital, Brisbane, with Don Laing as Chairman, Stammberger gave a lecture on ‘Instrumentation and Techniques of Endoscopic Surgery’. He then performed a practical demonstration in the operating theater at the Wesley Hospital which was beamed through to an audience watching in the Lecture Theatre on TV monitors.
On the following day, Thursday 5 May with Tim Cooney as Chairman, he gave a lecture on ‘Endoscopic Surgery Results and Complications’.
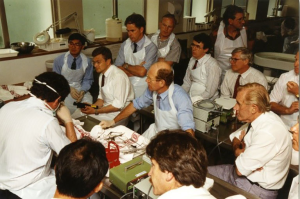
Immediately following this meeting, Stammberger flew to Melbourne and on Monday May 9 and Tuesday May 10, 1988, he conducted the first course on endoscopic sinus surgery in Australia at the Royal Victorian Eye and Ear Hospital (Figure 3).
It consisted of lectures and live operating from the operating theatre suite relayed to the Lecture Room in the Smorgan Wing of the Hospital. Dr. John Harrison was the Anaesthetist and under Stammberger’s request, the surgery was performed under local anaesthetic and neurolept anaesthesia. Despite the effort involved, there was a disappointing number of delegates, only 15–20. Most ENT Surgeons in Melbourne were very skeptical of this new surgery and felt it had little to offer them.
Meanwhile in various other towns and hospitals in Australia numerous other ENT surgeons were purchasing the required equipment and skilling themselves in this surgery. Most notable of those practitioners was Laing in Cairns, Qld, who acquired a masterful competence in the technique and was subsequently to give surgical demonstrations in Australia. These practitioners were handicapped by not belonging to teaching hospitals at that time with the consequent equipment deficiencies particularly in the audiovisual and teaching assistance fields.
The real breakthrough with the acceptance of FESS as the pre-eminent management of chronic sinus disease came with the Sydney Hospital FESS course from 24–28 July, 1989 organized by Henley Harrison of Sydney. The teaching faculty at that course consisted of Stammberger, Kennedy, James Zinreich, a Radiologist from Johns Hopkins Medical School and Gerard Wolf, a Faculty member of the ENT Department in Graz.
The assistant Australian speakers were Laing from Cairns; Raymond Bullock, a Sydney Allergist; Peter Martin, a Sydney Ophthalmologist and Thomas Havas, a Sydney ENT Surgeon. The Organizing Committee were Harrison, Coordinator, Laing, Havas, Paul Ng, Martin Forer, and M. Reynolds.
The four day course consisted of lectures and surgical demonstrations on a cadaver by Stammberger and Kennedy. On the second day, Wednesday 26 July, groups were divided into dissectors and non-dissectors. Dissectors were taken by bus to the Anatomy School at Sydney University.
On Thursday 27 July, live endoscopic operations were relayed from the Maitland operating theatre at Sydney Hospital to the Worrall Lecture Theatre. The surgery was performed by Stammberger, Kennedy and Wolf.
In the laboratory there were 41 dissectors and 30 non-dissectors.
The last day included a special session for Radiologists which may have been the first time such a session had been included in a FESS course. It was conducted by Zinreich and in it he pointed out that coronal CT scans were preferable to axial ones (this was prior to multi-planar reconstructions and radiologists in Australia had believed that reflections from dental amalgam which was present in the majority of patients would prevent satisfactory imaging of the sinuses). He showed that such reflections did not significantly interfere with imaging of the sinuses and after this session coronal cuts started to become the normal plane for sinus imaging—this was a significant advance.
On Wednesday evening October 18, 1989 a Sinus Endoscopy Meeting was held at the Royal Victorian Eye and Ear Hospital when the author’s Sinus Clinic presented the results of the Unit’s first 300 cases of FESS. There were no serious complications but 3 cases of periorbital haematoma and 1 patient with an inflammation of the left medial rectus muscle that settled with antibiotics.
The Otolaryngological Society of Australia AGSM in Melbourne from 18 March 1990 to 23 March 1990 saw little endoscopic sinus surgery content. Most of the rhinology was rhinoplasty with lectures given by the Invited Speaker, Gaylon McCullough from the University of Alabama, Birmingham, USA. At 10:45 am on Friday 2nd March, there was a sole concurrent session on endoscopic sinus surgery in the Rhinology session with Kane giving a lecture on ‘Endoscopic Sinus Surgery’ and Harrison on ‘Follow-up Endoscopic Workshop’.
The next major landmark FESS course held in Australia was the FESS course held in Melbourne on March 25–26, 1991 (Figure 4). This was held at the Royal Victorian Eye and Ear Hospital under the auspices of the Victorian Division of the Australian Society of Otolaryngology Head and Neck Surgery.
The Faculty consisted of Drs. Kennedy, Wolf and Laing. The meeting was sponsored by Stennings and Schering Plough. Dr. Kennedy had come across from Hobart immediately after the ASOHNS AGSM from March 18–22. He had also given excellent lectures in Hobart on endoscopic sinus surgery.
There was nearly 100 Registrants at this meeting and once again the lectures were held in the Lucy Jones Lecture Theatre and the operations were conducted in the Hospital’s basement operating theatres and transmitted to the Lucy Jones Hall. The dissectors were bused across to the Melbourne University Anatomy School.
Lectures were also given by Dr. Paul Nisselle on medico-legal problems with FESS and Dr. John Pike, Radiologist from the Alfred Hospital. Interestingly when Kennedy was making his closing comments, he said that in his mind endoscopic diagnosis was here to stay but he remained unsure about endoscopic surgery.
At this time endoscopic sinus surgery first appeared in the Australian Ear, Nose and Throat literature in 1990. ‘Functional endoscopic sinus surgery (FESS)’ appeared in the Australian Journal of Otolaryngology by Kane (5) and subsequently his article ‘Complications of FESS’ (6).
Australian Otolaryngologists were concerned about the potential for complications with this technique. In 1987 James Stankiewicz reported a complication rate of 29% in his first 90 patients operated on of which 8% were major complications including CSF leaks and ocular mishaps (7). This rate was reduced to 2.2% in the second 90 patients published in 1989 (8).
This was despite Stammberger’s report of the Graz experience of 2,500 cases in February 1986 (9) with no serious complications. Blood losses in that series were minimal and no patients suffered an injury to the ethmoid roof or dura and there were no serious orbital injuries.
The high complication rate experienced by Stankiewicz was not the experience of most practicing endoscopic sinus surgeons so in 1992 Kane instituted a National Survey in Australia amongst 100 practicing endoscopic surgeons. Ten thousand cases were collected with a complication rate of 0.22%. This paper ‘The Australian Experience with FESS and its Complications’ was presented at the 1st International Advanced Course in FESS in Vienna Austria July 29 to Aug 1, 1992 and subsequently published in the Annals of Otolaryngology (10).
In 1994 Mackay carried out a similar survey in the United Kingdom and found similar results (11). These surveys confirmed the view that in most hands the surgical technique was safe but required a new training and a new mindset in the crossover from the traditional method to the minimalist style of endoscopic surgery.
In 1993 the 2nd International Advanced Sinus Symposium was held in Philadelphia, USA. This followed the 1st International Advanced Sinus Symposium held in Vienna, Austria, from July 29 to Aug 1, 1992.
It became apparent in Philadelphia at the meeting that many of the world’s endoscopic sinus surgeons were keen scuba divers. After some discussions and lobbying, Australia was granted the right to host the 3rd International Advanced Sinus Symposium and Cairns was chosen as the venue because of its proximity to the reef for diving and because this area had developed fame as an exotic holiday destination that would attract international faculty members and delegates.
Thus the 3rd International Advanced Sinus Symposium was held from August 14–19, 1995 under the Chairman and Convenor, Kevin J. Kane (Figure 5).
It attracted one of the finest Faculties that had been put together since the introduction of FESS to the English-speaking world.
The International Faculty consisted of David Kennedy, Frederick Kuhn, Valerie Lund, Rodney Lusk, Ian Mackay, Mark May, Dale Rice, Stephen Schaefer, Heinz Stammberger, Gerald Wolf and S. James Zinreich.
A supporting Distinguished Participating Faculty of Claus Bachert, P.A.R. Clement, M. Pais Clemente, Martin Forer, Scott Graham, John T. Kennedy, Toshio Ohnishi, Dharambir Sethi, P. Van Cauwenberg, Johan Van der Merwe and Henny Yeoh attended.
The Australian Executive Committee were Kevin Kane, Convenor, Laurence Ryan, Secretary, David Marty, Treasurer, Henley Harrison and Donald Laing.
Four hundred Delegates attended and plenary sessions, workshops and demonstration cadaveric dissections followed over the 5 days.
A memorable demonstration dissection was held at this meeting on Friday 18 August 1995 when three simultaneous dissections took place on the same stage expertly moderated by Laurie Ryan. Mark May from Pittsburgh demonstrated his 2 handed technique, Frederick Kuhn from Augusta operating off the monitor screen for the first time in Australia demonstrated a dissection of the frontal recess and a dacryocystorhinostomy and Gerald Wolf from Graz demonstrated the closure of a CSF leak.
At this meeting Stammberger introduced the concept of ‘uncapping the egg’ for the first time, namely removing the thin bony remnant of the bulla lamella and frontal cells to open up the frontal sinus. He also introduced the new Storz 45˚ telescope.
At the close of the Symposium it was clear that FESS was here to stay in Australia.
In contradistinction to most countries regrettably Australia never developed an appropriate fee structure for endoscopic sinus surgery merely adopting the old traditional descriptors which by their multiple numbers and operating time differences brought dissatisfaction and discredit to the new technique.
In the later 1990’s many endoscopic sinus courses followed in various States of the country. These included Wormald establishing an annual endoscopic course in Adelaide in 1998 with the Invited International Guest, Dr. David Parsons from the US, and Richard Gallagher, Martin Forer and Ray Sacks commencing a similar annual course at St Vincent’s Hospital in Sydney in the same year. This course was handed over to Professor Richard Harvey to run in 2008 and this course later developed important innovations in skull based surgery. A Rhinology meeting was held in Newcastle on November 15–16, 1997 and chaired by Dr. S. Fernandes.
National courses were also run at this time. The chief amongst these were the two courses run by Smith & Nephew Surgical P/L in Queensland. The first on 12–13 July 1997 was Chaired by Dr. Martin Forer with Faculty Members Drs. Robert Black, Bill Coman and Kevin Kane and run at the School of Anatomy at the University of Queensland, St Lucia, Brisbane (Figure 6). There were 20 Dissectors and 30 non-Dissectors in attendance.

The second for that year was the 2nd Smith & Nephew Spring Meeting at the Novatel Twin Waters Resort at Palm Cove on 27 September to 2 October, 1997. Martin Forer and Kevin Kane spoke on endoscopic sinus surgery. Martin Forer later developed an endoscopic approach to the Pituitary Fossa that was rapidly taken up by international Rhinologists.
In the next decade of these Courses, Seminars and Conferences the crowning achievement for the Society was when the Australian Society of Otolaryngology, Head and Neck Surgery hosted the 11th Congress of the International Rhinologic Society (IRS) at the Sydney Convention and Exhibition Centre from 25–29 October 2005, with Kevin J. Kane as Convenor and President and P. J. Wormald as Scientific Secretary and General Secretary (Figure 7). The IRS meeting was run in conjunction with the AGSM of the Australian Society. A large international Faculty of over 40 attended with 600 Registrants.
Endoscopic sinus surgery was given an enormous boost in Australia when Peter John Wormald was appointed to the South Australian Chair of Otolaryngology Head and Neck Surgery in 1998 (Figure 8). This was a joint appointment between the Adelaide and Flinders University. This was effectively the first Chair in Rhinology in Australia.

P. J. Wormald was medically educated in South Africa and after spending a short period in Glasgow and Cape Town, South Africa, moved to the University of Hong Kong where he developed his interest in Rhinology under Professor Andrew Van Hasselt. He developed an outstanding University Department in South Australia and under his guidance spearheaded research and innovation in all aspects of Rhinology. These have included advances in surgical technique such as his explication of the complex anatomy of the frontal recess and sinus and the 3-dimensional building block approach to its surgery; his development of nasal instrumentation and far reaching establishment of teaching faculties and facilities. These include Rhinology Fellowships since 2000, research projects and advanced endoscopic courses such as the major Vascular Injury Course. He has educated and mentored a whole new generation of Rhinologists both in Australia and overseas.
The development and propagation of endoscopic sinus surgery in Australia has also been assisted by the establishment of the Australasian Rhinologic Society (ARS) in 2003. Under the foresight and drive of P. J. Wormald and Ray Sacks, the Australasian Rhinologic Society [later in 2013 renamed the Australia and New Zealand Rhinologic Society (ANZRS)] was formed with the aim of promoting excellence in clinical rhinology in Australia and New Zealand. The Society was open to medically-trained specialists in both countries as well as appropriate scientists.
The inaugural meeting was held in the Hunter Valley at the Cypress Gardens Motel on June 7–9, 2003 under the Convenorships of Drs. Ray Sacks and Neil Boustred. The author was the inaugural President of the new Society. The second meeting of that Society was held at Lindenderry on the Mornington Peninsula, Victoria, on 12–14 June 2004 with Kane as Convenor and the third in the Barossa Valley in South Australia from 6–8 October 2006 at the Novatel Motel with Wormald as Convenor. There have been annual meetings since and the ANZRS has been a major force in promoting rhinology in Australia.
Australia has pioneered many notable innovations in the technique particularly since the arrival of Wormald. Initially the teaching and practice was to perform the surgery under local anaesthesia. This was purported to give a more bloodless operating field and thus better visualization. The awake patient could also experience pain when pain-sensitive areas such as the fovea and orbit were approached and direct feedback clues could be given to the operating surgeon to alert him of imminent danger. Both Kennedy and Stammberger advocated the use of local anaesthesia in the 1980’s and 1990’s.
However Australia with a heavy influence of expert British anaesthesia with controlled blood pressure and local haemostatic techniques adopted general anaesthesia (GA) as the preferred technique. When the author showed videos of endoscopic sinus surgery at the 1st International Sinus Symposium in Vienna in 1991, the attendees were confounded by the fact that the operations were performed under GA Since then the world has generally operated under GA as the preferred method of anaesthesia as it is more comfortable both for the surgeon and the patient and gave the same operating haemostatic conditions.
Careful preparation of the nose before surgery however was stressed with the placement of materials soaked with vasoconstrictor agents such as cocaine and Co-phenylcaine (Lignocaine-phenylephrine) into the middle meatus and surrounding areas. Direct injections of vasoconstrictor agents such as lignocaine and adrenalin were made into the uncinate process area and often into the sphenopalatine ganglion area either through the nasal cavity or through the palate via the greater palatine foramen. In cases of nasal polyposis or gross infection, pre-operative courses of oral steroids such as prednisolone were prescribed.
Reuben Setliff (12) in the US noted the use of mechanical shavers in long bone and temporomandibular joint arthroscopy. Jack Urban at the House Ear Institute in Los Angeles in the late 1960’s had introduced a power-driven, suction-based rotating instrument for removal of acoustic neuromas. Setliff introduced the idea of using powered instrumentation for intranasal surgery. It became immediately clear to surgeons that powered instrumentation with suction irrigation allowed excellent visualization with clean cutting and minimal mucosal stripping.
The mechanical shaver was rapidly taken up by Australians and its use promoted particularly by Wormald. He championed the Xomed Medtronic ‘straight shot’ shaver which was more powerful and had wider bores in its blades so not only polyps and hypertrophied mucosa could be cleanly cut without stripping, but bone could be removed also. There was constant irrigation to clear the bits, so clogging was avoided and oscillation and speed adjustment was in-built. Material could be collected in a filtration bottle and sent to pathology for histological examination. These powered instruments with suction irrigation also allowed drill bits to be fitted, both straight and angled, which facilitated removal of bone in areas such as the frontal sinus.
A major problem in the early days of endoscopic sinus surgery was post-operative management of the ethmoid cavity. Surgical success depended on the outcome of a well healed middle meatus without adhesions and stenosis. Post-operative suctioning of the middle meatus under local anaesthesia in the office with division of adhesions was a miserable affair which many patients could not tolerate.
In the early days some surgeons recommended excision of the lateral aspect of the middle turbinate to create space and reduce the prospect of adhesions. This was rapidly abandoned as experience showed that this manoeuvre was guaranteed to cause them.
Spaces and stents were tried such as Gelfoam, Silastic stents and Gelfilm initially but all were unsatisfactory and were abandoned. The introduction in the first decade of the 21st Century of Medtronic’s Merogel containing hyaluronic acid inserted into the middle meatus was a major advance in promoting healing. Since then further bio-compatible materials have come on the market which has largely solved this difficult and frustrating problem.
Dr. Chris Brown from Melbourne in 2005 working with researchers from the United States introduced and performed a pilot study of ten patients at the Alfred Hospital Melbourne in expanding the sinus outlets by the use of inflatable balloon Sinuplasty. This gained approval by the US Regulatory Board and a multi-centre trial in both Australia and the United States ensued. Balloon Sinuplasty was based on the use of similar devices in coronary artery disease and other sites and avoided the removal of tissue and bone with the potential possibility of scarring and sequelae.
Paediatric FESS
Australia to its great credit remained very conservative and circumspect with regard to the controversial subject of endoscopic sinus surgery in children. This surgery was taken up and practiced with enthusiasm by some American surgeons such as Rodney Lusk, R. H. Lazar and David Parsons. However endoscopic sinus surgery in children was fraught with problems because of the difficulty of diagnosis when there was no clear cut definition of what chronic sinusitis was in children, the problem with the use of CT scanning and its associated radiation to make the diagnosis and allow planning for surgery, the difficulty of diagnostic endoscopic evaluation and post-surgical aftercare. These difficulties all mitigated against paediatric FESS.
Parsons visited the Royal Children’s Hospital in Melbourne on 8 June 1990 and ran a seminar on paediatric FESS. He advocated minimal FESS in some cases with an uncinectomy and antrostomy. To overcome the problem with post-operative care, he advocated the use of a Gelfilm roll placed into the middle meatus and then this was removed under general anaesthetic after 7 days, toilet to the cavity instituted and a replacement Gelfilm roll inserted.
Many surgeons who initially enthusiastically promoted FESS in children came to modify their position and practice more conservative medical treatment withholding surgery for only very severe cases. There was less controversy for the role of endoscopic sinus surgery in sinusitis with associated complications or in cystic fibrosis, fungal sinusitis and antrochoanal polyps.
To establish the place of endoscopic sinus surgery in children in Australia, a Conference was organized in Sydney by Dr. Tom Havas on ‘Evolving Concepts in Paediatric Rhinology’ from Aug 17–19, 2001, at the Sydney Stamford Plaza, Double Bay. The Keynote Speaker was Wormald and the Honoured Guest, Dr. Victor Bear. A large Faculty of ENT Surgeons, Allergists, Radiologists, Pediatricians and Respiratory Physicians attended.
The introduction of nasal telescopes into otolaryngology in Australia was the greatest advance in the specialty since the development of the Zeiss operating microscope in the 1950’s. It is a source of great pride to Australian Otolaryngology that this technique was taken up so enthusiastically and has spawned a major contribution by them to international Scientific Journals, Conferences and book publications.
This history wishes to record in some detail the early origins and development—the first 20 years—of this technique before with the passage of time it is lost to posterity. To those contemporary surgeons who feel left out of this history, the Author can only apologize. No doubt at some future time, the next 25 years from 2005 will be recorded and they will find their rightful place within it.
Acknowledgments
The author wishes to thank Dr. Henley Harrison for his generous assistance in the preparation of this article.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.01.08). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Messerklinger W. Endoscopy of the Nose. München: Urban and Schwarzenberg, 1978.
- Naumann H. Patholische anatomic der chronischen rhinitis and sinusitis. In: Proceedings VIII International Congress of Otorhinolaryngology. Amsterdam: Excerpta Medica, 1965:12.
- Wigand M. Endoscopic Surgery of the Paranasal Sinuses and the Anterior Skull Base. Jeorg Thieme. New York: Verlag Stuttgart, 1990.
- Draf W. Endonasal micro-endoscopic frontal sinus surgery: The fulda concept. Oper Tech Otolaryngol Head Neck Surg 1991;2:234-40. [Crossref]
- Kane KJ. Functional Endoscopic Sinus Surgery (F.E.S.S.). J Otolaryng Soc Austral 1990;6:299-302.
- Kane KJ. Complications of FESS. Aust J Otolaryng 1992;1:169-72.
- Stankiewicz JA. Complications of endoscopic intranasal ethmoidectomy. Laryngoscope 1987;97:1270-3. [Crossref] [PubMed]
- Stankiewicz JA. Complications in endoscopic intranasal ethmoidectomy: an update. Laryngoscope 1989;99:686-90. [Crossref] [PubMed]
- Stammberger H. Endoscopic endonasal surgery--concepts in treatment of recurring rhinosinusitis. Part II. Surgical technique. Otolaryngol Head Neck Surg 1986;94:147-56. [Crossref] [PubMed]
- Kane K. Australian experience with functional endoscopic sinus surgery and its complications. Ann Otol Rhinol Laryngol 1993;102:613-5. [Crossref] [PubMed]
- Cumberworth VL, Sudderick RM, Mackay IS. Major complications of functional endoscopic sinus surgery. Clin Otolaryngol Allied Sci 1994;19:248-53. [Crossref] [PubMed]
- Setliff RC, Parsons DS. The Hummer. New instrumentation for FESS. Am J Rhinol 1994;8:275-8. [Crossref]
Cite this article as: Kane KJ. The early history and development of endoscopic sinonasal surgery in Australia: 1985–2005. Aust J Otolaryngol 2018;1:7.