
Reliability of estimating blood loss in epistaxis
Introduction
Epistaxis, or nosebleed as it is known to patients, is a common presenting complaint to general practitioners and emergency departments accounting for 1.7 emergency department visits per 1,000 (1). From the Greek word “dripping”, there are two distinctions of epistaxis; anterior or posterior and 85% of cases are idiopathic (2). It is estimated that 60% of adults experience epistaxis, and in the UK, it is the number one Ear, Nose and Throat (ENT) presentation to emergency departments (3,4). Blood loss in epistaxis can range from small volume to catastrophic amounts depending on site of bleeding, patient factors and measures to arrest haemorrhage. A review of Scottish admissions over a 10-year period found that epistaxis accounted for a third of ENT admissions with an average age of 70 (5). This is most likely given the increase in medical diseases that require anticoagulation; aspirin is an independent risk factor for epistaxis (6). In patients presenting with epistaxis a prompt assessment of blood loss is required. This is because blood loss derived from initial haematocrit levels is unreliable, young patients have a smaller circulating volume with greater cardiovascular compensatory abilities and elderly patients may be taking cardiovascular or haematological system altering medications (7). Use of visual estimation remains an immediate and useful adjunct to patient assessment. We sought to determine the accuracy of clinical staff and students in estimating blood loss in hypothetical epistaxis from visual aids and whether the accuracy changes based on type of profession, duration of profession and blood spilled. We present the following article in accordance with the STROBE reporting checklist (available http://dx.doi.org/10.21037/AJO-19-53).
Methods
Ethical considerations
Ethics was obtained from the local site Human Research Ethics Committee (HREC/17/QPCH/482). Human blood was not used due to the cost and restrictions in handling.
Study design/participants
A visual aid survey was developed using commercially acquired defrosted pig blood spilled on ten common medical and household products (Figure 1). This was conducted, with department approval, in a mortuary room in the pathology department of Sunshine Coast University Hospital. This survey was then electronically distributed over a 1-month period (via SurveyMonkey) amongst medical and paramedic Facebook groups, asking them to best estimate the amount of blood on the product. Informed consent was collected on initiation of survey. Descriptive statistics were used to summarise the demographics of participants. A number scale was used for participants to select the exact estimated volume to the nearest millilitre. All photographs had a centimetre scale for reference of object size.
Outcomes
The accuracy of a participant to estimate the amount of an individual blood spill was assessed as both the difference and percent accuracy for each spill. In addition, each spill was classified as either correct, underestimated or overestimated.
Statistical methods
To assess whether the size of the spill affected accuracy of estimation, paired t-tests were employed for each of the repeated items. Three items had two different blood volumes spilled on them.
The mean of the absolute differences across all images was calculated to assess overall accuracy. Linear regression models were used to test whether there was a relationship between overall accuracy and profession or years of experience in profession. All analysis was carried out in R 3.5 an online statistical computer (8). Categorical variables were summarised with counts and percentages, while mean, standard deviation median and inter-quartile range were calculated for continuous variables.
Results
A total of 192 respondents competed the survey, 17 were excluded for partial completion with 175 valid responses included in this work. The profession demographic breakdown consisted mainly of doctors (78%), followed by paramedics (17%), and nurses (5%). Of note is that 83% of paramedics were students compared with 4% of doctors identifying as students. A further breakdown of years in profession can be seen in Table 1. Ninety-four percent of participants reported having seen a nose bleed.
Table 1
| Characteristic | Profession, n [%] | |||
|---|---|---|---|---|
| Doctor (N=137) | Nurse (N=9) | Paramedic (N=29) | Overall (N=175) | |
| Years in profession | ||||
| Student | 6 [4] | 1 [11] | 24 [83] | 31 [18] |
| 0–3 | 46 [34] | 0 [0] | 1 [3] | 47 [27] |
| 3–5 | 27 [20] | 1 [11] | 2 [7] | 30 [17] |
| 5–10 | 36 [26] | 2 [22] | 1 [3] | 39 [22] |
| 10+ | 22 [16] | 5 [56] | 1 [3] | 28 [16] |
| Seen a nose bleed | ||||
| No | 8 [6] | 0 [0] | 2 [7] | 10 [6] |
| Yes | 129 [94] | 9 [100] | 27 [93] | 165 [94] |
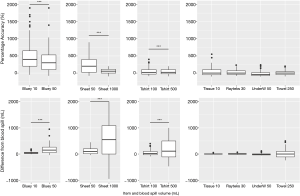
Table 2 summarises the results for each individual spill. The majority of participants overestimated the size of the spill for all items, with the exception of the men’s underpants and the bath towel where the majority underestimated the spill size. The most correctly estimated spill was the 10 mL spill on tissues, which was estimated correctly by 30% of participants. Estimating blood spills on the blueys proved the most difficult with a noticeably higher mean and variation in the absolute percent estimation accuracy (Table 2 and Figure 1).
Table 2
| Volume (mL) | Item | Number [%] | Absolute percent accuracy [%] | ||||
|---|---|---|---|---|---|---|---|
| Correct | Under | Over | Mean ± SD | Median [IQR] | |||
| 10 | Ten tissues | 53 [30] | 56 [32] | 66 [38] | 68±84 | 50 [0–100] | |
| 10 | Bluey | 7 [4] | 6 [3] | 162 [93] | 476±426 | 400 [200–650] | |
| 30 | Rayteks | 19 [11] | 78 [45] | 78 [45] | 57±50 | 50 [33–67] | |
| 50 | Sheet/mattress | 20 [11] | 29 [17] | 136 [78] | 234±223 | 237 [60–400] | |
| 50 | Men’s underpants | 23 [13] | 107 [61] | 45 [26] | 56±41 | 60 [20–80] | |
| 50 | Bluey | 6 [3] | 18 [10] | 151 [86] | 350±303 | 300 [100–530] | |
| 100 | T-shirt | 20 [11] | 58 [33] | 97 [55] | 84±80 | 60 [30–100] | |
| 250 | Bath towel | 18 [10] | 85 [49] | 71 [41] | 49±38 | 40 [20–68] | |
| 500 | T-shirt | 9 [5] | 60 [34] | 106 [61] | 62±58 | 52 [23–100] | |
| 1000 | Sheet/mattress | 19 [11] | 31 [18] | 124 [71] | 78±58 | 75 [30–109] | |
Size of spill
Figure 2 shows that size of spill does affect the accuracy of participants estimates, indicating the difference between the actual value and the estimate increases with size of spill, while the percentage accuracy decreases with size of spill. Two size blood spills were tested on blueys, t-shirts and sheets/mattresses. Paired t-test showed significant differences between accuracy and size of spill in both the raw difference and the absolute percentage error (Figure 2).
Years in profession
The mean percentage accuracy across all items and volumes was significantly affected by the number of years in profession. Compared to the reference group with 0–3-year experience all those with additional experience were on average significantly better at estimating blood loss. There was no statistical difference between students and those with 0–3-year experience (Table 3).
Table 3
| Years in profession* | Coefficient | SD | P value |
|---|---|---|---|
| 3–5 years | −60.1 | 22.9 | 0.009 |
| 5–10 years | −50.9 | 21.2 | 0.017 |
| 10+ | −50.5 | 23.3 | 0.032 |
| Student | 32.3 | 22.6 | 0.155 |
*, reference is 0–3 years.
Profession
Given that the majority of paramedics were students, and there is a significant difference seen by years of experience, to test whether there was a difference between profession a subset excluding students was used. No statistically significant difference was observed between the professions (Table 3).
Discussion
Epistaxis is a common presentation both to Emergency Departments and ENT specialists; however, in the literature only one study has reported on estimation of blood loss in epistaxis (9). This study used flour and food colouring to stimulate actual blood applied on to some household objects and also in reservoirs. They found that larger volumes tended to be under-estimated and there was no difference in seniority of clinician, however this study had a small sample size (n=32), with an even smaller subset of participants at different seniority levels, and was likely underpowered to make this conclusion. Only 6 clinicians were included and there was no comment on statistical methodology. In our study there was a statistical difference in estimation with clinicians’ accuracy increasing with years of experience.
We found that size of spill does effect the accuracy of participants estimates, where the difference between the actual value and the estimate increased with size of spill, and the percentage accuracy decreased with size of spill.
The most correctly estimated volume was on a household object (tissues) at a small volume. This may be due to professional and personal experience of blood visualised on this product and in keeping with small volumes more likely to be correctly estimated. In contrast, the “bluey”, a common medical product was most difficult to estimate blood from. This could be consistent with its absorbable nature.
Comparable papers are to be found in the obstetric field with estimation of blood loss in postpartum haemorrhage. In postpartum haemorrhage, studies have reported that at smaller volumes there is a tendency to overestimate and underestimate at greater volumes (10,11). However, in obstetric medicine, given that post-partum haemorrhage is defined as >500 mL in vaginal delivery and 1,000 mL in caesarean delivery, then the expected total blood loss will, by definition, be assumed to be greater (12). In the obstetric field, visual estimation has been shown to be inaccurate and in opposition of laboratory values. Many studies, using stimulated blood loss on common products have shown a varying reliability of approximation (13).
This study has demonstrated a significant increase in accuracy in blood loss estimation with years in profession. This implies that experience improves reliability. Studies focusing on post-partum haemorrhage have demonstrated the reliability and importance of visual estimation education. Several have shown that use of a visual aid guide or reference tool can improve approximated blood loss (14,15). Interestingly this improved the outcomes regardless of level of experience. This was facilitated through development of a stylised pictogram simulating episodes of blood loss. Participants were then provided with either online or in person education to better guide them in estimating blood loss.
Recognising the limitations of clinicians’ estimation of blood loss and developing strategies to better educate assessment has many implications. Blood loss estimation is useful in both the elective and emergency setting; operative blood loss is an important predictor of mortality (16,17). Blood loss estimation, particularly in children, can have significant diagnostic implications; a Queensland coronial inquest into a child’s death from a missed button battery ingestion and subsequent aoro-oesophageal fistula highlighted the need for reliable blood loss estimation and did identify a significant impact in this patients care due to the underestimation of blood loss (18). There are several ways postulated to estimate blood loss including visual estimation, direct measurement, gravimetric and comparison of pre and post haemoglobin levels (19). Around 5–15% of epistaxis patients will require surgical intervention for their bleeding often in the acute setting (20). Stahl et al. sought to compare blood loss estimation using expert assessment and pre- and post-haemoglobin levels. They found that haemoglobin based blood volume calculations were poor predictors of overall blood loss and only closely approximated other measurement tools over a period of more than 24 hours (17). Thus for patients who present with an acute bleed and require surgical intervention within the next 24 hours their laboratory studies will not appropriately reflect their total volume lost. Furthermore, a review of the management of epistaxis from 2009 suggests that not all epistaxis patients require formal laboratory measurements, only those with severe haemorrhage (21). An accurate estimation of blood loss is therefore essential to triage patients who may require additional investigations or more judicious resuscitation.
There were several limitations of this study. Whilst pigs and humans share similar coagulation profiles the porcine blood in this study had been frozen and thawed (22). Evidence suggests that whilst coagulability is altered during this process, the difference is most likely non-clinical (23). Results would be most accurately collected if this study was repeated using fresh, human blood, however, we acknowledge that this poses significant logistical and ethical issues.
Secondly, the majority of paramedic and nursing participants in this study were students who had fewer years of experience. After excluding students only eight nurses and five paramedics remain, and the study is underpowered to test the hypothesis comparing the medical professions. As the survey gave different ranges of blood loss from which participants selected their response there is inherent bias as answers could not be given out of those ranges. This may have altered some participants responses.
Conclusions
Epistaxis is a common presentation to Emergency Departments and General Practitioners. Over-estimation of blood loss is common and has implications for excessive resuscitation of patients and the inappropriate use of blood products with possible side effects. Studies in postpartum haemorrhage have suggested that exposure to visual aids of blood loss can improve clinician estimations and guide resuscitation. We hypothesised that certain populations will estimate blood loss poorly and that those with a longer period of clinical practice would be more reliable. Based on this study’s findings that with experience, estimation reliability improves and that smaller volumes are better quantified we would postulate that a visual aid could be validated and used as a measurement and education tool for primary care physicians and first responders to guide epistaxis management. These results have implications for post tonsillectomy bleeding and per rectal bleeding; both areas that could be explored further.
Acknowledgments
Funding: None
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/AJO-19-53
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/AJO-19-53). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the local site Human Research Ethics Committee (HREC/17/QPCH/482). Human blood was not used due to the cost and restrictions in handling. The authors confirm that written informed consent was obtained from the participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pallin DJ, Chng YM, McKay MP, et al. Epidemiology of Epistaxis in US Emergency Departments, 1992 to 2001. Ann Emerg Med 2005;46:77-81. [Crossref] [PubMed]
- Ross PD, McClymont LG. Epistaxis. Surgery (Oxford) 2006;24:296-8. [Crossref]
- Melia L, McGarry GW. Epistaxis: update on management. Curr Opin Otolaryngol Head Neck Surg 2011;19:30-5. [Crossref] [PubMed]
- Morgan DJ, Kellerman R. Epistaxis: evaluation and treatment. Prim Care 2014;41:63-73. [Crossref] [PubMed]
- Walker TWM, Macfarlane TV, McGarry GW. The epidemiology and chronobiology of epistaxis: an investigation of Scottish hospital admissions 1995–2004. Clin Otolaryngol 2007;32:361-5. [Crossref] [PubMed]
- Livesey JR, Watson MG, Kelly PJ, et al. Do patients with epistaxis have drug‐induced platelet dysfunction? Clin Otolaryngol Allied Sci 1995;20:407-10. [Crossref] [PubMed]
- Ashburn JC, Harrison T, Ham JJ, et al. Emergency Physician Estimation of Blood Loss. West J Emerg Med 2012;13:376-9. [Crossref] [PubMed]
- A language and environment for statistical computing. R Foundation for Statistical Computing. 2018. Available online: https://www.R-project.org/
- Beer HL, Duvvi S, Webb CJ, et al. Blood loss estimation in epistaxis scenarios. J Laryngol Otol 2005;119:16-8. [Crossref] [PubMed]
- Razvi K, Chua S, Arulkumaran S, et al. A comparison between visual estimation and laboratory determination of blood loss during the third stage of labour. Aust N Z J Obstet Gynaecol 1996;36:152-4. [Crossref] [PubMed]
- Dildy GA 3rd, Paine AR, George NC, et al. Estimating blood loss: can teaching significantly improve visual estimation? Obstet Gynecol 2004;104:601-6. [Crossref] [PubMed]
- Homcha BE, Mets EJ, Goldenberg MDF, et al. Development and Assessment of Pictorial Guide for Improved Accuracy of Visual Blood Loss Estimation in Cesarean Delivery. Simul Healthc 2017;12:314-8. [Crossref] [PubMed]
- Natrella M, Di Naro E, Loverro M, et al. The more you lose the more you miss: accuracy of postpartum blood loss visual estimation. A systematic review of the literature. J Matern Fetal Neonatal Med 2018;31:106-15. [Crossref] [PubMed]
- Al-Kadri HM, Dahlawi H, Al Airan M, et al. Effect of education and clinical assessment on the accuracy of post partum blood loss estimation. BMC Pregnancy Childbirth 2014;14:110. [Crossref] [PubMed]
- Zuckerwise LC, Pettker CM, Illuzzi J, et al. Use of a novel visual aid to improve estimation of obstetric blood loss. Obstet Gynecol 2014;123:982-6. [Crossref] [PubMed]
- Wu WC, Schifftner TL, Henderson WG, et al. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery. JAMA 2007;297:2481-8. [Crossref] [PubMed]
- Stahl DL, Groeben H, Kroepfl D, et al. Development and validation of a novel tool to estimate peri-operative blood loss. Anaesthesia 2012;67:479-86. [Crossref] [PubMed]
- Hutton J. Inquest into the death of Summer Alice STEER. Queensland Coroners Court 2015. (2013/2322). Available online: https://www.courts.qld.gov.au/__data/assets/pdf_file/0004/444289/cif-steer-sa-20151103.pdf
- Schorn MN. Measurement of Blood Loss: Review of the Literature. J Midwifery Womens Health 2010;55:20-7. [Crossref] [PubMed]
- McDermott AM, O’Cathain E, Carey BW, et al. Sphenopalatine Artery Ligation for Epistaxis: Factors Influencing Outcome and Impact of Timing of Surgery. Otolaryngol Head Neck Surg 2016;154:547-52. [Crossref] [PubMed]
- Schlosser RJ. Clinical practice. Epistaxis. N Engl J Med 2009;360:784-9. [Crossref] [PubMed]
- Sondeen JL, de Guzman R, Amy Polykratis I, et al. Comparison between human and porcine thromboelastograph parameters in response to ex-vivo changes to platelets, plasma, and red blood cells. Blood Coagul Fibrinolysis 2013;24:818-29. [Crossref] [PubMed]
- Gosselin RC, Dwyre DW. Determining the effect of freezing on coagulation testing: comparison of results between fresh and once frozen-thawed plasma. Blood Coagul Fibrinolysis 2015;26:69-74. [Crossref] [PubMed]
Cite this article as: Grigg S, Maunder J, Betz-Stablein B, Llewellyn S. Reliability of estimating blood loss in epistaxis. Aust J Otolaryngol 2020;3:15.



