An 11-year tertiary level audit of surgical pathology of the parotid in Western Australia
Introduction
Neoplasms of the major salivary glands, and particularly the parotid gland, are known to be diverse. The treatment of choice for most salivary gland neoplasms is surgical extirpation, with or without adjuvant therapies (1,2). Classic literature has tended to suggest that benign tumours are more common than malignant tumours, particularly when referring to primary salivary gland tumours of the parotid (1). However, we noticed what seemed to be a large number of parotid operations being performed for malignancy, and in particular metastatic disease. This observation provided the impetus for the present study.
Given the high rates of cutaneous malignancy in Australia (1), we were particularly interested in the rates of cutaneous metastases to the parotid. Many Australians experience long-term exposure to elevated levels of ultraviolet radiation, a known risk factor for developing cutaneous malignancies, especially in sun-exposed head and neck regions (2). While basal cell carcinoma is the most common skin cancer in Australia, it rarely metastasizes. Squamous cell carcinoma (SCC) however, is typically more aggressive and more readily metastasises. A prospective Australian cohort of 87 patients with metastatic SCC to the parotid gland was found to have a very poor prognosis (2).
Parotid neoplasms can present in a number of ways, but most commonly a palpable mass will be the reason for a surgical referral. A detailed history and examination, combined with imaging and in many cases cytology via fine-needle aspirate, will be undertaken in the work-up. For those cases that were suitable for surgery, we wanted to better quantify the types of pathology encountered.
Methods
This study is a retrospective electronic chart review of prospectively recorded data on all patients who underwent surgery to the parotid gland treated within any of the three tertiary level Western Australia public hospitals (Sir Charles Gairdner Hospital, Royal Perth Hospital, and Fremantle Hospital), over an 11-year period [2003–2013]. Cases were obtained through interrogation of a prospectively and independently maintained electronic operating theatre database at each hospital. All cases where a surgical procedure was recorded with the term stem ‘parotid’, including ‘parotidectomy’, were extracted. Using hospital unique identifier numbers, the electronic medical records of these patients were reviewed in a separate database to obtain demographic data (age and gender), date of procedure, and surgical histopathologic diagnosis. Clinical data regarding presentation, medical history, examinations and investigations were not available electronically. A de-identified dataset was securely stored and used for analysis. Ethics approval was granted through the WA Human Research Ethics Committee (HREC 15-088).
Results
A total of 706 operations were performed that involved partial or complete resection of the parotid gland. There were 462 (65%) male and 244 (35%) female patients in total. The mean age was 61.0 (SD =16.8, range, 8–98). The majority of operations were performed on neoplastic lesions (n=686). A small number performed on infective/inflammatory processes (Chronic sialadenitis, n=10; Abscess, n=6; Sialolithiasis, n=4) were excluded from further analysis. Table 1 presents a list of all neoplastic histologic outcomes. Malignant neoplasms (n=364) were more frequent than benign neoplasms (n=322) of the parotid. SCC was the most common surgical pathology, followed by Pleomorphic Adenoma. Combined with Warthin’s tumour and metastatic Melanoma, these four neoplasms accounted for 80% of surgical parotid pathology. Furthermore, the ten most frequent tumours made up 93% of cases, with each accounting for more than 1%. Metastatic cutaneous malignancies (n=293) far outnumbered primary salivary gland neoplasms (n=71). Of note, the top three malignant diseases were of cutaneous origin.
Table 1
| Benign | n (N=322) | % | Malignant | n (N=364) | % |
|---|---|---|---|---|---|
| Pleomorphic adenoma | 195 | 28 | Squamous cell carcinoma | 230 | 34 |
| Warthin’s | 80 | 12 | Melanoma | 38 | 6 |
| Lymphoepithelial cyst | 12 | 2 | Basal cell carcinoma | 19 | 3 |
| Oncocytoma | 11 | 2 | Adenocarcinoma | 13 | 2 |
| Basal cell adenoma | 5 | <1 | Acinic cell carcinoma | 11 | 2 |
| Lipoma | 4 | – | Mucoepidermoid carcinoma | 11 | 2 |
| Myoepthelioma | 3 | – | Lymphoma | 8 | 1 |
| Atypical fibroxanthoma | 2 | – | Merkel cell carcinoma | 6 | <1 |
| Sialocele | 2 | – | Adenoid cystic carcinoma | 4 | – |
| Benign mixed tumour | 1 | – | Epithelial-myoepithelial carcinoma | 4 | – |
| Castleman’s disease | 1 | – | Salivary duct carcinoma | 4 | – |
| Cavernous haemangioma | 1 | – | Microcystic adnexal carcinoma | 3 | – |
| Follicular hyperplasia | 1 | – | Large cell carcinoma | 2 | – |
| Lymphoid hyperplasia | 1 | – | Malignant peripheral nerve sheath tumour | 2 | – |
| Lymphadenoma | 1 | – | Myoepithelial carcinoma | 2 | – |
| Necrotising granuloma | 1 | – | Carcinoma ex-Pleomorphic | 1 | – |
| Paraganglioma | 1 | – | Clear cell carcinoma | 1 | – |
| Neuroendocrine carcinoma | 1 | – | |||
| Oncocytic carcinoma | 1 | – | |||
| Poorly differentiated Carcinoma | 1 | – | |||
| Small cell carcinoma | 1 | – | |||
| Spindle cell carcinoma | 1 | – |
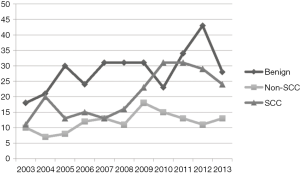
The incidence of surgical pathology over the period of data collection is presented in Figure 1. Given the rates observed in Table 1, malignancies were separated into SCC and non-SCC, and plotted along with benign pathologies. Benign parotid neoplasms overall had a stable incidence over the 11-year review period, with an uncharacteristic peak in 2012. Rates of SCC exceeded other malignancies combined over the period examined, with a clear preponderance from 2010 through to 2013.
Focusing on the neoplastic cases, there were significantly greater number of operations performed on males (n=449) compared to females (n=237), χ2[1]=64.9, P<0.001. Moreover, clear sex differences were seen in distribution of neoplasms. Females were more likely to have a benign (n=164) rather than malignant (n=80) pathology, χ2[1]=28.9, P<0.001. The reverse was seen for males, who were more likely to have a malignant (n=284) rather benign (n=179) neoplastic pathology, χ2[1]=23.8, P<0.001. Overall, males were 3.25 [odds ratio (OR), 95% confidence interval (CI): 2.34–4.51] times more likely than females to have a malignant parotid neoplasm {χ2[1]=52.2, P<0.001}. Of note, there were roughly equal numbers of males (n=165) and females (n=157) with benign parotid neoplasms. In females with malignant parotid neoplasms (n=80), the majority were carcinomas of cutaneous origin (n=52). Half of malignant parotid neoplasms were SCC in females (n=40). On the other hand, in males with malignant neoplasms (n=284), the vast majority were of cutaneous origin (n=241). Notably, two-thirds of malignant parotid neoplasms were SCC (n=190).
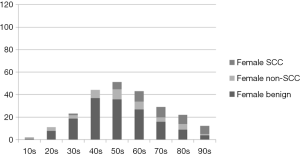
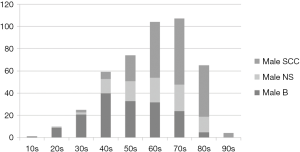
Age as well as sex appears to influence surgical pathology. Figures 2 and 3 depict the age-group stacked histograms for benign, non-SCC malignancy, and SCCs for females and males respectively. Age was plotted as groups in decades. For women, the peak decades for benign neoplasms were the 40, 50, and 60 s (Figure 2). It was not until women were 80 years and above that malignant neoplasms were more frequent than benign neoplasms. SCCs were increasingly more common for females in the 50s decade and above. For men, the peak decades for benign neoplasms were again in the decades 40, 50, and 60 s (Figure 3), with frequencies comparable to females. However, malignant neoplasms were more common for males 50 years and above, peaking in the 70 s decade. It was also observed for men in their 50 s, that SCCs became more frequent than other malignancies combined. This trend continued in older decades, with SCC becoming the most common pathology in males 60 years and above. Further quantifying the association of sex and age with malignancy rates for females, benign neoplasms were more common than malignant neoplasms, irrespective whether age was 50 years and below or above 50 years. Nonetheless, malignancy was 3.23 (95% CI: 1.70–6.13) times more likely when females were aged over 50 years {χ2[1]=13.57, P<0.001}. In contrast, for males, malignancy was 8.45 (95% CI: 5.19–13.77) times more likely when over 50 years old {χ2[1]= 86.26, P<0.001}.
Discussion
As far as we are aware, this study presents the largest series of surgical parotid pathology in the Australian medical literature. Through retrospectively examining surgical operating and pathology databases we were able to examine over 700 cases of parotid surgery performed over an 11-year period. The population distribution and tertiary referral systems of Western Australia are relatively unique. The state of Western Australia has a vast land area of 2.6 million km2 and is home to a population of around 2.6 million people. Despite this wide area and referral base, patients referred to the public health system for assessment and surgery (from both rural and urban settings) received their treatment in one of the three public Head and Neck surgery services, all of which are in the greater Perth metropolitan area. The close proximity of referral services facilitated the broader scale collection of data.
As many as 80% of all salivary gland neoplasms occur within the parotid gland (1), with surgical extirpation the treatment of preference in most instances. Our data indicated that 96% of patients underwent surgery for a neoplastic lesion. Many contemporary texts and epidemiology reports suggest benign neoplasms are the most common (75–80%) (1,3-6). Our results are comparable if only primary salivary gland neoplasms are considered, where 84% were benign. In contrast, when all surgical pathology to the parotid was considered the present series found that malignant neoplasms overall were more common (53%). In particular metastatic SCC predominated, accounting for 34% of all parotid neoplasms, and 63% of parotid malignancies.
The likelihood of an individual undergoing parotid surgery for a malignancy was moderated by both sex and age. More males underwent parotid surgery than females irrespective of pathology. Yet, male and female rates for benign disease were almost equivalent. The sex difference was more apparent for malignancies, with males almost 3.5 times more likely to have surgery for cancer than females. When age was also considered it was apparent that the likelihood of malignancy rose when patients were over 50 years old. Pathology was more likely to be benign in both males and females under 50 years undergoing parotid surgery. However, females over 50 years were over three times more likely to have surgery for malignancy, with an over eight times risk seen in males over 50 years old. Again, the prevalence of SCC as the surgical pathology predominated with advancing age. SCC was clearly the most common pathology seen in males over 60 years old. These data suggest that SCC should be a top differential for a Western Australian presenting with a parotid mass, particularly if the individual is over 50 years old, and especially if they are male. Moreover, as metastatic cutaneous malignancies accounted for 43% of all parotid surgical pathology, a thorough history and examination of prior or active skin cancers is mandated in the setting of a parotid mass. Skin type and sun exposure are known independent risk factors for cutaneous malignancies (2), and warrant consideration in risk assessment for parotid masses in the Australian setting
There is a divide in the literature regarding the most common malignant lesion of the parotid gland. While some studies have found metastatic lesions such as SCC be the most commonly isolated malignant lesion (3), others have found primary malignant lesions to be more common (5,6). We found that cutaneous based malignancies of parotid were very common in males aged 50 and above. In particular, SCC was most common malignant parotid lesion (32.53%) in our patient cohort. This was significantly higher than the previously reported from other Australian studies. Coombe et al. reported a prevalence of 21.53% (7), while O’Brien et al. reported a prevalence of 9.17% (4). The high incidence of metastatic SCC to the parotid gland is felt to be an Australian phenomenon and confers patients an extremely poor prognosis especially if locoregional control is not achieved early in a patient’s course of management (8).
The most commonly isolated benign tumours of the parotid gland are pleomorphic adenomas and Warthin’s tumours (9). This was also reflected in our series where these were the two most common benign tumours isolated—pleomorphic adenoma (61.90%), followed by Warthin’s tumour (25.40%). This result was also consistent with that of a recent Australian study by Coombe et al. (7) where pleomorphic adenoma (56.10%) followed by Warthin’s tumour (23.17%) were similarly also the most commonly isolated benign primary salivary gland neoplasms.
Given the high prevalence of malignancy within parotid masses in our patient cohort, it is essential to have a high index of suspicion for patients presenting with parotid gland masses. A careful history with a comprehensive physical examination including the scalp and face is essential, and can help identify potential malignant or metastatic disease. Other investigations such as radiological imaging and fine needle aspirates (FNA) serve as useful adjuncts in determining the aetiology and nature of the parotid lesion. Cytological evaluation through FNA can assist clinicians in not only differentiating between neoplastic and non-neoplastic lesions but also in determining if a neoplastic lesion is benign or malignant (10). However, the overall role of cytological evaluation of parotid specimens obtained via FNA remains debatable. This is due to a relatively high false-negative rate (40%) (11), variable sensitivity for diagnosing neoplasia (96%) and malignancy (79%) (10), and significant variability of both the sensitivity and specificity of this test in diagnosing parotid lesions (10).
The Australian Cancer Registry (ACR) recorded 258 parotid cancers in 2013 nationwide. This represents only 0.2% of cancers diagnosed in that year according to the Australian Institute of Health and Welfare (AIHW). The ACR uses multiple strategies to identify cancers, yet formal histology was used in around 85% of cases (WA Cancer Registry 2012). Moreover, parotid malignancy rates represent those of primary salivary gland neoplasms (ICD C07). Metastatic deposits will be recorded under the original pathology, including SCC, BCC, and melanoma. Benign tumour rates were not reported. Thus, such data does not readily translate to the clinical presentation of a parotid mass and likelihood of subsequent surgical pathology. For this reason, we feel our data provides important translational information for Australian head and neck surgeons and primary care physicians. A recent study on projected malignancy rates, suggested primary parotid malignancies should decline over the decade [2014–2025] (12). However, it is the rates metastatic malignancies of cutaneous origin, in particular SCC, that are seemingly of greater importance.
The incidence of cutaneous malignancies is rising worldwide along with its consequential strain on health care services (2). Incidence does however vary geographically due to factors such as UV radiation exposure and skin type (2). Australians live in a climate where they are exposed to large amounts of UV radiation and are at an increased risk of developing cutaneous malignancies such as SCC (2). This study further highlights the importance public health initiatives such as educating patients on the importance of maintaining adequate sun protection precautions throughout the year as a means of primary prevention.
It is important to be mindful of the limitations of this study. Most importantly, it is not a study of true prevalence. First, pathology was determined from post-operative specimens. Rates are potentially biased, by including only those who are medically fit and elected to undergo surgical management of their disease. Second, the decision to proceed with parotid surgery will potentially be swayed by the suspicion or confirmation of malignancy on pre-operative fine needle aspirate or core biopsy. It is possible older individuals with benign pathology on FNA, or surgically unfit individuals have been missed by the collection of post-surgical data. This could potentially exaggerate the comparative rates of malignancy seen in the older age-groups. Third, only tertiary public hospital surgical databases were interrogated. Our data collection did not capture information on patients who underwent parotid surgery in private institutions and other non-tertiary settings. It is therefore uncertain whether there is a bias to having malignant neoplasms resected within the public system. To gain a more accurate perception of incidence, prospective data from assessments in both public and private clinics would need to be undertaken. Our impression is that such biases are likely small, and unlikely to demonstrably alter the relative frequencies of pathologies found. The study design also adds an element of selection bias in that all patients in our cohort elected to undergo surgery to their parotid. For example, patients with benign parotid disease who elected to have their disease conservatively managed or patients who were high-risk surgical candidates due to their poor general health, or even patients with malignant parotid disease but had disseminated metastases, were missed from our study. However, given our large study population number, we suspect that these cases were few and are therefore unlikely to impact our overall outcomes significantly.
In contrast to literature from other countries where benign lesions accounted for up to 80% of all parotid lesions (1), SCC was the most common parotid pathology in our Australian cohort—accounting for almost a third of our patients, even more common than pleomorphic adenoma.
This study provides one of the larger cohorts of patients published over this timeframe, through which it was possible to perform a state-wide tertiary level review on pathologic outcome from parotid surgery. It is also the first Western Australian tertiary level study that provides epidemiological data on parotid surgery pathology in Western Australia. It highlights the significant statewide prevalence of metastatic SCC to the parotid, especially given the poor prognosis this disease is known to confer on patients (8). It serves as a basis for, and highlights the importance of, further research to be conducted into management and outcomes of parotid neoplasms, particularly cutaneous malignancies Australia.
Acknowledgments
We would like to acknowledge the various departments (especially the Department of Pathology) within the three WA Health tertiary hospitals, without whom this publication would not be possible.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.09.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was granted through the WA Human Research Ethics Committee (HREC 15-088). Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Speight PM, Barrett AW. Salivary gland tumours. Oral Dis 2002;8:229-40. [Crossref] [PubMed]
- Lomas A, Leonardi Bee J, Bath Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol 2012;166:1069-80. [Crossref] [PubMed]
- Upton D, McNamar J, Connor N, et al. Parotidectomy: ten-year review of 237 cases at a single institution. Otolaryngol Head Neck Surg 2007;136:788-92. [Crossref] [PubMed]
- O'Brien CJ, Malka VB, Mijailovic M. Evaluation of 242 consecutive parotidectomies performed for benign and malignant disease. Aust N Z J Surg 1993;63:870-7. [Crossref] [PubMed]
- Lin CC, Tsai MH, Huang CC, et al. Parotid tumors: a 10-year experience. Am J Otolaryngol 2008;29:94-100. [Crossref] [PubMed]
- Takahama Junior A, de Almeida O, Kowalski L. Parotid neoplasms: analysis of 600 patients attended at a single institution. Braz J Otorhinolaryngol 2009;75:497-501. [Crossref] [PubMed]
- Coombe RF, Lam AK, O'Neill J. Histopathological evaluation of parotid gland neoplasms in Queensland, Australia. J Laryngol Otol 2016;130:S26-31. [Crossref] [PubMed]
- O'Brien CJ, McNeil EB, McMahon JD, et al. Significance of clinical stage, extent of surgery, and pathologic findings in metastatic cutaneous squamous carcinoma of the parotid gland. Head Neck 2002;24:417-22. [Crossref] [PubMed]
- Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg 1986;8:177-84. [Crossref] [PubMed]
- Schmidt RL, Hall BJ, Wilson AR, et al. A systematic review and meta-analysis of the diagnostic accuracy of fine-needle aspiration cytology for parotid gland lesions. Am J Clin Pathol 2011;136:45-59. [Crossref] [PubMed]
- Sergi B, Contucci A, Corina L, et al. Value of fine-needle aspiration cytology of parotid gland masses. Laryngoscope 2004;114:789. [Crossref] [PubMed]
- Abdelhafied D, Kruger E, Tenant M. Projections of the incidence of pharyngeal, tongue and parotid gland cancer in Western Australia. Austral-Asian J Cancer 2014;13:31-6.
Cite this article as: Davidoss NH, Wormald R, Hinton-Bayre A. An 11-year tertiary level audit of surgical pathology of the parotid in Western Australia. Aust J Otolaryngol 2018;1:19.