Antibiotic prescribing practices in otolaryngology head and neck surgery in Australia and New Zealand: a survey of 137 specialists
Introduction
Antibiotic resistance has become a global health issue with substantial health and economic burdens (1). Mortality related to antibiotic resistance exceeds 20,000 deaths per year in United States and European Union (1). Although the mortality rate in Australia has not been quantified, there is evidence to suggest that multi-drug resistant Staphylococcus aureus bacteraemia rates are significantly higher than European countries (2). In Australia, 21.9% of hospital antibiotic prescriptions were considered inappropriate either because they were not indicated (19.6%), duration was incorrect (17.7%), dose was incorrect (19.5%) or the chosen antimicrobial did not comply with guidelines (25.2%) (3). To counteract the developing problem of resistance, a national antibiotic resistance strategy has been developed with goals and objectives to mitigate the progression of antimicrobial resistance (1). This is based on the Global Action Plan on Antimicrobial resistance developed by the World Health Organisation (4).
Surgical prophylaxis is the main indication for prescribing antibiotics and interestingly over 40% of antibiotics prescribed are inappropriate. This has remained consistent for the past 3 years (3) and poses a significant problem especially given that close to 750,000 people had elective surgery in public hospitals across Australia in 2016–2017 (5). Specifically within Otolaryngology, Head and Neck Surgery, over 60,000 patients were admitted in public hospitals to receive an elective operation (5). The most common elective operations were tonsillectomy (with or without adenoidectomy), myringotomy and septoplasty (5).
There is currently limited evidence for the role of antibiotics in reducing post tonsillectomy morbidity (6). There is also little evidence to demonstrate the effectiveness of systemic antibiotics in septoplasty and myringotomy ± insertion of middle ear ventilation tubes (7). Australian guidelines recommend that in the absence of specific cardiac conditions, prophylaxis is not required for tonsillectomy, adenoidectomy, endoscopic sinus surgery or uncontaminated neck dissection (8). For other procedures in Otolaryngology, Head and Neck surgery, a single dose of a first generation cephalosporin (cephazolin) and a nitroimidazole (metronidazole) within 60 minutes before surgical incision is recommended for procedures where the incision is made through mucosal surfaces (oral, nasal, pharyngeal and oesophageal) or those involving insertion of a prosthetic material (8).
Evidence to measure the awareness and effectiveness of guidelines, particularly within Australia and New Zealand is sparse. Previous studies in Netherlands suggest that while approximately 70% of Otolaryngologists, Head and Neck Surgeons were aware of national and international, guidelines, adherence rates were only 45% (9). Although studies in the USA demonstrated a higher adherence rate to guidelines in paediatric tonsillectomy patients, there was still a significant non-adherence rate emphasising the need for increased awareness and implementation in the future (10).
This study aims to assess the antibiotic prescribing practices in Otolaryngology, Head and Neck surgery in Australia and New Zealand, comparing current practices to national guidelines and current evidence.
Methods
The names of practising Otolaryngologists registered under Australian Society of Otolaryngology, Head & Neck Surgery (ASOHNS) and New Zealand Society of Otolaryngology, Head & Neck Surgery (NZOHNS) were obtained and an invitation was sent via email to participate in the survey (Supplementary file).
The survey was designed using SurveyMonkey (SurveyMonkey Inc. San Mateo, California, USA). A list of common procedures were obtained from the Royal Australasian College of Surgeons Morbidity Audit and Logbook Tool—Procedure list for Otolaryngology Head and Neck Surgery (11).
The survey contained four pages with the first page asking surgeons about antibiotic prescribing practices for tonsillectomy ± adenoidectomy, septoplasty ± turbinoplasty (with or without packing), functional endoscopic sinus surgery (with or without packing) and insertion of grommets. Options to select were no antibiotics, pre- or post-operative antibiotics. For insertion of grommets, participants were asked to select whether they prescribed oral antibiotics, ototopical or both.
Participants were then asked to indicate their preference of pre- or post-operative antibiotics.
The second page expanded on the list to include different procedures from different subspecialties within Otolaryngology Head and Neck Surgery. This list was adapted from the Royal Australasian College of Surgeons Morbidity Audit and Logbook Tool—Procedure list for Otolaryngology Head and Neck Surgery.
The final section of the survey asked about country of practice (Australia, New Zealand), area of interest and number of years in practice (<5, 5–10, 10–20, >20). Three reminders were sent out at 4-week intervals through email in order to increase response rate.
Results
A total of 472 emails were sent to members from ASOHNS and NZSOHNS. This consisted of 306 ASOHNS members and 166 NZSOHNS members.
After 12 weeks of the survey being active, a total of 137 responses were collected (29.0% response rate). Average survey completion time was 4 minutes and 47 seconds.
Majority of surgeons (64.2%) indicated they practiced general ENT followed by Rhinology (49.2%), Paediatrics (45.8%) and Head and Neck (34.2%). Most surgeons indicated they had been in practice for over 20 years (38.3%), followed by 10–20 years (25%), 5–10 years (20%) and <5 years (16.7%).
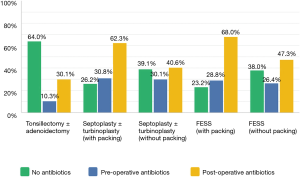
The prescribing practices for tonsillectomy ± adenoidectomy, septoplasty ± turbinoplasty (with and without packing) and FESS (with and without packing) are summarised in Figure 1.
For tonsillectomy ± adenoidectomy, most surgeons (64%, n=87) prescribed no antibiotics while 30.1% (n=41) prescribed postoperative antibiotics (Figure 1). The most common antibiotic prescribed was cephazolin (54.2%, n=13) followed by ampicillin (25%, n=6).
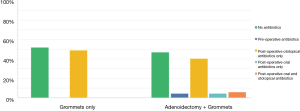
For insertion of middle ear ventilation tubes, most surgeons (51.8%, n=71) did not prescribe antibiotics while 48.9% (n=67) prescribed post-operative ototopical antibiotics only (Figure 2).
For septoplasty ± turbinoplasty most surgeons preferred post-operative antibiotics if they used packing after the operation (62.3%, n=81) as opposed to no packing (40.6%, n=54). Furthermore, more surgeons preferred no antibiotics if packing wasn’t used (39.1%, n=52) compared to those who used packing (26.2%, n=34). This was similar to FESS operations where 23.2% (n=29) of surgeons preferred no antibiotics if they used packing as opposed to 38% (n=49), if no packing was used (Figure 1).
Cephazolin was the most common pre-operative antibiotic prescribed for septoplasty ± turbinoplasty (79.6%, n=39) and FESS (71.7%, n=33).
The most common post-operative antibiotic for septoplasty ± turbinoplasty was cephalexin (53.3%, n=32) followed by amoxicillin plus clavulanic acid (26.7%, n=16). Interestingly for FESS operations, both amoxycillin plus clavulanic acid and cephalexin were prescribed equally (32.3%, n=21 for both) by cephalexin (26.42%, n=14).
The majority of surgeons indicated prevention of infection as the main reason for prescribing antibiotics. For tonsillectomy ± adenoidectomy, surgeons also indicated less post-operative pain, lower post-operative bleeding and faster wound healing as other reasons for prescribing antibiotics (Table 1).
Table 1
| Variable | Prevention of infection | Less post-operative pain | Lower post-operative bleeding | Earlier return to normal activity | Faster wound healing | Total respondents |
| Tonsillectomy ± adenoidectomy | 53.2%; 25 | 27.7%; 13 | 38.3%; 18 | 14.9%; 7 | 6.4%; 3 | 47 |
| Grommets | 95.1%; 58 | 0.00%; 0 | 0.00%; 0 | 3.3%; 2 | 6.6%; 4 | 61 |
| Septoplasty ± turbinoplasty | 90.2%; 83 | 3.3%; 3 | 6.5%; 6 | 2.2%; 2 | 10.9%; 10 | 92 |
| FESS | 92.2%; 83 | 2.2%; 2 | 8.9%; 8 | 2.2%; 2 | 10%; 0 | 90 |
Sub-specialty operations
Figure 3 summarises the antibiotic preferences for various subspecialty operations.
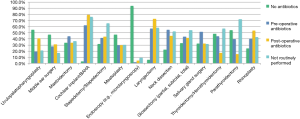
Most surgeons did not prescribe any antibiotics for endoscopic procedures involving the airway. For bronchoscopy, laryngoscopy, microlaryngoscopy, oesophagoscopy) 93.9% (n=107/114) of surgeons indicated they would not prescribe any antibiotics.
For neck dissections 22.4% (n=13/58) of surgeons indicated they do not prescribe any antibiotics where as 55.2% (n=32/58) indicated they prescribe pre-operative antibiotics. For surgery on the thyroid, parathyroid and salivary glands, pre-operative antibiotics were prescribed by 44.2% (n=23/52), 39.4% (n=13/33) and 51.8% (n=43/83) of surgeons respectively.
Interestingly, many surgeons did not prescribe any antibiotics for these operations (thyroid: 48.1%, n=25/52; parathyroid: 54.5%, n=18/33; salivary gland: 32.5%, n=27/83).
Prescribing practises were varied with different otological procedures.
For mastoidectomy, 33.3% (n=27/81) of surgeons prescribed no antibiotics while 44.4% (n=36/81) of surgeons preferred only pre-operative antibiotics.
Majority of the surgeons indicated they would not give antibiotics for middle ear surgery (myringoplasty, tympanoplasty, OCR) (47.2%, n=50/106).
For surgeons who performed cochlear implantation/insertion of bone-anchored hearing aids, 62.1% (n=18/29) indicated they prescribed pre-operative antibiotics.
For closed rhinoplasty, 27.6% (n=21/76) of surgeons preferred no antibiotics, while 38.2% (n=29/76) preferred pre-operative antibiotics.
Discussion
Our results indicate that while most surgeons did not prescribe any antibiotics for tonsillectomy ± adenoidectomy, a significant number prescribe post-operative antibiotics. Our findings were similar to previous studies in the USA where 30–40% of surgeons surveyed, prescribe antibiotics for these operations (10,12). Common reasons for prescribing antibiotics in this survey were prevention of infection, less post-operative pain and less post-operative bleeding. However, a Cochrane systematic review and meta-analysis by Dhiwakar et al. (6), found that antibiotics did not significantly reduce pain or need for analgesics. Furthermore, a meta-analysis did not show a significant reduction in delayed haemorrhage (6). However, there was a slight reduction in reducing number of patients with fever.
For septoplasty ± turbinoplasty and FESS (without packing) antibiotic prescribing was almost split between prescribing no antibiotics at all to prescribing post-operative antibiotics. In cases where packing was involved, preferences favored toward prescribing post-operative antibiotics. A similar survey of surgeons attending the American Rhinology Society demonstrated that 43% do not prescribe antibiotics for a routine FESS operation (13). However, survey of 442 otolaryngologists found that 70% of respondents prescribed antibiotics for endoscopic sinus surgery in the USA (12). Current Australian guidelines do not recommend use of antibiotics for routine uncomplicated FESS (8). Furthermore, a systematic review and meta-analysis of randomized controlled trials by Saleh et al. (14), found that antibiotic prophylaxis in FESS was associated with slightly lower but not significantly different rates of infection, symptoms scores and endoscopic scores.
For insertion of grommets, approximately half of the surgeons indicated they prescribed post-operative ototopical antibiotics only. The prescribing rates were higher compared to colleagues in the USA where approximately 85% of surgeons indicated they prescribed no pre and/or postoperative antibiotics (12).
A Cochrane systematic review and meta-analysis found that post-operative ototopical antibiotics were associated with a reduced incidence of post-operative otorrhea. However, the authors have recommended intervention only in patients with a high risk of ear discharge (15).
In this survey, prescribing practice was varied among subspecialties. For uncomplicated head and neck dissections, 21.54% of surgeons indicated they prescribed no antibiotics for these operations. This is comparable to previous surveys in the USA where 20% of respondents prescribed no antibiotics (12). Current Australian guidelines do not recommend antibiotic prophylaxis in uncomplicated neck dissections (8). While some studies do not support use of prophylactic antibiotics in uncomplicated neck dissection (16), there is level 1a evidence (17) supporting the use of prophylactic antibiotics for 24 hours (18). For thyroidectomy/hemithyroidectomy, 48.93% of the surgeons did not prescribe any antibiotics. This was slightly lower compared to a survey of endocrine surgeons in the USA where 62% did not prescribe any antibiotics (19). As routine thyroidectomy and parathyroidectomy are considered clean procedures, antibiotic prophylaxis is not recommended (20-22).
For otological procedures such as mastoidectomy and middle ear surgery (myringoplasty, tympanoplasty, OCR), our survey indicated that 33.3% and 47.2% did not prescribe antibiotics for these procedures respectively. This is similar to prescribing practices of colleagues in the USA (12). A Cochrane systematic review concluded that there is no evidence to support prophylactic use of antibiotics in clean otologic surgery (23). However, the role of antibiotics in cochlear implantation remains uncertain (24).
High-level studies are needed to assess the role of antibiotics in contaminated otologic surgeries. Similarly, the role of antibiotics in skull base surgeries remains uncertain due to the lack of randomised controlled trials (25).
Despite the low response rate (29%), this survey analyses the prescribing practices of Otolaryngologists, Head and Neck Surgeons in Australia and New Zealand allowing a snapshot of current trends within the specialty. Furthermore, our response rate compared favourably to previous surveys within the specialty, which ranged from 6–43% (9,12,13).
Inherent within the study is the response bias associated with survey design. Although most surgeons completed the entire survey, responses were low for some specialty procedures such as cochlear implantation where out of 120 responses, 91 did not routinely perform this procedure. This may reflect the small community of subspecialists who perform these procedures in Australia or New Zealand.
Overall, this study highlights a gap between current guidelines and prescribing practices in some areas of Otolaryngology Head and Neck Surgery. Although evidence in Australia and New Zealand on adherence to guidelines is sparse, previous studies in the Netherlands and USA have emphasised a need for increased awareness and implementation of guidelines in the future (9,10). Furthermore, the Australian Commission on Safety and Quality in Health Care have highlighted the need for increased collaboration with the Royal Australasian College of Surgeons to improve this gap (3).
Given the increased attention to and awareness of antibiotic resistance, further high level randomised controlled trials may help to determine the need and efficacy of antibiotics in various procedures within Otolaryngology, Head and Neck Surgery. For procedures where there is level 1a evidence regarding antibiotics use, e.g., tonsillectomy ± adenoidectomy, uncomplicated neck dissections and uncomplicated ear surgery, guidelines should reflect these findings with efforts to increase dissemination and awareness among specialists.
Conclusions
In conclusion, our data indicate a gap between current guidelines and antibiotic prescribing practices of Otolaryngologists, Head and Neck Surgeons in Australia and New Zealand. In addition to efforts focussing on awareness and dissemination of current guidelines, high-level studies are needed to establish robust evidence-based guidelines to aid in the decision-making process for surgeons.
Supplementary
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2019.02.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional ethical approval and informed consent were waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Responding To The Threats of Antimicrobial resistance: Australia's First National Antimicrobial Resistance Strategy 2015-2019. Available online: https://www.amr.gov.au/resources/national-amr-strategy
- Coombs GW, Daley DA, Thin Lee Y, et al. Australian Group on Antimicrobial Resistance Australian Staphylococcus aureus Sepsis Outcome Programme annual report, 2014. Commun Dis Intell Q Rep 2016;40:E244-54. [PubMed]
- Second Australian report on antimicrobial use and resistance in human health. Australia: Australian Commission on Safety and Quality in Health Care, 2017.
- Global Action Plan on Antimicrobial Resistance Geneva: World Health Organization 2015.
- Elective surgery waiting times 2016–17: Australian hospital statistics. Canberra: Australian Institue of Health and Welfare, 2017.
- Dhiwakar M, Clement WA, Supriya M, et al. Antibiotics to reduce post-tonsillectomy morbidity. Cochrane Database Syst Rev 2010;12:CD005607. [PubMed]
- Ottoline AC, Tomita S, Marques Mda P, et al. Antibiotic prophylaxis in otolaryngologic surgery. Int Arch Otorhinolaryngol 2013;17:85-91. [PubMed]
- Surgical Prophylxis. Therapeutic Guidelines Therapeutic Guidelines Ltd Melbourne, Australia. 2018. Available online: https://tgldcdp.tg.org.au.acs.hcn.com.au/viewTopic?topicfile=surgical-prophylaxis&guidelineName=Antibiotic&topicNavigation=navigateTopic#n7
- Aarts MC, van der Heijden GJ, Siegers C, et al. Awareness of, opinions about, and adherence to evidence-based guidelines in otorhinolaryngology. Arch Otolaryngol Head Neck Surg 2012;138:148-52. [Crossref] [PubMed]
- Padia R, Olsen G, Henrichsen J, et al. Hospital and Surgeon Adherence to Pediatric Tonsillectomy Guidelines Regarding Perioperative Dexamethasone and Antibiotic Administration. Otolaryngol Head Neck Surg 2015;153:275-80. [Crossref] [PubMed]
- Procedure list for Otolaryngology Head and Neck Surgery. Morbidity Audit and Logbook Tool. Royal Australisian College of Surgeons 2014. Available online: https://www.surgeons.org/media/20676730/2014-02-11_doc_ohns_procedure_list.pdf
- Valdez TA, Marvin K, Bennett NJ, et al. Current trends in perioperative antibiotic use: a survey of otolaryngologists. Otolaryngol Head Neck Surg 2015;152:63-6. [Crossref] [PubMed]
- Chandra RK, Conley DB, Kern RC. Prophylactic i.v. antibiotics in functional endoscopic sinus surgery: trends and attitudes of the American Rhinologic Society membership. Am J Rhinol Allergy 2009;23:448-50. [Crossref] [PubMed]
- Saleh AM, Torres KM, Murad MH, et al. Prophylactic perioperative antibiotic use in endoscopic sinus surgery: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2012;146:533-8. [Crossref] [PubMed]
- Syed MI, Suller S, Browning GG, et al. Interventions for the prevention of postoperative ear discharge after insertion of ventilation tubes (grommets) in children. Cochrane Database Syst Rev 2013;4:CD008512. [PubMed]
- Man LX, Beswick DM, Johnson JT. Antibiotic prophylaxis in uncontaminated neck dissection. Laryngoscope 2011;121:1473-7. [Crossref] [PubMed]
- Group OLoEW. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. Available online: http://www.cebm.net/index.aspx?o=5653
- Vila PM, Zenga J, Jackson RS. Antibiotic Prophylaxis in Clean-Contaminated Head and Neck Surgery: A Systematic Review and Meta-analysis. Otolaryngol Head Neck Surg 2017;157:580-8. [Crossref] [PubMed]
- Moalem J, Ruan DT, Farkas RL, et al. Patterns of antibiotic prophylaxis use for thyroidectomy and parathyroidectomy: results of an international survey of endocrine surgeons. J Am Coll Surg 2010;210:949-56. [Crossref] [PubMed]
- Lu Q, Xie SQ, Chen SY, Chen LJ, Qin Q. Experience of 1166 thyroidectomy without use of prophylactic antibiotic. Biomed Res Int 2014;2014:758432. [Crossref] [PubMed]
- Qin Q, Li H, Wang LB, et al. Thyroid surgery without antibiotic prophylaxis: experiences with 1,030 patients from a teaching hospital in China. World J Surg 2014;38:878-81. [Crossref] [PubMed]
- Avenia N, Sanguinetti A, Cirocchi R, et al. Antibiotic prophylaxis in thyroid surgery: a preliminary multicentric Italian experience. Ann Surg Innov Res 2009;3:10. [Crossref] [PubMed]
- Verschuur HP, de Wever WW, van Benthem PP. Antibiotic prophylaxis in clean and clean-contaminated ear surgery. Cochrane Database Syst Rev 2004;3:CD003996. [PubMed]
- Anne S, Ishman SL, Schwartz S. A Systematic Review of Perioperative Versus Prophylactic Antibiotics for Cochlear Implantation. Ann Otol Rhinol Laryngol 2016;125:893-9. [Crossref] [PubMed]
- Rosen SA, Getz AE, Kingdom T, et al. Systematic review of the effectiveness of perioperative prophylactic antibiotics for skull base surgeries. Am J Rhinol Allergy 2016;30:e10-6. [Crossref] [PubMed]
Cite this article as: Ahmadzada S, Wong EH, Naidoo Y. Antibiotic prescribing practices in otolaryngology head and neck surgery in Australia and New Zealand: a survey of 137 specialists. Aust J Otolaryngol 2019;2:11.