
Management of post tonsillectomy secondary haemorrhage: Flinders experience
Introduction
Secondary post-tonsillectomy haemorrhage (sPTH) is a common post-operative complication in Otolaryngology with the National prospective tonsillectomy audit reporting a secondary haemorrhage rate ranging from 1.3% to 6.1% in 33921 patients undergoing tonsillectomy between 2003 and 2004 in England and Northern Ireland (1). The majority of available literature focuses on the factors associated with the risk of sPTH such as surgical technique, same day discharge or surgeon experience with only limited evidence-based literature on the management of sPTH (2) once a patient presents with sPTH. Conservative management of sPTH is usually attempted in the first instance. However, it is unclear how safe or effective conservative management is or whether it is associated with increased length of stay (LOS). A 7-year retrospective analysis by Arora et al attempted to produce guidelines for management of sPTH (3). Their protocol was to admit most patients with sPTH, with 61% of their patients requiring active medical intervention. Also, patients under 6 years of age with a normal oropharyngeal examination at the emergency department were less likely to need further intervention (3).
Flinders Medical Centre (FMC) is a tertiary academic South Australian (SA) public hospital that covers a large geographical area in the southern region of SA. There are several peripheral public and private hospitals in this geographical area performing tonsillectomy in both adults and paediatric patients. FMC provides 24-hour emergency Otolaryngology care service for patients living in this area. Hence, patients with sPTH presenting to FMC for admission and management in the study include patients operated at FMC as well as other surrounding hospitals.
The Stammberger classification for sPTH proposed a method of grading bleeding episodes according to the clinical examination findings of the oropharynx and the need to intervene (Table 1) following a 9-month prospective analysis of sPTH at a single centre (4). In April 2014, Flinders Medical Centre (FMC) applied the Stammberger classification of sPTH for all patients presenting to FMC as part of a protocol (Figure 1) and results were audited every four weeks.
Table 1
| Stammberger grade | Returned to theatre | Adult | Paediatric |
|---|---|---|---|
| A1—dry wound, no coagulum | No | 25 (89%) | 18 (95%) |
| Yes | 3 (11%) | 1 (5%) | |
| Median length of stay, hours [IQR] | 18 [10–30] | 17 [14–22] | |
| A2—coagulum, dry wound after removal of coagulum | No | 33 (97%) | 20 (95%) |
| Yes | 1 (3%) | 1 (5%) | |
| Median length of stay, hours [IQR] | 25 [18–30] | 26 [17–36] | |
| B1—active bleeding, non-invasive treatment | No | 10 (100%) | 6 (100%) |
| Yes | 0 (0%) | 0 (0%) | |
| Median length of stay, hours [IQR] | 29 [24–34] | 31 [18–47] | |
| B2—active bleeding, treatment under local anaesthesia | No | 0 (0%) | 3 (75%) |
| Yes | 0 (0%) | 1 (25%) | |
| Median length of stay, hours [IQR] | – | 35 [18–44] | |
| C—haemorrhage needing treatment under general anaesthesia | No | 0 (0%) | 0 (0%) |
| Yes | 14 (100%) | 9 (100%) | |
| Median length of stay, hours [IQR] | 31 [28–36] | 36 [34–40] |
IQR, interquartile range.
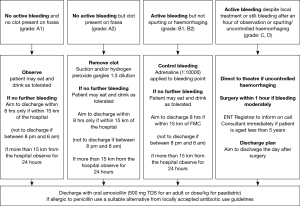
This study aims to report outcomes of patients presenting with sPTH to FMC, graded according to the Stammberger classification, with regards to re-bleeding during their admission (Figure 2).
Methods
The Otolaryngology department at FMC has an electronic registry that identifies all patients with sPTH admitted to the hospital. A retrospective chart review of all sPTH admissions to FMC from April 2014 to May 2016 identified by the registry was conducted to analyse the management of sPTH. For the purposes of this study, sPTH was defined as a bleeding episode beyond midnight of the day of the tonsillectomy. Each admission to FMC was counted and analysed as a single episode of sPTH for the purposes of this study. A proportion of these patients had their tonsillectomy at a hospital other than FMC.
Statistical analysis
Non-parametric two tailed Mann-Whitney-U and Fisher’s Exact Chi-Squared testing was conducted for categorical comparisons and Kruskal-Wallis test for multivariate analysis. An alpha value of 0.05 was utilized to determine statistical significance. Central tendency reported as median values with interquartile range (IQR) due to small sample size and non-normal distribution of data.
Ethics approval
Ethical approval was granted by The Southern Adelaide Clinical Human Research Ethics Committee. There was no conflict of interest declared by the authors of this paper.
Results
In 24 months, 145 patients presented to FMC with sPTH. Fifty-nine percent of these patients were adults with a median age of 24 years (IQR, 21–34 years). Forty-one percent of patients were under 18 years of age with a median age of 10 years (IQR, 4–15 years). Overall, there were slightly more male adult (59%) presentations whereas there were slightly more female paediatric presentations (56%).
The majority (80%) of the patients treated at FMC for sPTH had their initial surgery elsewhere (Table 2). Indication for surgery was not documented in the case notes for 50% of the patients who didn’t have their original tonsillectomy at FMC; therefore, we were unable to analyse the indication for tonsillectomy. We attempted to contact the private ENT surgeon of the patient but were unable to obtain the required private medical records for all the patients. Recurrent tonsillitis was the most common indication for tonsillectomy where adequate documentation in the case notes was present. Overall, 58% of the patients had coblation (COB) tonsillectomy and the remaining patients had cold steel (CS) tonsillectomy with bipolar haemostasis. Majority of the paediatric patients had CS tonsillectomy (56%) whereas the majority of adult patients had COB tonsillectomy (67%).
Table 2
| Adult | Paediatric | Overall | |
|---|---|---|---|
| Number of patients [%] | 86 [59] | 59 [41] | 145 |
| Median age [IQR] | 24 [21–34] | 10 [4–15] | 19 [12–26] |
| Gender, n [%] | |||
| Female | 35 [41] | 33 [56] | 68 [47] |
| Male | 51 [59] | 26 [44] | 77 [53] |
| Median length of stay, hours [IQR] | 25 [16–32] | 22 [16–36] | 25 [16–34] |
| Return to theatre (RTT), n [%] | |||
| Yes | 18 [21] | 12 [20] | 30 [21] |
| No | 68 [79] | 47 [80] | 115 [79] |
| Location of primary surgery, n [%] | |||
| Flinders Medical Centre (FMC) | 16 [18] | 13 [22] | 29 [20] |
| Flinders Private Hospital (FPH) | 40 [47] | 19 [32] | 59 [41] |
| Other hospitals | 30 [35] | 27 [46] | 57 [39] |
| Indication, n [%] | |||
| RT | 30 [35] | 11 [19] | 41 [28] |
| SDB/OSA | 8 [9] | 16 [27] | 24 [17] |
| RT & SDB/OSA | 2 [2] | 5 [8] | 7 [5] |
| Not recorded | 46 [54] | 27 [46] | 73 [50] |
| Tonsillectomy technique, n [%] | |||
| Cold steel with bipolar (CS) | 28 [33] | 33 [56] | 61 [42] |
| Coblation (COB) | 58 [67] | 26 [44] | 84 [58] |
IQR, inter quartile range; RT, recurrent tonsillitis; SDB, sleep disordered breathing; OSA, obstructive sleep apnoea.
Overall, 79% of the patients were treated conservatively without the need to return the patient to theatre (RTT). Twelve children (20% of the paediatric group) returned to theatre and 18 adults (21% of the adult group) returned to theatre. Adult patients were marginally more likely to RTT compared to paediatric patients with RR =1.07 (CI 0.5–2.3), however, patient age was not a statistically significant factor for returning to theatre (P>0.05). The overall relative risk (RR) of returning to theatre is higher if the patient had a COB tonsillectomy [RR =1.45 (CI 0.7–2.9)]. This was observed for both paediatric patients with a RR =1.78 (CI 0.6–5.0) and for adult patients with a RR =1.25 (CI 0.5–3.1). However, these RR values were not statistically significant (P>0.05) between CS and COB groups.
sPTH presentations were graded according to Stammberger classification (Table 1). There were no grade D or E presentations. The majority of presentations were classified as grade A2 (38%). The majority of paediatric patients who had a CS tonsillectomy presented with a grade A1 (42%) sPTH, whereas most paediatric patients who had COB tonsillectomy presented with a grade A2 (42%) sPTH. In adult patients both CS and COB tonsillectomy groups presented with 39% and 40% grade A2 sPTH respectively (Table 3).
Table 3
| Stammberger classification | Adult [%] | Paediatric [%] | Total | |||
|---|---|---|---|---|---|---|
| Cold steel with bipolar haemostasis | Coblation | Cold steel with bipolar haemostasis | Coblation | |||
| A1 | 7 [25] | 21 [36] | 14 [42] | 5 [19] | 47 [32] | |
| A2 | 11 [39] | 23 [40] | 10 [29] | 11 [42] | 55 [38] | |
| B1 | 5 [18] | 5 [9] | 2 [6] | 4 [16] | 16 [11] | |
| B2 | 0 [0] | 0 [0] | 3 [9] | 1 [4] | 4 [3] | |
| C | 5 [18] | 9 [15] | 4 [12] | 5 [19] | 23 [16] | |
| Total | 28 | 58 | 33 | 26 | 145 | |
In total, thirteen patients (8.9% of the original sPTH) from grade A1 to B2 were readmitted for subsequent sPTH (i.e., more than one admission with sPTH) with seven of these patients needing RTT (Table 4). Patients who had COB tonsillectomy were more likely to represent with sPTH and needed to RTT (Table 4). Median time to represent with a sPTH after their tonsillectomy was 42.34 hours (IQR, 14.7–74.4). None of the patients with sPTH who returned to theatre in the initial visit (Stammberger Classification C) subsequently represented to hospital with further haemorrhage.
Table 4
| Patient | Age (years) | Gender | Grade | Time to readmission (hours) | RTT | Technique |
|---|---|---|---|---|---|---|
| 1 | 5 | F | A2 | 3.9 | Yes | COB |
| 2 | 12 | M | A1 | 11.38 | Yes | COB |
| 3 | 15 | F | B2 | 45.93 | Yes | CS |
| 4 | 18 | F | A1 | 38.75 | Yes | COB |
| 5 | 22 | M | A2 | 13.97 | Yes | COB |
| 6 | 22 | F | A1 | 107.42 | Yes | COB |
| 7 | 27 | M | A1 | 88.5 | Yes | COB |
| 8 | 6 | F | A1 | 18.13 | No | CS |
| 9 | 9 | M | A2 | 152.17 | No | COB |
| 10 | 16 | F | B1 | 71.83 | No | COB |
| 11 | 17 | F | A2 | 82.13 | No | CS |
| 12 | 19 | F | A1 | 14.90 | No | COB |
| 13 | 19 | F | A2 | 14.35 | No | CS |
| 14 | 21 | M | A1 | 28.68 | No | COB |
| 15 | 21 | M | A1 | 61.47 | No | COB |
| 16 | 22 | M | A1 | 56.35 | No | CS |
| 17 | 25 | M | B1 | 15.48 | No | COB |
| 18 | 26 | M | A2 | 117.87 | No | COB |
| 19 | 28 | F | A2 | 6.62 | No | CS |
| 20 | 36 | M | A1 | 67.72 | No | COB |
CS, cold steel; COB, coblation; RTT, return to theatre; M, male; F, female.
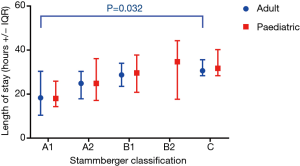
Overall, median LOS was 25 hours per admission with adult patients being admitted for 3 hours longer than the paediatric patients (P>0.05) (Table 2). LOS increased with severity of sPTH (Figure 2), however, the only statistically significant difference was between grade A1 and C for adult patients (13 hours longer in grade C, P=0.032). The median time of admission was 10:00 hours (IQR, 05:17–17:24) in the morning for adults and 15:00 hours (IQR, 05:19–20:47) in the afternoon for paediatric patients.
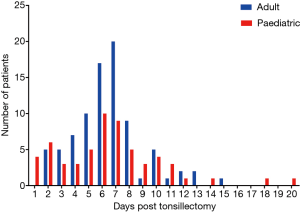
Day 6 post tonsillectomy was the most common day for sPTH presentation for both adults and children (Figure 3). There was no statistically significant difference between the day post tonsillectomy and the grade of sPTH.
Duration between 1st episode of sPTH and 2nd sPTH
Paediatric patients presented with a second bleeding episode at a median duration of 46 hours (IQR, 14.8–76.6) after discharge from hospital (with their first sPTH) compared to adults who presented at a median duration of 39 hours (IQR, 14.9–67.8 hours) after initial discharge. There was no statistically significant difference in time to represent with a second sPTH when compared to age, gender, post-operative day or tonsillectomy technique.
Discussion
Tonsillectomy is a common procedure in otolaryngology with post tonsillectomy haemorrhage being one of the complications that is potentially life threatening (mortality rate 0.002%) (5). A thorough literature search using PubMed®, EMBASE® and Google® advanced search for grey literature indicated no published guidelines for management of sPTH. Standardised recording of events has the benefit of auditing the management of sPTH and for future research. The Stammberger classification (4) (Table 1) provides a way of grading sPTH on admission. Our observations in this study suggest that conservative management in the first instance is appropriate for patients presenting with their first sPTH episode as 79% of patients in our study did not require a return to theatre (RTT) during the first admission for sPTH. We found in our retrospective review that COB tonsillectomy or multiple presentations with sPTH in the same patient was associated with an increased chance of requiring a RTT.
Patients who required a RTT with their first sPTH did not present to FMC or other SA public hospitals with further bleeding episodes. SA health has an electronic patient registry that allows us to identify if patients were admitted at other public hospitals for sPTH. Most of the patients who RTT had a COB tonsillectomy but this result was not statistically significantly compared to the CS group due to the small number of patients in this study. Study of 2,541 tonsillectomies with a COB tonsillectomy technique, reported a 1.7% RTT rate for sPTH (6). They also reported an increased severity of bleeding in this group of patients with 33% of these patients requiring a blood transfusion. The decision to RTT is made at the time of patient presentation based on ongoing oropharyngeal bleeding, and significant decrease in haemoglobin levels. The experience at FMC supports the conservative management of most patients with their first sPTH who had COB tonsillectomy.
Managing patients with a self-reported sPTH with a normal oropharyngeal examination is a contentious issue in the literature, especially in the paediatric setting. The Graz study in 2013 recommends admitting all patients for at least 24 hours for monitoring because of the small risk of a severe second bleeding episode (7). Attner et al. in 2009 reported, only 1 out of 114 paediatric patients with self-reported sPTH, who had a normal oropharyngeal examination on presentation to the emergency department (ED), required further intervention. However, the authors recommend admission and monitoring for potential re-bleeding for all patients (8). A recent study of 407 sPTH presentation (92% paediatric), indicated that only 11% of patients with a normal oropharynx in the initial examination progressed to have a more severe bleeding episode requiring further intervention (9). At FMC (Table 4), only 2 out of 58 paediatric patients (3.4%) with self-reported sPTH (grade A1) required multiple admissions for sPTH and one of these patients needed to RTT for definitive management of sPTH in the subsequent visit. Our results also show that teenaged and adult patients were more likely to require a RTT if they presented on multiple occasions with sPTH. Yuen et al. reports 83% of these re-bleeding episodes occurred within 24 hours of the initial episode, consistent with previously reported data (10). In contrast, our results show 40% of re-bleeding episodes occurred within 24 hours of the initial admission. However, our results also show that re-bleeding in all grade A1 paediatric patients occurred within 24 hours of the initial admission. In contrast, only 13% of adults with an initial grade A1 re-bled within 24 hours of the initial admission. Hence, we propose that paediatric patients with sPTH should be admitted for 24 hours for observation and adult patients require shorter period of inpatient observation. There is no specific literature exploring the safety of specific distances from hospital for the outpatient management of sPTH. However, a recent study from Auckland, New Zealand reporting on the safety of day case tonsillectomy indicated their criteria to be: patients living within one hour from the hospital (11).
Majority of sPTH presentations to FMC were patients who had their tonsillectomy at other institutions in the surrounding geographical area (Table 2) with only 20% of the sPTH presentations having their original surgery at FMC. Indications for the tonsillectomy were poorly recorded in the patient notes. Attempt to contact external surgeons for further history was not always successful. Of the recorded indications, recurrent tonsillitis was the most common indication.
We have considered the distances patients travel to our hospital on presentation with sPTH and the age differences between patients. The overall time to readmit with a second sPTH episode ranged from 15 to 152 hours after their first sPTH with no statistically significant difference when compared to age, gender or tonsillectomy technique. At FMC the median LOS was 25 and 22 hours for adult and paediatric group respectively. The time of presentation appears to be a significant predictor of LOS due to logistical reasons. Median time at presentation was 12:19PM, which meant most patients were kept overnight for observation. Post tonsillectomy haemorrhage is a concern for patients, their families and surgeons. Our retrospective chart review contains only observational data but it does provide some evidence that the risk of requiring a RTT is low and conservative management of grade A and B bleeds is appropriate.
Our results also indicated that patients who re-presented, after their first sPTH, with further bleeding were more likely to require a RTT. Hence, we feel that conservative management for multiple sPTH is less likely to be successful and the patient is more likely to require a RTT for management of their sPTH in those situations.
Our study limitations include the risks and biases inherent to retrospective chart reviews, incomplete data on the indications for tonsillectomy, relatively small sample size, and the heterogeneous population with tonsillectomies performed by multiple surgeons using multiple techniques from various institutions. We also acknowledge the variability in clinical assessment of sPTH in ED setting is based on experience of the medical officer and is likely to affect our dataset.
Conclusions
This retrospective chart review suggests that risk of ongoing bleeding after initial presentation is low for grade A and B sPTH patients and conservative management of sPTH is safe. Patients with multiple sPTH presentations are more likely to require a RTT on subsequent presentations with sPTH. There is no clear evidence on the best management of sPTH based on age, gender or tonsillectomy technique. A prospective controlled study would provide better evidence for the management strategies of sPTH.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.11.02). EHO serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was granted by The Southern Adelaide Clinical Human Research Ethics Committee. Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope 2007;117:717-24. [Crossref] [PubMed]
- Kwok MM, Subramaniyan M, Rimmer J, et al. Post-tonsillectomy haemorrhage in Australia—a multivariable analysis of risk factors. Aust J Otolaryngol 2018;1:2. [Crossref]
- Arora R, Saraiya S, Niu X, et al. Post tonsillectomy hemorrhage: who needs intervention? Int J Pediatr Otorhinolaryngol 2015;79:165-9. [Crossref] [PubMed]
- Sarny S, Ossimitz G, Habermann W, et al. Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 2011;121:2553-60. [Crossref] [PubMed]
- Østvoll E, Sunnergren O, Ericsson E, et al. Mortality after tonsil surgery, a population study, covering eight years and 82,527 operations in Sweden. Eur Arch Otorhinolaryngol 2015;272:737-43. [Crossref] [PubMed]
- Amir I, Belloso A, Broomfield SJ, et al. Return to theatre in secondary post-tonsillectomy haemorrhage: a comparison of coblation and dissection techniques. Eur Arch Otorhinolaryngol 2012;269:667-71. [Crossref] [PubMed]
- Sarny S, Habermann W, Ossimitz G, et al. What lessons can be learned from the Austrian events? ORL J Otorhinolaryngol Relat Spec 2013;75:175-81. [Crossref] [PubMed]
- Attner P, Haraldsson PO, Hemlin C, et al. A 4-year consecutive study of post-tonsillectomy haemorrhage. ORL J Otorhinolaryngol Relat Spec 2009;71:273-8. [Crossref] [PubMed]
- Sarny S, Habermann W, Ossimitz G, et al. Tonsilar haemorrhage and re-admission: a questionnaire based study. Eur Arch Otorhinolaryngol 2011;268:1803-7. [Crossref] [PubMed]
- Yuen S, Kawai K, Roberson DW, et al. Do post-tonsillectomy patients who report bleeding require observation if no bleeding is present on exam? Int J Pediatr Otorhinolaryngol 2017;95:75-9. [Crossref] [PubMed]
- Mahadevan M, van der Meer G, Gruber M, et al. The starship children's hospital tonsillectomy: A further 10 years of experience. Laryngoscope 2016;126:E416-E420. [Crossref] [PubMed]
Cite this article as: Dharmawardana N, Chandran D, Elias A, Kao SST, Ooi EH. Management of post tonsillectomy secondary haemorrhage: Flinders experience. Aust J Otolaryngol 2018;1:31.


