
Paediatric fish bone ingestion: a 10-year analysis at a tertiary pediatric hospital
Introduction
Foreign body ingestion and impaction remains a common problem both in paediatric and adult populations. In children, the highest incidence of impaction typically occurs between the ages of 6 months to 3 years, and the most common ingested foreign bodies include coins, small toys, button batteries and magnets (1).
Compared to adults, children in Western populations rarely ingest fish bones. However, previous literature has demonstrated that in countries with a higher fish intake, such as those in Asia, there is an increased incidence of fish bone ingestion and impaction in both children and adults (2). Fish bone ingestion poses significant potential hazards regardless of age, including visceral gastrointestinal perforation, secondary deep neck abscesses or mediastinitis and delayed oesophageal stenosis (3). Therefore, regardless of the demographics, fish bone ingestion necessitates accurate diagnosis and appropriate evidence-based management.
Paediatric fish bone ingestion presents its own unique challenges. Paediatric fish bone ingestion may provide a diagnostic challenge as a result of difficulties obtained with history-taking from the child, the event frequently unwitnessed by the carers and identification of the exact location of the bone. Although the size of the foreign body has not specifically been assessed in fish bone impactions, it is a well-established predictor for impaction risk in other foreign bodies such as coins (4,5). It therefore follows that foreign body and relative anatomical size may also be relevant in fish bones—that is, conservative management in anticipating spontaneous passage of smaller bones in adults may not be appropriate in children, a consequence of the smaller overall airway and oesophageal diameter. Furthermore, specific anatomical structures at risk of fish bone impaction may be proportionally larger in the child, including the palatine tonsils, tongue base, vallecula and pyriform fossa.
Impacted fish bones provide an investigative dilemma in the paediatric patient. Flexible fibre-optic nasendoscopy, a frequently used diagnostic technique in adults, may be logistically difficult and traumatic in an uncooperative child. Radiological investigations also have significant limitations. Anteroposterior (AP) and lateral airway X-rays have limited sensitivity and specificity as not all fish bones are radio-opaque and the soft tissue in the suprahyoid region may approach bone density (6,7). High resolution computed tomography (CT), while much more sensitive than plain X-rays (8,9), is relatively contraindicated in children due to concerns of radiation exposure (10).
Given these considerations, there is merit in evaluating the evidence regarding demographic characteristics, presenting symptoms and management options for fish bone ingestion in the paediatric population. Identifying the specific population at risk, the symptoms suggestive of impacted fish bone and the diagnostic utility of investigations may facilitate earlier diagnosis and reduce the requirement for unnecessary intervention without jeopardising patient safety. Understanding previous treatment experience and overall outcomes from managing fish bone ingestion may provide insight in determining which children should undergo urgent surgical removal and those where conservative, expectant management may be appropriate.
The aim of this study was therefore to perform a retrospective review of the presentation, investigation and management of fish bone ingestion presentations to an Australian tertiary paediatric hospital over a 10-year period.
Methods
Study design
A retrospective review of prospectively collected data was performed. Paper and electronic medical records were reviewed on consecutive patients who presented to The Children’s Hospital Westmead with suspected foreign body impaction over a 10-year period between January 1994 and December 2004.
Patients were identified using the International Coding of Diseases (ICD) Nine codes 933, 935.1, 935.2, 936, 938 and ICD Ten codes T17.2, T18.1 T18.2, T18.3, T18.4, and T18.9. Cases were then individually reviewed to exclude all foreign bodies other than fish bones.
Data collection
Data was collected from paper and electronic medical records for each included patient. Basic patient demographics including age and sex were recorded. The following clinical characteristics were collected: time to presentation from reported impaction in hours, whether the patient was symptomatic, the presenting symptoms reported, the type of investigation (such as flexible nasendoscopy, X-ray or CT imaging) and number of each investigation performed.
Location of the fish bone, if found, was recorded for each patient as well as the investigation utilised to make this diagnosis. The treatment undertaken for each patient was included, whether by expectant treatment or surgical intervention. Subsequent complications were also recorded.
Statistical analysis
Descriptive data analysis was performed in this cohort of patients. Patient demographic, clinical characteristics and outcomes were reported as percentages and raw numbers for categorical variables and means with standard deviations for continuous variables.
All data analysis was performed using Statistical Analysis Software 9.4 (SAS Institute, Cary, NC, USA).
Ethical approval
Ethical approval was obtained from the Western Sydney Local Health District Human Research Ethics Committee (WSLHD HREC; approval number MR-2004-12-02) prior to initiation of the study.
Results
Patient demographics
A total of 525 children were identified as presenting to the Children’s Hospital at Westmead with confirmed or suspected foreign body ingestion over the 10-year period. Suspicion of fish bone as the ingested foreign body represented only 8.0% of all of these foreign body presentations (n=42). Of these 42 children, the mean age was 6.2±4.0 years and 40.5% (n=17) were female. By contrast, the mean age for coin impactions was younger at 3.4 years (P<0.05). Mean time to presentation from reported time of ingestion was found to be 19 hours for fish bones compared to 2 hours for coin ingestions (P<0.05).
Presenting symptoms
Ninety three percent (n=39) of patients were found to be symptomatic at time of presentation. The most common presenting symptoms included: pain localised to the neck (38.5%, n=15); followed by pain localised to the oral cavity (25.6%, n=10); and foreign body sensation (25.6%, n=10.) The remaining children (7%, n=3) were asymptomatic at presentation. However, one child who was asymptomatic was found to have had an impacted fish bone located at the upper oesophagus.
Examination and investigations
Sixty-seven percent (n=28) of patients underwent either AP or lateral plain film X-ray. Of these, 3 patients were found to have a positive X-ray report of a foreign body consistent with fishbone. However, of patients who underwent X-ray, 35.7% (n=10) were found to have a fish bone present on oral examination or on flexible nasendoscopy. No children underwent more than one X-ray or CT scan.
Management
Forty point four percent (n=17) of patients were found to have a fish bone identified at time of review. Of these, 15 required removal, 1 passed spontaneously during the inpatient stay and 1 was regurgitated. Sixty-four point seven percent (n=11) were found to have been impacted in a palatine tonsil (n=10) or elsewhere in the oral cavity (n=1). All of these were successfully removed using a combination of tongue depressors, headlight, and forceps without requiring general anaesthetic.
Sixteen point seven percent (n=7) children underwent examination under general anaesthetic. Fifty-seven point one percent (n=4) of these were found to have a lodged fish bone, of which all were successfully removed with either direct laryngoscopy or rigid oesophagoscopy. Two of these fish bones were located at the upper oesophagus; one at the oropharynx; and the remaining one at the piriform fossa.
Outcomes and complications
No significant complications were identified in this cohort of patients. No children required a revision or second look procedure, and no children were re-admitted after discharge. One child experienced a mild mucosal erosion from fish bone removal which required analgesia and serial observation over 2 weeks until full recovery.
Discussion
Fish bones are one of the most common foreign bodies ingested requiring otolaryngology review and surgical intervention in adult populations, particularly in populations with high dietary intake of fish.
Diagnosing fish bone impaction in children can be problematic, even in those with a clear corroborated history of ingestion, as the fish bone often has passed by the time of definitive examination. Most ingested fish bones pass spontaneously without harm. However, potentially serious complications of an impacted fish bone can result, such as visceral perforation and abscess formation. As a result, timely, accurate diagnosis of whether a fish bone remains in-situ is critical in the appropriate management of these patients.
In this cohort, most children who presented to hospital were symptomatic. However, less than half were found to still have an impacted fish bone by the time of review or endoscopy. On the other hand, one child who was asymptomatic was found to have fish bone impacted just below the level of cricopharyngeus. Therefore, the authors suggest that presenting symptoms are typically present when a fish bone is present, but that a high index of suspicion must be maintained even in children who report being asymptomatic or minimally symptomatic, particularly given that children cannot always be relied upon to answer truthfully in an unfamiliar environment such as a hospital, for fear of the consequences of treatment. When symptoms are reported, however, the site often correlates with the location of the fish bone or site of injury, which may provide insight to the areas requiring focused examination. Of importance to note, however, is that when focal sensation is lost—this may indicate the level of foreign body may be oesophageal, below the level of cricopharyngeus.
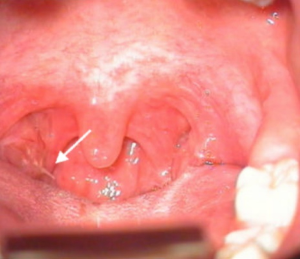
Most fish bones were found to be located within the oral cavity or oropharynx. Tonsillar hypertrophy is more common in children than in adults, particularly when compared to the overall posterior pharyngeal diameter (11). This may explain why tonsillar impaction was so common in this cohort, accounting for almost two thirds of removed fish bones (3) (Figure 1). This reinforces that thorough, well-illuminated oropharyngeal, with particular attention to examination of the tonsils should be routine. Tonsillar foreign bodies, when identified, may be removed at the bedside in the cooperative child, with no further need for intervention under general anaesthesia. An additional test of pressure point tenderness for foreign bodies in the cricoid area, is also of utility.
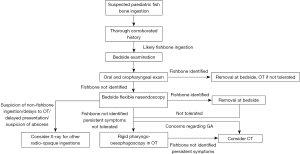
The authors suggest that bedside flexible nasendoscopy with topical local anaesthetic should be attempted in the first instance in all other children with a history of fish bone ingestion. It is then suggested that in patients where a fish bone is identified but cannot be removed at the bedside, or in patients who do not tolerate flexible nasendoscopy, rigid pharyngo-oesophagoscopy under general anaesthesia should be performed.
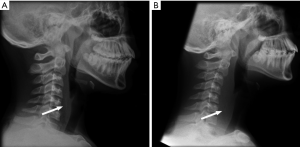
Plain film X-rays have limited diagnostic utility in fish bone impaction. Previous studies have reported detection rates as low as 30%, while other series report rates from 55% to 80% (6,7). X-rays typically have low sensitivity as not all fish bones are radio-opaque, although some radiolucent fishbones, if sufficiently large, can still be detected. Various overlapping soft tissue structures and normal variations of laryngeal cartilage and thyroid gland calcification patterns, which are more common in adults, may also mimic fishbones, although these are more often seen in adult populations. As a result, positive X-rays in children are relatively more specific compared to adults.
Therefore, the authors recommend children with positive X-rays should undergo endoscopic examination under anaesthesia. However, proceduralists should be aware that the identified fish bone may have passed spontaneously or less commonly, be regurgitated by the time of the procedure. X-rays may be useful in identifying soft tissue swelling of the airway, particularly in cases where presentation from ingestion is delayed (Figure 2). An important additional sign suggestive of potential injury on X-ray includes air lucency which may suggest abscess formation in the pharynx.
While no CT scans were performed in this series, both sensitivity and specificity for fish bones has previously been described in the literature as approaching 100% (9). CT imaging is often avoided in children due to concerns regarding excessive radiation exposure and, at our institution, diagnostic endoscopy either by the bedside or under general anaesthetic is considered more appropriate. However, with improved radiation protocols and safety, the authors would consider CT imaging in cases with a negative X-ray, persisting high index of clinical suspicion, and where clinical reasons existed to avoid endoscopy or general anaesthesia.
A suggested management algorithm for a child who presents with a suspected fishbone ingestion is outlined in Figure 3. In this flowchart, the utility of flexible nasendoscopy, X-ray and CT imaging is considered in the diagnostic workup.
While fish bone impaction is a common clinical problem, it is an issue that is seldom discussed in the literature. A study performed by Ngan et al. (3) examined 358 fish bones ingested by patients with mean age 41.5 years. Of these, they found only 21 patients had a fish bone located in the oral cavity while in the remaining patients who underwent endoscopic examination, 82 were found to have a more distal region fish bone requiring removal. This study also confirmed that while symptomatology is often not useful in predicting the presence of a fish bone (the positive predictive values of most symptoms were under 0.50), the site of symptoms was more accurate in predicting for the location and laterality of the foreign body. Plain radiograph examinations were also of limited usefulness in detecting a fishbone with a sensitivity 0.32. However, where a fishbone was identified on X-ray, there was high likelihood of one being identified on endoscopy, with a specificity of 0.91.
The literature on fish bone impaction in paediatric populations is even more limited. To our knowledge, only one study performed by Lim et al. (12) examines this topic. In their retrospective study based at a Korean tertiary Emergency Department, 416 children aged under 15 years were assessed. Interestingly, this comprised more than half of all paediatric foreign body presentations over the 13-year period of the study, likely reflecting the increased fish consumption of the population. They found that older children and shorter time to presentation predicted for the requirement for fish bone removal. The types of ingested fish, types of presenting symptoms, the presence of radio-opaque X-ray findings and the presence of parent witnessed ingestion were not statistically significant (P=0.20, 0.38, 0.16 and 0.39 respectively).
The main limitation of this study is its retrospective design, particularly given that the data was collected approximately 10 years ago. This has the only readily available data on fishbone ingestion over a 10-year period in Australia. There is a potential that the incidence of fishbone ingestion in children is no longer representative of current trends. Nevertheless, this study contains a sizeable cohort of an Australian experience that the authors believe outlines treatment paradigms that may remain relevant to current practice.
Conclusions
Fish bones are uncommon foreign bodies ingested by children. In this cohort, most impacted fish bones were identified within the oral cavity or oropharynx and were able to be removed at the bedside in the cooperative child without the need for further endoscopic examination or surgical intervention. This may be secondary to the increased proportional size of the palatine tonsils in children and reinforces the importance of thorough oral and oropharyngeal examination in the diagnostic workup.
Plain X-rays appear to have limited diagnostic utility in predicting for fish bone impaction in children. While presence and nature of symptoms are useful when reported, a high index of suspicion should be maintained when children report to be asymptomatic.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2019.05.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was obtained from the Western Sydney Local Health District Human Research Ethics Committee (WSLHD HREC; approval number MR-2004-12-02) prior to initiation of the study. Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dereci S, Koca T, Serdaroğlu F, et al. Foreign body ingestion in children. Turk Pediatri Ars 2015;50:234-40. [Crossref] [PubMed]
- Nandi P, Ong GB. Foreign body in the oesophagus: review of 2394 cases. Br J Surg 1978;65:5-9. [Crossref] [PubMed]
- Ngan JH, Fok PJ, Lai EC, et al. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 1990;211:459-62. [Crossref] [PubMed]
- Singh N, Chong J, Ho J, et al. Predictive factors associated with spontaneous passage of coins: A ten-year analysis of paediatric coin ingestion in Australia. Int J Pediatr Otorhinolaryngol 2018;113:266-71. [Crossref] [PubMed]
- Reilly JS, Walter MA, Beste D, et al. Size/shape analysis of aerodigestive foreign bodies in children: a multi-institutional study. Am J Otolaryngol 1995;16:190-3. [Crossref] [PubMed]
- Devarajan K, Voigt S, Shroff S, et al. Diagnosing Fish Bone and Chicken Bone Impactions in the Emergency Department Setting: Measuring the System Utility of the Plain Film Screen. Ann Otol Rhinol Laryngol 2015;124:614-21. [Crossref] [PubMed]
- Evans RM, Ahuja A, Rhys Williams S, et al. The lateral neck radiograph in suspected impacted fish bones--does it have a role? Clin Radiol 1992;46:121-3. [Crossref] [PubMed]
- Goh BK, Tan YM, Lin SE, et al. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol 2006;187:710-4. [Crossref] [PubMed]
- Akazawa Y, Watanabe S, Nobukiyo S, et al. The management of possible fishbone ingestion. Auris Nasus Larynx 2004;31:413-6. [Crossref] [PubMed]
- Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012;380:499-505. [Crossref] [PubMed]
- Papaioannou G, Kambas I, Tsaoussoglou M, et al. Age-dependent changes in the size of adenotonsillar tissue in childhood: implications for sleep-disordered breathing. J Pediatr 2013;162:269-74.e4. [Crossref] [PubMed]
- Lim CW, Park MH, Do HJ, et al. Factors Associated with Removal of Impactted Fishbone in Children, Suspected Ingestion. Pediatr Gastroenterol Hepatol Nutr 2016;19:168-74. [Crossref] [PubMed]
Cite this article as: Wong E, Cheng AT, Aggarwala S, Chong J, Duvnjak M, Azimi F, Cope D, Singh N. Paediatric fish bone ingestion: a 10-year analysis at a tertiary pediatric hospital. Aust J Otolaryngol 2019;2:16.


