Myringoplasty outcomes of Indigenous Australians in the West Kimberley region of Western Australia
Introduction
Indigenous Australian children and adolescents residing in rural locations have a high prevalence of middle ear disease (1,2). Hearing loss associated with chronic suppurative otitis media (CSOM) can adversely affect language and cognitive development which can result in an educational and employment disadvantage, and this in turn has been associated with over-representation in the criminal justice system (3). Approximately 60% of Indigenous children by 2 years of age will have had at least one tympanic membrane (TM) perforation (4).
Myringoplasty aims to prevent otorrhoea and improve hearing loss associated with CSOM by closing the perforation. Previous studies to assess the success rate of myringoplasty in the Australian Indigenous rural and remote populations have demonstrated a lower TM perforation closure rate when compared to non-Indigenous city counterparts (5,6). To the best of our knowledge, there have been no recent reviews of myringoplasty outcomes in the West Kimberley region. In 2000, Mak et al. reported on myringoplasty outcomes in Indigenous Australians in this region (7). Only 68 of 212 patients had complete follow up, and of those 68, a 53% success rate was reported [success was defined as TM closure at more than 6 months with an air-bone gap (ABG) of less than 25 dB]. In a subsequent prospective study of 78 paediatric Indigenous myringoplasty outcomes in Western Australia, complete follow-up was achieved in 78% of ears, but with a similar success rate of 49% (8).
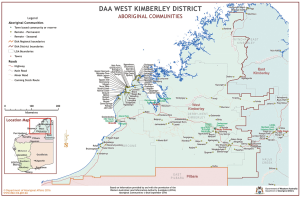
The Kimberley region in far north-western Australia is a vast and sparsely populated region. The estimated population in this area was 38,801 in 2015. Table 1 and Figure 1 demonstrate the geographical and demographic diversity of this region (11). It is serviced by the Kimberley Aboriginal Medical Service (KAMS) and the Western Australia Country Health Services (WACHS). Both organisations employ Ear Nose and Throat (ENT) surgeons, audiologists, anaesthetists and Aboriginal health workers who visit Broome, Derby, Kununurra and surrounding communities. Patients with ENT problems are referred by the local Aboriginal health services and general practitioners to the visiting ENT service. The geographical isolation of the region, mobility of the Indigenous population and the limited number of visits by the ENT service make identification of ear pathology, surgical management, and timely follow up of patients challenging.
The aim of this study was to review the outcomes of myringoplasty surgery performed in the West Kimberley region over the last 10 years, and identify factors associated with surgical and audiological outcomes.
Methods
The study was a retrospective audit of all patients undergoing myringoplasty for a TM perforation between 2004 and 2014 in the West Kimberley region of Western Australia. Ethical approval for this study was provided by WACHS, the Western Australian Aboriginal Health Ethics Committee (WAAHEC), Kimberley Aboriginal Health Planning Forum (KAHPF), and University of Adelaide ethics committee.
An operating theatre database prospectively recording all procedures was interrogated to identify cases at the major regional hospitals in Broome and Derby. The terms “myringoplasty” and “tympanoplasty” were used to search the database. The inclusion criteria were all indigenous patients that underwent a myringoplasty (defined by closure of the TM with graft materials such as temporalis fascia, fat, perichondrium, or composite grafts). Any patient undergoing myringoplasty in conjunction with cholesteatoma or other ear surgery (such as atticotomy, mastoidectomy, ossicular chain reconstruction) were excluded.
Individual patient charts were reviewed for demographic, clinical, operative, and audiometric data. Audiometry was conducted under standardized conditions in hearing booths whenever available. Otherwise audiological testing was performed in the quietest room available with calibrated, noise-insulating over-the-ear or insert headphones.
The primary outcome measures were otoscopic and audiometric. “Success” was defined as closure of the TM and an average air-bone gap (ABG) of less than or equal to 25 dB across 500 Hz, 1, 2, and 4 kHz with a follow-up of at least 6 months post-surgery, in keeping with the Mak et al. studies (7,8).
TM perforation size was divided into 4 grades. Small perforations (Grade 1) were defined as an area less than or equal to 25% of the total surface area of the TM, medium perforations (Grade 2) between 26% and 50%, large perforations (Grade 3) between 51% and 75%, and subtotal perforations (Grade 4) between 76% and 99%. The World Health Organisation (WHO) classification of hearing loss severity was used to grade the magnitude of the ABG (see Table 2) (12). If a patient underwent bilateral myringoplasties then the ear with the greatest pre-operative ABG was used for analysis of “Success”.
Table 2
| Air-bone gap (dB) | Degree of hearing loss |
|---|---|
| <25 | Normal |
| 26–44 | Mild |
| 45–59 | Moderate |
| >60 | Severe |
Results
A total of 327 patients identifying as Indigenous underwent a myringoplasty. There were 38 non-Indigenous myringoplasty patients excluded. There were 419 ears identified during the audit period fulfilling the inclusion criteria. There were 92 patients who underwent bilateral myringoplasties. Patient demographics, perforation characteristics, and pre-operative audiometry data was extracted along with myringoplasty operative technique, graft material, and placement.
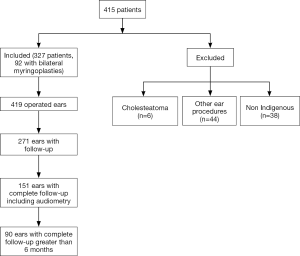
Only 207 patients (representing 271 operated ears) attended follow-up to assess the surgical outcome. This represented an attrition rate of 36.4% of patients (35.3% of operated ears) lost to any recorded follow-up. One hundred and fifty-one of the 271 operated ears had at least 6 months follow-up post-operatively, however 61 (14.6%) of these did not have complete audiometric data. This resulted in 90 operated ears across 73 patients with complete otoscopic and audiometric follow-up sufficient to evaluate the primary end-point (Figure 2) (12).
Patient demographics
The 327 Indigenous patients who had undergone myringoplasty were aged between 4.8 years to 56.5 years. Patients were divided into three groups—young children (less than 8 years of age), older children (8 to 18 years of age) and adults (over 18 years of age). Table 3 demonstrates that more patients were operated on in Derby than in Broome and that there were twice as many female patients as there were male.
Table 3
| Variables | Complete follow-up (n=73 patients, 90 ears), n [%] | Incomplete follow-up (n=254 patients, 329 ears), n [%] | Total (n=327, 419 ears), n(%) | P value |
|---|---|---|---|---|
| Demographicsa | ||||
| Age (years) | NS | |||
| <8 | 22 [30] | 61 [24] | 83 [25] | |
| 8–18 | 41 [56] | 123 [48] | 164 [50] | |
| >18 | 10 [14] | 70 [28] | 80 [24] | |
| Location | <0.001 | |||
| Broome | 12 [16] | 112 [44] | 124 [38] | |
| Derby | 61 [84] | 142 [56] | 203 [62] | |
| Gender | <0.05 | |||
| Female | 53 [73] | 155 [61] | 208 [64] | |
| Male | 20 [27] | 97 [38] | 117 [36] | |
| Unknown | 0 [0] | 2 [<1] | 2 [<1] | |
| Pre-operative perforation statusb | ||||
| Total number of ears | 90 | 329 | 419 | – |
| Location | NS | |||
| Anterior | 23 [26] | 83 [25] | 106 [25] | |
| Posterior | 12 [13] | 26 [8] | 38 [9] | |
| Central | 50 [56] | 156 [47] | 206 [49] | |
| Not recorded | 5 [6] | 64 [19] | 69 [16] | |
| Size | NS | |||
| Grade 1 (<25%) | 13 [14] | 73 [22] | 86 [21] | |
| Grade 2 (25–50%) | 39 [43] | 92 [28] | 131 [31] | |
| Grade 3 (50–75%) | 12 [13] | 33 [10] | 45 [11] | |
| Grade 4 (>75%) | 15 [17] | 79 [24] | 94 [22] | |
| Not recorded | 11 [12] | 52 [16] | 63 [15] | |
| Prior attempts | – | |||
| One+ | 22 [24] | 73 [22] | 95 [23] | |
| Not recorded | 3 [3] | 33 [10] | 36 [9] | |
| Middle ear status | NS | |||
| Dry | 72 [80] | 278 [84] | 350 [84] | |
| Wet | 18 [20] | 51 [16] | 69 [16] | |
| Surgical techniquesb | ||||
| Bilateral surgery | 34 [38] | 150 [46] | 184 [44] | – |
| Approach | NS | |||
| Transcanal | 50 [56] | 169 [51] | 219 [52] | |
| Endaural | 23 [26] | 83 [25] | 106 [25] | |
| Post-auricular | 4 [4] | 17 [5] | 21 [5] | |
| Not recorded | 13 [14] | 60 [18] | 73 [17] | |
| Graft Material | NS | |||
| Cartilage | 28 [31] | 67 [20] | 95 [23] | |
| Composite | 11 [12] | 50 [15] | 61 [15] | |
| Perichondrium | 12 [13] | 20 [6] | 32 [8] | |
| Temporalis Fascia | 35 [39] | 155 [47] | 190 [45] | |
| Fat Plug | 1 [1] | 19 [6] | 20 [5] | |
| Not recorded | 3 [3] | 18 [5] | 21 [5] | |
| Surgical techniquesb | ||||
| Graft placement | NS | |||
| Underlay | 61 [69] | 213 [65] | 274 [65] | |
| Inlay | 24 [27] | 54 [16] | 78 [19] | |
| Overlay | 2 [2] | 11 [3] | 13 [3] | |
| Not recorded | 3 [3] | 51 [16] | 54 [13] | |
Totals less than the overall were due to missing data. a, based on number of patients n=327; b, based on number of ears n=419. NS, not significant.
Preoperative status of the ear and size of perforation
The location of the perforation was defined by its position relative to the handle of malleus. Central perforations were the most common (Table 3). In more than 20% of patients the site of the perforation was not recorded at either the time of booking or time of surgery. With regards to size, the majority were medium perforations followed by subtotal perforations. The size of the perforation was not recorded in 14.8% of patients.
The majority of cases were primary myringoplasties (69%), with 22% being revision cases (n=77 one prior attempt, n=16 two or more prior attempts). The number of prior attempts was not documented in 9% (n=38 ears). The middle ear was dry in 83.5% of operated ears at the time of booking for surgery, with 90.9% dry on the day of surgery.
Pre-operative audiometry
Pure tone audiometry was obtained in 382 (91.2%) ears pre-operatively. However, only 269 ears had air and bone conduction thresholds at 500 Hz, 1, 2 and 4 kHz recorded. In this group, using the WHO classification (Table 2) applied to the surgical ear, 91 of the operated ears had normal hearing preoperatively (33.8%), 153 ears had mild hearing loss (56.9%), 23 ears had moderate hearing loss (8.6%), and 2 ears had severe hearing loss (0.7%). Overall, this group had a mean ABG of 30.1 dB (SD =10.9) and bone conduction thresholds ranged between −10 and 40 dB, with a mean of 6.8 dB (SD =7.3).
As expected, larger perforations were associated with a greater ABG. The mean ABG for subtotal perforations was 35.3 dB (SD =10.8, n=55), with 33.5 dB (SD =11.0, n=38) for large perforations, 29.7 dB (SD =10.6, n=90) for medium perforations, and 24.2 dB (SD =8.1, n=51) for small perforations. A one-way independent groups ANOVA demonstrated a significant effect for perforation size on pre-operative ABG, F(3,230) =11.76, P<0.001. Post-hoc analysis (Tukey HSD) demonstrated subtotal perforations had a greater ABG than medium (P<0.01) and small (P<0.001) perforations. Large (P<0.001) and medium (P<0.05) perforations also had a larger ABG than small perforations. The state of the middle ear did not affect the ABG except in Grade IV perforations, where wet perforations (M =43.0 dB, SD =13.2, n=24) had 11dB worse hearing than dry perforations (M =31.8 dB, SD =7.5, n=70).
Myringoplasty techniques by operated ear
The transcanal approach was the most commonly used technique and the post-auricular approach the least common (Table 3). The surgical approach was not recorded in 17.4% of ears. The most common graft material used was temporalis fascia, followed by cartilage, composite grafts, perichondrium, and fat plugs. Graft material was not recorded in 5% of cases. The majority of grafts were positioned using an underlay technique, followed by the inlay technique. The onlay technique was the least common, and in 13% of cases the method of graft placement was not documented (Table 4).
Table 4
| Technique | Number |
|---|---|
| Transcanal using temporalis fascia placed underlay | 78 |
| Endaural approach using temporalis fascia placed underlay | 67 |
| Transcanal approach using cartilage/composite as an inlay | 55 |
| Transcanal approach using cartilage/composite as an underlay | 29 |
| Endaural approach using cartilage/composite as an underlay | 26 |
| Post-auricular approach using temporalis fascia as an underlay | 17 |
| Other techniques/not recorded | 147 |
Given the high rate of patients lost to follow-up, the demographic, clinical, audiometric and operative data for the complete follow-up sample (n=90 ears) were compared to the remaining operative sample (n=329 ears) lost to complete follow-up. The complete and incomplete follow-up groups differed in terms of demographic variables of location and gender. Derby patients and females were more likely to complete follow-up (see Table 3). The groups did not significantly differ on any other demographic, otoscopic, audiometric, or surgery variable.
Follow-up
Of the 207 patients (271 ears) with documented follow-up, clinical review was undertaken at a median of 7.6 months (range, 10 days to 110 months). Of the 271 operated ears, 33 ears (12.2%) were seen less than 2 months post-surgery, 84 (31.0%) between 2 to 6 months, 44 (16.2%) between 6 to 12 months, 57 (21.0%) between 12 to 24 months, and 50 ears (18.5%) seen over 2 years. The date of follow-up was not clearly recorded for three cases.
Complete audiometric follow-up for any ear was defined as patients with a calculated ABG for 500 Hz, 1, 2, and 4 kHz both pre- and post-surgery. This was found for n=152 ears. A further n=62 ears with incomplete audiometry were excluded. Complete otoscopic and audiometric follow-up at least 6 months post-surgery was available for n=90 ears (n=73 patients). This means only 21.5% of the operated ears (22.3% of patients) had adequate follow-up data to evaluate the main outcomes.
Outcome measures
There were three outcome measures of interest: success, closure of the TM perforation, and hearing improvement at least 6 months post-surgery. To maintain consistency and comparability with the studies published by Mak et al. (7,8) success was defined as closure of the TM with an ABG of less than 25 dB at greater than 6 months. Hearing improvement was defined as a reduction in ABG of 10 dB or more. Univariate odds ratio analyses for the outcomes are presented in Table 5. A dry middle ear at the time of booking surgery was greater than 5 times more likely to succeed than a wet middle ear. Female gender [odds ratio (OR) =4.69, 95% confidence interval (CI), 1.23–17.93], small to medium perforation size (OR =3.24, 95% CI, 1.13–9.33), and normal preoperative ABG (OR =6.77, 95% CI, 1.45–31.62) were significantly more likely to be associated with TM closure. With regards to hearing improvement, no significant associations were found. Notably however, no wet ear at the time of booking recorded an improvement in hearing, which explains why the odds ratio was not calculable.
Table 5
| Variables (reference) | Success (29%) | Tympanic membrane closure (39%) | Hearing improvement (29%) |
|---|---|---|---|
| Age (<8 years) | 0.77 (0.24–2.51) | 0.72 (0.25–2.09) | 2.71 (0.93–7.81) |
| Location (Broome) | 0.50 (0.40–5.82) | 1.27 (0.36–4.47) | 1.85 (0.52–6.63) |
| Gender (female) | 2.45 (0.63–9.55) | 4.69* (1.23–17.93) | 2.06 (0.60–7.07) |
| Size of perforation (small/medium) | 3.31 (0.99–11.02) | 3.24* (1.13–9.33) | 1.39 (0.49–3.91) |
| Prior attempts (nil) | 1.10 (0.37–3.24) | 0.70 (0.26–1.87) | 1.40 (0.45–4.35) |
| Pre-operative ABG (<25 dB) | 9.04* (1.13–71.97) | 6.77* (1.45–31.62) | 1.54 (0.46–5.21) |
| Middle ear (dry) | 5.24* (1.52–18.04) | 2.96 (0.88–9.95) | Not calculable |
| Approach (transcanal) | 0.54 (0.19–1.48) | 0.61 (0.23–1.56) | 0.94 (0.35–2.55) |
| Graft (fascia/perichondrium) | 1.45 (0.57–3.70) | 0.94 (0.40–2.23) | 0.59 (0.23–1.53) |
| Placement (underlay) | 0.73 (0.27–1.95) | 0.88 (0.35–2.25) | 1.63 (0.56–4.68) |
Data are presented as odds ratios (95% confidence intervals). *, P<0.05. ABG, air-bone gap.
Table 6 presents the percentage of operated ears classified according to the WHO hearing loss classification both pre and post-surgery. Just over a quarter of ears had normal hearing pre-operatively, however normal hearing was seen in almost half of the operated ears at greater than 6 months.
Table 6
| Hearing level (ABG) | Pre-operative (%) | Post-operative (%) |
|---|---|---|
| Normal (<25 dB) | 27.8 | 46.7 |
| Mild (25–40 dB) | 54.4 | 32.2 |
| Moderate (40–60 dB) | 17.8 | 21.1 |
| Severe (>60 dB) | 0 | 0 |
ABG, air-bone gap.
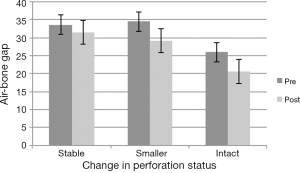
Hearing outcomes were also classified by change in perforation status (see Figure 3). Hearing was significantly improved by 5.4 dB (SD =11.2) when the perforation was closed (n=31), t(30) =2.70, P<0.05. A reduction in perforation size post-surgery was associated with a 5.2 dB (SD =13.1) reduction in ABG (n=21), but this just failed to reach statistical significance. When the perforation remained stable or enlarged, a non-significant change of 2 dB was observed (n=30).
Discussion
Chronic middle ear disease is widely prevalent in Indigenous Australians. Unfortunately, despite the ongoing awareness of its significant morbidity, there are limited studies evaluating the efficacy of interventional strategies offered to this population. The last published study reviewing myringoplasty outcomes in Indigenous Australians residing in remote Western Australia was over a decade ago (8). Our study is the most recent retrospective appraisal of myringoplasty practise and outcome in the West Kimberley region of Western Australia.
Closure of TM 6 or more months after surgery was seen in 39% of ears in our study. This figure rises to 71% if closure and reduction of perforation size are combined. These results are in contrast to the study by Mak et al. (7), which found a success rate of 49% with 51% hearing improvement, and a mean gain of 9 dB. Hearing improvement of greater than or equal to 10 dB in ABG was demonstrated in 29% of cases in our study in comparison to reported average hearing gain of 9.14 dB in the UK audit study for primary successful myringoplasty and 9.16 dB for unsuccessful primary myringoplasty (13). Closure or reduction in perforation size was comparable with Mak et al. reporting 72% (7). From our analysis, it appears that closure rates have not significantly improved in the last decade for Indigenous Australians in the West Kimberley region.
Our closure rate was lower than international metropolitan studies, including the 10-year UK myringoplasty study with a reported closure rate of 89.5% and the Swedish myringoplasty outcomes study with a closure rate of 88.5% (13-16). This is probably representative of the severity of underlying middle ear disease in Indigenous Australians, and the possible difference in ear anatomy and socioeconomic status that predisposes this population to TM perforations.
Our study identified a significant issue with patients lost to follow up, with less than 22% of the original operative cohort completing clinical and audiometric follow-up for more than six months. This is less than the 32% follow-up rate observed by Mak et al. (7), which was obtained with considerable effort, by community health nurses, Aboriginal health workers, and the later visiting ENT teams to locate missing patients. More encouragingly, a follow-up rate of 78% was obtained in a subsequent prospective study conducted by Mak et al. (8). The low follow-up numbers are more than likely multifactorial.
Western Australia has the third highest number of Indigenous residents, and the third highest percentage of Indigenous residents in Australian states (17). WA (41%) is only second to NT (81%) in terms of the percentage of Indigenous individuals living in remote or very remote areas. Despite this and being the largest state of Australia, all specialist ENT services are based in Perth. While visiting specialist trips are more frequent to larger sized Kimberley towns such as Broome, Derby and Kununurra, smaller communities might have specialists visit only once or twice a year. This makes timely follow-up hard to attain.
It is not uncommon for individuals to move from one town to another further hampering efforts to locate patients for post-operative assessment. Anecdotally, separation from community is a major factor affecting attendance. It takes time, patience, and consistency to engage remote patients and communities. We found that patients from the Derby region and females were more likely to complete follow-up. All of these factors provide a unique challenge to the provision of ear health services, including operative and audiology interventions and follow-up.
There is no consensus on the ideal age for myringoplasty but many authors recommend delaying myringoplasty until the child is older than 8 years in order to allow for eustachian tube maturation which is thought to increase the likelihood of a successful outcome (18). The other school of thought, is that attempting to close the perforation in a child with chronic infections has the potential to improve hearing and quality of life (18). Duval found that preschool children have a significantly higher rate of perforations post tympanoplasty which was attributed to re-perforations after successful healing due to persistence of eustachian tube dysfunction or recurrent acute otitis media (19). Other studies have also found myringoplasty was less successful in paediatric populations (20,21). In our study, 25% of patients were under 8 years of age, and age was not associated with successful myringoplasty. Our study did not demonstrate hearing improvement in the setting of persistent perforation. Perhaps, in some cohorts, delaying myringoplasty till age 8 might improve myringoplasty outcomes. The potential benefit of hearing improvement that may occur despite incomplete closure, has been considered sufficient justification to attempt repair. Hearing improvement facilitates better speech, language and behaviour outcomes in turn avoiding developmental delay. However, some caution should be exercised in generalising the results from overseas studies to our relatively unique cohort.
We found having a normal ABG pre-operatively and a dry middle ear significantly improved the chances of a ‘successful’ myringoplasty. The effect of a discharging ear on the graft take has not been resolved. Some have proposed that dry, uninfected ears provide optimum conditions for healing (22), while others have reported comparable closure in the presence of a wet ear (23). The association between a dry ear at the time of surgery booking and success suggests that perhaps only patients with dry ears should be offered a myringoplasty. This can be problematic because the state of middle ear can frequently fluctuate. In our cohort the percentage of dry ears improved from 83% at the time of booking to 90% at the time of surgery. In addition, it can be problematic to cancel surgery when patients have had to travel far with their families to attend specialist care.
The favoured approach is often dependent on the site of perforation and the surgeons’ preference. The endaural approach is commonly used for posterior or central perforations, while anterior perforations are often best approached postauricular (18). The transcanal approach, a suitable option for small central perforations has been popular, and is frequently technically suitable in Indigenous Australian ears because the external auditory canal is often well sized to allow good exposure. We noted with interest that the different surgical approaches did not appear to influence outcomes.
A variety of graft materials including temporalis fascia, fat, perichondrium, cartilage, composite grafts, and bio design synthetic grafts are used in myringoplasty. There has been insufficient evidence to indicate successful outcomes associated with any particular graft types (18). Temporalis fascia is the most common graft type reported (18). Temporalis fascia has been generally considered more robust than tragal perichondrium, but less than tragal cartilage or composite grafts. We found that temporalis fascia had the highest rate of closure but the difference between temporalis fascia and tragal perichondrium grafts was not statistically significant.
The state of middle ear disease and hearing loss in the Indigenous Australians is complex, and this should be reflected in any approach to its remediation (2). Our data suggest that myringoplasty outcomes in the Kimberley over the last decade are poor. Furthermore, this study suggests that outcomes from myringoplasty have not demonstrably improved compared to the data reported by Mak et al. (7,8). We remain mindful however that our results are based on a minority of recorded procedures due to patients being lost to follow-up and incomplete data recording.
Significant resources are required to access, evaluate, consent, mobilise, operate and follow-up on any surgical case in remote towns and communities. Systems to improve coordination of data as well as post-operative care are needed in addition to clinician led systematic prospective data collection to ascertain the success rate of outreach services and surgeries, including myringoplasty. Standardised audits will allow for appropriate patient selection and adequate resource allocation and help improve myringoplasty outcomes in disadvantaged Indigenous Australians. It is often commented that middle ear disease is a reflection of the underlying health status of the community (24). There are likely limitations to what can realistically be achieved with patient selection and operative technique in this cohort. It is quite probable that more wide-sweeping changes to living conditions, access to clean water, better nutrition, and health care workers will go further to improve ear and hearing outcomes.
Conclusions
The overall closure rate following myringoplasty surgery in Indigenous Australians was 39% in the West Kimberley region over the last decade. TM perforation closure improved hearing. A standardised and integrated approach to documentation will assist in minimising unnecessary data attrition. Improving patient attrition figures will continue to be a challenge and will take coordination and education to realise. Myringoplasty outcomes will likely remain poor in this cohort until community health standards improve.
Acknowledgments
The authors would like to thank Kimberley Aboriginal Medical Services, Kimberley Aboriginal Health Planning Forum, Derby Aboriginal Health Services, Broome regional Aboriginal Health Services, Western Australia Country Health Services, Broome Hospital, Derby Hospital.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.05.05). EHO serves as an unpaid editorial board member of Australian Journal of Otolaryngology. JK serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was provided by WACHS (No. 2015/23), the Western Australian Aboriginal Health Ethics Committee (WAAHEC) (No. 640), Kimberley Aboriginal Health Planning Forum (KAHPF) (No. 2015/-016), and University of Adelaide ethics committee (No. 2015/23). Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Australian Institute of Family Studies. Ear disease in Aboriginal and Torres Strait Islander children. [Canberra, A.C.T.: Closing the Gap Clearinghouse], 2014:21.
- Burns J, Thomson N. Review of ear health and hearing among Indigenous Australians. Perth, WA: Australian Indigenous HealthInfoNet, 2013.
- Vanderpoll TH, Damien Phoenix Consulting Northern Territory. Dept. of Correctional Services. Investigation into hearing impairment among Indigenous prisoners within the Northern Territory Correctional Services / Troy Vanderpoll and Damien Howard. Darwin: Northern Territory Correctional Services, 2011.
- O'Leary SJ, Triolo RD. Surgery for otitis media among Indigenous Australians. Med J Aust 2009;191:S65-8. [PubMed]
- Australian Institute of Health and Welfare. Northern Territory Remote Aboriginal Investment: Ear and Hearing Health Program July 2012 to June 2016 (Cat. no. IHW 176). 2017.
- Morris PS, Leach AJ, Silberberg P, et al. Otitis media in young Aboriginal children from remote communities in Northern and Central Australia: a cross-sectional survey. BMC Pediatr 2005;5:27. [Crossref] [PubMed]
- Mak D, MacKendrick A, Weeks S, et al. Middle-ear disease in remote Aboriginal Australia: a field assessment of surgical outcomes. J Laryngol Otol 2000;114:26-32. [Crossref] [PubMed]
- Mak D, MacKendrick A, Bulsara M, et al. Outcomes of myringoplasty in Australian Aboriginal children and factors associated with success: a prospective case series. Clin Otolaryngol Allied Sci 2004;29:606-11. [Crossref] [PubMed]
- Australian Bureau of Statistics. Regional Statistics - Kimberley, Western Australia outback [document]. 2015 (updated 2015-06-29). Available online: http://stat.abs.gov.au/itt/r.jsp?RegionSummary®ion=50804&dataset=ABS_REGIONAL_ASGS&geoconcept=REGION&datasetASGS=ABS_REGIONAL_ASGS&datasetLGA=ABS_REGIONAL_LGA®ionLGA=REGION®ionASGS=REGION
- Australian Bureau of Statistics. Derby-West Kimberley. 52800 ed: Australian Bureau of Statistics, 2015.
- WA Department of Planning Lands and Heritage. Communities in DAA Districts 2017 Available online: https://www.daa.wa.gov.au/about-the-department/publications/maps/communities-in-daa-districts/
- Franks JR. Hearing measurement. Occupational Exposure to Noise: Evaluation, Prevention and Control. Geneva: World Health Organisation, 2001:183-231.
- Phillips JS, Yung MW, Nunney I. Myringoplasty outcomes in the UK. J Laryngol Otol 2015;129:860-4. [Crossref] [PubMed]
- Berglund M, Florentzson R, Fransson M, et al. Myringoplasty Outcomes From the Swedish National Quality Registry. Laryngoscope 2017;127:2389-95. [Crossref] [PubMed]
- Carr MM, Poje CP, Nagy ML, et al. Success rates in paediatric tympanoplasty. J Otolaryngol 2001;30:199-202. [Crossref] [PubMed]
- Karela M, Berry S, Watkins A, et al. Myringoplasty: surgical outcomes and hearing improvement: is it worth performing to improve hearing? Eur Arch Otorhinolaryngol 2008;265:1039-42. [Crossref] [PubMed]
- Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians, June 2011 [document]. 2013 (updated 2013-08-30). Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3238.0.55.001Main+Features1June%202011?OpenDocument
- Aggarwal R, Saeed SR, Green KJ. Myringoplasty. J Laryngol Otol 2006;120:429-32. [Crossref] [PubMed]
- Duval M, Grimmer JF, Meier J, et al. The effect of age on pediatric tympanoplasty outcomes: a comparison of preschool and older children. Int J Pediatr Otorhinolaryngol 2015;79:336-41. [Crossref] [PubMed]
- Vrabec JT, Deskin RW, Grady JJ. Meta-analysis of pediatric tympanoplasty. Arch Otolaryngol Head Neck Surg 1999;125:530-4. [Crossref] [PubMed]
- Lancaster JL, Makura ZG, Porter G, et al. Paediatric tympanoplasty. J Laryngol Otol 1999;113:628-32. [Crossref] [PubMed]
- Kotecha B, Fowler S, Topham J. Myringoplasty: a prospective audit study. Clin Otolaryngol Allied Sci 1999;24:126-9. [Crossref] [PubMed]
- Caylan R, Titiz A, Falcioni M, et al. Myringoplasty in children: factors influencing surgical outcome. Otolaryngol Head Neck Surg 1998;118:709-13. [PubMed]
- World Health Organisation. Prevention of Hearing Impairment from Chronic Otitis Media. 1996.
Cite this article as: Soumya , Hinton-Bayre A, Coates H, Ooi EH, Kuthubutheen J. Myringoplasty outcomes of Indigenous Australians in the West Kimberley region of Western Australia. Aust J Otolaryngol 2018;1:18.