Is mastoiditis being over-diagnosed on computed tomography imaging? —radiological versus clinical findings
Introduction
The diagnosis of acute mastoiditis (AM) has been disputed. Luntz and colleagues (1) described AM as: acute otitis media (AOM) on otoscopy with local mastoid inflammatory findings (pain, erythema, sagging of postero-superior wall of external auditory canal and auricular protrusion) or mastoid inflammatory changes with radiological or surgical findings of AM +/− evidence of AOM on otoscopy. Other authors (2,3) have suggested that diagnosis requires all of otoscopic findings of AOM, inflammatory changes over the mastoid process and radiological findings of AM.
The clinically important distinction in AM compared to middle ear infections is the development of periostitis or osteitis (4), as patients with bony destruction have an increased risk of intra or extra cranial complications. Incipient mastoiditis involves periostitis without any bony septa destruction whilst coalescent mastoiditis involves bony erosion secondary to osteitis involving the bony mastoid septa or mastoid cortex (2,4).
There has been a significant reduction in the incidence of serious complications stemming from AOM or chronic otitis media (OM) since the advent of antibiotics and improved medical care (2). Over the last century the incidence of AM as a complication of AOM has reduced from 50% to 0.4% (5). Despite being uncommon, AM can be associated with potential serious complications (2). Thus, primary and emergency care physicians often have a high index of suspicion regarding the diagnosis of “mastoiditis”.
In suspected cases of AM, computerised tomography (CT) of the temporal bone can be a helpful aid for diagnosis and evaluation of potential complications. CT imaging can display information on the state of the middle ear cavity, the mastoid air cells and evaluate for intra- and extra-cranial complications. An understanding of CT findings is important both for clinician-based risk stratification and management. Furthermore, an appreciation of the pathophysiology of middle ear and mastoid disease is important in predicting the potential limitations of temporal bone imaging.
Approximately 85% of children experience at least 1 episode of AOM with middle ear inflammation and exudate formation (2). This inflammatory exudate is not confined to the middle ear space but extends to involve the mastoid air cells secondary to open communications via the aditus ad antrum. It is thus expected that AOM will show evidence of mastoid opacification on CT imaging as a consequence of this contiguous system.
CT imaging of the mastoid segment of the temporal bones is the preferred modality for evaluating the mastoid air cells. It is generally performed without contrast and presented in bony settings with bone appearing white and all else appearing a degree of grey. It is important to note that one cannot easily differentiate opacification in this region and causes may include infective exudate, mucosal thickening/oedema, sterile fluid, granulation tissue or cholesteatoma. One such example is in the setting of otitis media with effusion (OME). OME reflects a delay in clearance of middle ear effusion from the middle ear cleft and mastoid air cells leading to persisting fluid. CT imaging will show opacification but not bony erosion as seen with coalescent mastoiditis (6-8).
Previous observations have indicated that there is a high incidence of CT temporal bone imaging undertaken in the evaluation of AM as it is helpful in diagnosis complications of AM and can be useful for surgical planning (4). The aim of this study was to evaluate the importance of the presence of mastoid opacification on CT imaging and it’s the relationship with the clinical picture. It is hypothesized that opacification of the mastoid air cell system may not necessarily reflect coalescent changes or eventuate a diagnosis of AM. We present the following article in accordance with the STROBE reporting check list (available at http://dx.doi.org/10.21037/ajo-20-24).
Methods
This study was reviewed by the Metro North Human Research Ethics Committee Chairperson and deemed compliant with the National Health and Medical Research Council guidance “Ethical Considerations in Quality Assurance and Evaluation” 2014, Ref No: HREC/2020/QRBW/61419. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
A retrospective analysis of all CT imaging of the brain, paranasal sinuses, temporal bones and internal auditory meatus (IAM) was undertaken at three hospitals constituting the Royal Brisbane and Women’s Hospital (RBWH) and Sunshine Coast Health District (SCHD) between the 31st December 2016 and 31st of December 2018. The RBWH treats patients above 16 years of age in a metropolitan area whilst the SCHD deals with patients of all ages.
CT scanning was performed with either Siemens SOMATOM Definition Flash Dual Source scanner or Siemens SOMATOM Definition AS Single Source Scanner. Scanning protocol was varied as either CT sinus, CT IAM or CT brain protocol with reconstructed slice thickness of 0.5/0.3 mm for CT IAM; 0.5/0.4 mm for CT brain; and multi-planar reconstructions of 1/2 mm in axial and coronal planes for CT IAM’s and brain; 1.5/3 mm for CT sinuses as per standard hospital protocol.
Retrospective chart review was conducted and the overall incidence of radiological diagnosis of mastoiditis was calculated from reviewing formal reports of these studies. A database of all patients with reported mastoiditis on CT imaging was created.
Patients included in the review had underwent CT imaging performed displaying the entire middle ear cleft and mastoid air cells, within the time period of data collection. Legible medical records must have been available that included medical notation from the review leading to CT request in which there was a clear stipulation of the examination findings and the reason for CT request.
Patients were excluded with background of mastoidectomy, a differential of encephalocele or meningocele on CT imaging or patients with cholesteatoma on CT imaging.
Chart and imaging review focused on documenting any current or past otological symptoms or interventions, infection and treatment, both medical or surgical. Treatment plans were reviewed in depth if otological in nature or noted as “medical treatment” to encompass non-otological treatments.
Examination findings, particularly otoscopy and examination of the pinna and peri-auricular region was noted, as were patients who were referred to Otolaryngology. The presence or absence of fevers, meningitis or intracranial conditions was documented.
Statistical analysis of the findings was undertaken using SPSS software.
The aims of the statistical data analyses were to examine whether there is a significant association between the radiological and clinical diagnosis of mastoiditis, to examine whether there is a significant association between radiological and clinical diagnosis of mastoiditis and the age of the subject, to examine if there is a significant association between the radiological finding of mastoiditis and the treatment undertaken and to find if there is a significant association between the clinical and radiological diagnosis of mastoiditis and the clinical findings of otalgia, otorrhoea, mastoid tenderness, hearing concerns, temperatures, and otoscopic changes.
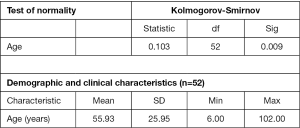
Statistical analysis of the data was undertaken using the IBM SPSS statistics software package. Data was examined for data entry errors. Nominal data has been expressed as n-valued variables (e.g., 1 = no mastoid tenderness; and 2 = mastoid tenderness) and continuous data has been used when appropriate (e.g., age). A Kolmogorov-Smirnov test of normality was conducted to establish if the subject age of the sample can be assumed to be from a normally distributed population. The aims of the data analysis have been addressed using Spearman’s rank non-parametric correlation coefficients and Chi-square test of independence as appropriate.
Results
In total, 1,946 CT scan reports and image sets that visualized the mastoid segment of the temporal bones were reviewed.
Of the 1,946 scans, 52 scans (2.7%) had reported a finding of mastoiditis. These reports were compiled by a total of 11 radiologists.
The imaging reviewed included all IAM, paranasal sinus, temporal bone and brain CT scans. This was purposefully undertaken to review the incidence of reported mastoiditis seen in patients undergoing CT imaging that included their temporal bones regardless of whether they had suspicion of otological pathology.
A retrospective review of the 52 patients who had radiological finding of mastoiditis on CT imaging was undertaken. Data from these patients was statistically analysed. A Kolmogorov-Smirnov test of normality indicated that subject age can be assumed to come from a normally distributed population at alpha =0.001 (Figure 1). Therefore, the subsequent use of parametric statistics and techniques is justified for age.
Demographic and clinical characteristics
Demographic and clinical characteristics of the subjects are summarised in Figure 1 and outlined in Table 1. The average age of the subjects at the time of the examination was 55.93 years (SD =25.95 years). The average age of patients with an actual diagnosis of AM was 6.7 years (SD =0.94 years), based on the 3 patients diagnosed and treated for AM. This highlights the tendency for diagnosis to occur in a younger age group. Spearman’s rank non-parametric correlation coefficient was used to test for statistically significant association between the CT diagnosis of mastoiditis and the age of the subject, and true diagnosis of mastoiditis and the age of the subject. The results indicated that the correlations between CT diagnosis of mastoiditis and the age of the subject (r=−0.202, P=0.039), and true diagnosis of mastoiditis and the age of the subject (r=−0.289, P=0.003) were both significant at alpha =0.05. Therefore statistically, younger patients are more likely to have opacification of the mastoid and mastoiditis (see Table 1).
Table 1
| Age (years) | CT indication | Diagnosis | Treatment |
|---|---|---|---|
| 6 | Mastoiditis | Mastoiditis | S; IV Abs; PO Abs |
| 6 | Mastoiditis | Mastoiditis | IV Abs; PO Abs |
| 8 | Mastoiditis | Mastoiditis | S; IV Abs; PO Abs; anticoagulation |
| 8 | Mastoiditis | OM | IV Abs; PO Abs |
| 13 | Mastoiditis | OM | PO Abs |
| 13 | Mastoiditis | OM | PO Abs |
| 14 | Mastoiditis | OM | PO Abs |
| 15 | Mastoiditis | OM | PO Abs |
| 16 | Mastoiditis | OM | PO Abs |
| 19 | Mastoiditis | OM | IV Abs; PO Abs; Top |
| 23 | Sinusitis | AS | PO Abs |
| 28 | Mastoiditis or OE | OE | Top |
| 30 | Mastoiditis or OE | OE | Top |
| 31 | Mastoiditis or OE | OE | Top |
| 32 | Hearing loss | NIO | Nil |
| 32 | Otitis media | NIO | Nil |
| 32 | Mastoiditis or OE | OE | PO Abs; Top |
| 32 | Sinusitis | AS | PO Abs |
| 37 | Neurological | NOC | Medical |
| 37 | Mastoiditis | OE | Top |
| 41 | Otitis media | OM | Medical |
| 43 | Otitis externa | OM | Nil |
| 43 | Mastoiditis | OE | PO Abs; Top |
| 43 | Hearing loss | NIO | Nil |
| 45 | Mastoiditis | OE | Top |
| 47 | Sinusitis | AS | Medical |
| 49 | Exostosis | NIO | Nil |
| 56 | Neurological | NOC | Medical |
| 56 | Mastoiditis | OM | Nil |
| 56 | Otitis externa | NIO | Nil |
| 63 | Sinusitis | AS | Medical |
| 64 | Neurological | NOC | Medical |
| 65 | Otitis externa | OE | Top |
| 65 | Trauma | NOC | Medical |
| 70 | Hearing loss | NIO | Nil |
| 71 | Neurological | NOC | Medical |
| 72 | Mastoiditis | OE | PO Abs; Top |
| 75 | Neurological | NOC | Medical |
| 75 | Exostosis | NIO | Nil |
| 76 | Neurological | NOC | Medical |
| 77 | Trauma | NOC | Medical |
| 78 | Neurological | NOC | Medical |
| 79 | Neurological | NOC | Medical |
| 80 | Neurological | NOC | Medical |
| 81 | Trauma | NOC | Medical |
| 82 | Neurological | NOC | Medical |
| 84 | Neurological | NOC | Medical |
| 86 | Hearing loss | NIO | Nil |
| 88 | Neurological | NOC | Medical |
| 90 | Neurological | NOC | Medical |
| 94 | Neurological | NOC | Medical |
| 94 | Neurological | NOC | Medical |
AS, acute sinusitis; NOC, non-otological cause; OE, otitis externa; OM, otitis media; NIO, non-infective ontological cause; S, sinusitis; IV Abs, intravenous antibiotics; PO Abs, oral antibiotics; Top, topical antibiotics; Medical, medical team management.
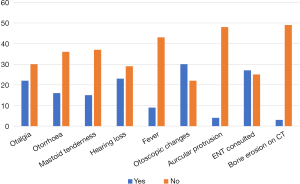
As summarised in Figure 2, 42.3% of the subjects had otalgia (n=22), 30.8% had otorrhoea (n=16), 28.8% had mastoid tenderness (n=15), 57.7% had otoscopic abnormalities (n=30), and 17.3% had a documented fever (n=9). Otoscopic findings included an inflamed external auditory canal in 15.4% of the subjects (n=8), inflammatory tympanic membrane changes in 32.7% of the subjects (n=17), and non-infective observations such as exostoses, tympanic membrane perforation and tympanosclerosis in 13.5% of subjects (n=7).
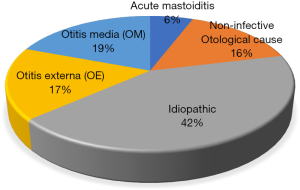
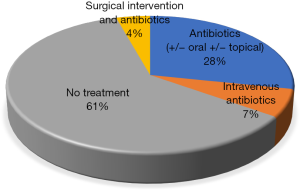
Of the 52 patients, 30 (57.7%) were clinically diagnosed with an otological pathology. Of these a small number were investigated for non-infective otological pathology (n=8, 15.4%), which included three patients (5.8%) undergoing CT for sudden onset hearing loss; three patients (5.8%) post trauma and two patients (3.8%) with exostosis. Seventeen-point-there percent (n=9) of patients were diagnosed with otitis externa (OE), 19.2% with OM (n=10). Importantly, only 5.8% (n=3) were diagnosed with AM (see Figure 3). The majority of patients (n=28, 53.8%) with a radiological diagnosis of mastoiditis did not require otological treatment. Of those that did, 25.0% (n=13) required oral +/− topical antibiotics and 5.8% (n=3) received intravenous antibiotics (see Figure 4). Only 2 patients (n=3.8%) required surgical intervention.
Interestingly three patients (5.8%) classified as non-otological causes had a diagnosis of acute sinusitis that may have contributed to acute eustachian tube dysfunction and subsequent middle ear effusion.
Of the 22 patients (42.3%) investigated for non-otological concerns, 3 patients (5.8%) had documented fever but none of these had documented otalgia, mastoid tenderness, hearing loss, auricular protrusion, otorrhoea or abnormal otoscopy findings. In a retrospective review we rely on clinicians notes to adequately examine patients and provide appropriate documentation. None of these patients had any infective changes noted on ear exam or ear exam findings were omitted altogether. As a limitation to this study, reliance on clinicians with potentially limited experience examining ears or taking otology specific histories is noted.
Three patients (5.8%) with a radiological diagnosis of mastoiditis were subsequently diagnosed with AM. Common clinical features of these patients were mastoid tenderness, bulging and erythematous tympanic membrane, auricular protrusion. All of these patients required ENT admission and treatment. Fevers were documented in 2 of 3 patients (66.7%). In all cases CT temporal bone imaging revealed mastoid septa erosion. Importantly, none of the other 49 patients showed evidence of bony erosion.
One patient diagnosed with complicated AM and underwent cortical mastoidectomy, grommet insertion and prolonged course of intravenous antibiotics. The associated extra-dural abscess and sigmoid sinus thrombosis resolved with above treatment.
The other two patients with diagnosed AM were treated with intravenous antibiotics and topical preparations following grommet insertion. Both patients had a prolonged course of oral antibiotics on discharge.
Of note, 19 (36.5%) of the 52 CT request forms specified mastoiditis as a condition to be excluded, all three patients with AM were included in this group (Table 1).
In total, formal ENT consultation was requested in 27 patients (51.9%). Five patients (9.6%) were admitted, including those diagnosed with AM. One patient diagnosed with AOM had clinical findings of auricular protrusion and was treated with 2 days of intravenous antibiotics prior to discharge on oral antibiotics. One (1.9%) patient diagnosed with AOE was admitted for pain management and intravenous antibiotics.
Twelve patients (23.1%) were commenced on oral antibiotics, topical antibiotics or both following ENT review and subsequently discharged home.
The remaining ten patients referred to ENT were either referred for outpatient follow-up or were discharged without antibiotic therapy.
Overall, from the 1,946 CT scan reports and images reviewed, 52 scans (2.7%) had reported mastoiditis. Only 5.8% (3 of 52) ended up with a specialist diagnosis of AM. Therefore, 94.2% of CT reports with reported mastoiditis did not end up with a clinical diagnosis of AM. Only 3 patients of the 52 were then diagnosed with AM by an ENT team following these scans. Most others had OE, media or idiopathic reasons for these findings.
Discussion
AM manifests in a continuum from early mastoid and middle ear suppuration with periostitis and osteitis to widespread bony destruction of mastoid trabeculae, inner and outer cortex erosion with extension of suppuration beyond the mastoid with associated potential complications. CT imaging showing mastoid opacification is often reported as mastoiditis however emerging evidence reaffirms that AM is a rarity even in the setting of mastoid opacification.
Previous studies have displayed the accuracy of CT imaging for diagnosing mastoiditis in the setting of bony erosion. Migirov reviewed 37 patients with a history of middle ear disease and correlated CT findings with intraoperative findings to assess accuracy (3). The study found that CT had a sensitivity of 97% and a positive predictive value of 94% in the diagnosis of complicated AM based on hallmark findings of osseous destruction of mastoid air cells (3). Simsek and colleagues reviewed pre-operative CT findings of 50 patients with COM and correlated results with findings at mastoidectomy (9). In this study CT was highly sensitive to the presence of mastoid pneumatisation (96%) and temporal bone destruction (95%).
Palma et al. performed a single centre retrospective review of 62 adults treated for mastoiditis from 1992 to 2010 (5). The inclusion criteria for a diagnosis of mastoiditis in this study was based on common diagnostic criteria; specifically, post-auricular swelling, erythema or tenderness, protrusion of the auricle, evidence of co-existent or recent otitis media, fever and supportive findings on high resolution temporal bone CT scanning (5). A diagnosis based on radiological findings alone was included when evidence of mastoid empyema with bony coalescence or cortical erosion was detected. The overall incidence of mastoiditis was 0.99 cases per 100,000 adults in this study (5). Additionally, in 40% of the mastoiditis cases reviewed, temporal bone CT imaging showed opacification within the mastoid without evidence of bony destruction. In this subgroup diagnosis relied on clinical signs of mastoid inflammation or fevers (5). This suggests bone erosion is not always present in patients treated for mastoiditis and that non-specific opacification of the mastoid on CT may be the only radiological finding in incipient mastoiditis in the non-contrast CT scan.
Interestingly, mastoid opacification has also been consistently detected in patients with uncomplicated acute otitis externa (AOE). Brennan and Saadia-Redleaf (10) reviewed 209 patients diagnosed with and treated for uncomplicated AOE. Of these patients, 27 had CT imaging of the temporal bones with 29 involved ears. Seventy-nine percent of those imaged patients had fluid within their middle ear cleft, mastoid air cells or both (10). Of the scans, one unaffected contralateral ear also had mastoid effusion present without symptoms of either AOE or OM. Although, as suggested in the study, the patients selected for CT investigation were likely done so due to severity of symptoms, the inclusion criteria did specify that patients had an uncomplicated course and recovered with standard treatment (10). Consequently, mastoid opacification occurs in OE and this was certainly seen in this study with over 19% of patients being diagnosed with OE.
Recently there have been studies showing the rates of incidental mastoid opacification particular in the paediatric population. Placanica and Anderson (11) reviewed 767 CT scans retrospectively in a paediatric cohort and found a prevalence rate between 5–20%, with peak prevalence in those aged between 0–4 years of age. Lafferty et al. (12) also found a high incidental mastoid opacification rate of 14.2% in the paediatric population. This has been reaffirmed by research looking into incidental mastoid opacification in children based on magnetic resonance imaging (MRI) imaging. Again, increased prevalence is seen in children of younger age groups with prevalence of over 40% noted in children under 2 years of age (13). While these reviews focused solely on a paediatric population, our study reviews a broad population age demographic with an average age around 56 years old. Our findings suggest higher rates of mastoid opacification and mastoiditis win younger age groups, consistent with these recent papers. This fits with the known increased risk of mastoiditis in younger populations, prevalence of eustachian tube dysfunction in children and higher rates of middle ear infections seen in paediatric populations (3,11-13).
Sayal et al. (14) undertook a retrospective review of temporal bone CT imaging to identify prevalence of incidental mastoid opacification. This study only reviewed patients without otological symptoms. In this asymptomatic patient cohort, they found none of the patients who were reported to have mastoiditis or mastoid effusion were diagnosed with mastoiditis and only 8.8% of the cohort had evidence of any otological disease. Comparatively, this study excluded any patient having imaging done for any ear symptoms or findings prior to imaging which may explain the reason no true diagnosis was found.
Our study is unique in comparison to these recent studies in that it looks at a wide range of patients, to mimic the wide range of indications for CT imaging that includes mastoids in the hospital system. It includes patients undergoing CT scans for otological symptoms across all age groups. The results are however consistent with what was found in the paediatric and symptoms free cohorts reviewed in these recent studies showing mastoid opacification to be a low yield finding in isolation for a diagnosis of AM.
CT imaging of the temporal bones in patients with suspected mastoiditis does certainly play a role in their management. Consideration of surgical management in AM is often influenced by the presence of coalescence or bony erosion seen on CT imaging. Owing to its enhanced ability to view bony details, is described as the gold standard for imaging in suspected mastoiditis whilst MRI is seen as an adjunct for assessment of possible intracranial complications (2,5,15,16).
Although there is extensive literature supporting the accuracy of CT imaging in mastoiditis in the presence of bony erosion (3-5,9,17), this research has looked specifically at the finding of mastoid opacification itself. An understanding of the pathophysiology of middle ear and mastoid disease suggests that opacification of the mastoid air cells may be an extension of uncomplicated AOM or OE rather than more serious AM (1,2,5).
Radiological reporting of mastoiditis is not in keeping with the clinical entity of AM. Based on this study, mastoid effusion or radiological reports of mastoiditis in the asymptomatic patient without evidence of bony erosion on CT is unlikely to require treatment beyond conservative approach (oral antibiotics or watch and wait). Overall, 2.7% of CT scans showed mastoid opacification even in patients without acute middle ear symptoms. Although this number is low, given the ease of access and varied indications for CT imaging that will include the mastoid segment of the temporal bone, this will likely become pertinent to many primary care and emergency clinicians as well as Ear Nose and Throat doctors. This number is higher in younger populations as seen in this study and recent research (Figure 1, Table 1).
In summary, opacification of mastoid air cells on CT imaging is a non-specific finding seen in a range of otologic conditions from the common; OE, OM and in the rare; acute mastoiditis. Furthermore, there are a number of cases where this is a completely incidental finding. It is suggested from the analysis of available literature and the findings of this review that the radiological reporting of this finding would be better stated as “mastoid opacification for clinical correlation” if no bony erosion is seen.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-24
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-24). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved Human Research Ethics Committee Metro North Hospital & Health Service HREC/2020/QRBW/61419 and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Luntz M, Brodsky A, Nusem S, et al. Acute mastoiditis--the antibiotic era: a multicenter study. Int J Pediatr Otorhinolaryngol 2001;57:1-9. [Crossref] [PubMed]
- El-Kashlan H, Harker L, Shelton C, et al. Complications of Temporal Bone Infections. in: Flint P, Haughey B, Lund V, et al. Cummings otolaryngology. 6th edition. Philadelphia: Saunders Elsevier, 2015 2015;140:1979-98.
- Migirov L. Computed tomographic versus surgical findings in complicated acute otomastoiditis. Ann Otol Rhinol Laryngol 2003;112:675-7. [Crossref] [PubMed]
- Vazquez E, Castellote A, Piqueras J, et al. Imaging of complications of acute mastoiditis in children. Radiographics 2003;23:359-72. [Crossref] [PubMed]
- Palma S, Bovo R, Benatti A, et al. Mastoiditis in adults: a 19-year retrospective study. Eur Arch Otorhinolaryngol 2014;271:925-31. [Crossref] [PubMed]
- Maroldi R, Farina D, Palvarini L, et al. Computed tomography and magnetic resonance imaging of pathologic conditions of the middle ear. Eur J Radiol 2001;40:78-93. [Crossref] [PubMed]
- Habesoglu TE, Habesoglu M, Toros SZ, et al. How does childhood otitis media change the radiological findings of the temporal bone?. Acta Otolaryngol 2010;130:1225-9. [Crossref] [PubMed]
- Bluestone CD, Klein JO. Intratemporal complications and sequelae of otitis media. In: Bluestone CD, Stool SE. editors. Pediatric otolaryngology. Philadelphia, PA: Saunders, 1983:549-52.
- Kucur C, Simşek E, Kuduban O, et al. The clinical value of temporal bone tomography in chronic otitis media. Kulak Burun Bogaz Ihtis Derg 2013;23:21-5. [Crossref] [PubMed]
- Brennan TE, Saadia-Redleaf MI. Occult middle ear and mastoid fluid in acute otitis externa. Laryngoscope 2012;122:2067-70. [Crossref] [PubMed]
- Placanica T, Anderson S. Incidental finding of mastoid opacification in computed tomography imaging of the asymptomatic paediatric population. J Laryngol Otol 2019;133:588-91. [Crossref] [PubMed]
- Lafferty DJ, Cohn JE, McKinnon BJ. Incidental mastoid opacification on computed tomography in the pediatric population. Int J Pediatr Otorhinolaryngol 2020;128:109688. [Crossref] [PubMed]
- Singh S, Rettiganti MR, Qin C, et al. Incidental mastoid opacification in children on MRI. Pediatr Radiol 2016;46:704-8. [Crossref] [PubMed]
- Sayal NR, Boyd S, Zach White G, et al. Incidental mastoid effusion diagnosed on imaging: Are we doing right by our patients?. Laryngoscope 2019;129:852-7. [Crossref] [PubMed]
- Choi SS, Lander L. Pediatric acute mastoiditis in the post-pneumococcal conjugate vaccine era. Laryngoscope 2011;121:1072-80. [Crossref] [PubMed]
- Polat S, Aksoy E, Serin GM, et al. Incidental diagnosis of mastoiditis on MRI. Eur Arch Otorhinolaryngol 2011;268:1135-8. [Crossref] [PubMed]
- Vlastarakos PV, Kiprouli C, Pappas S, et al. CT scan versus surgery: how reliable is the preoperative radiological assessment in patients with chronic otitis media? Eur Arch Otorhinolaryngol 2012;269:81-6. [Crossref] [PubMed]
Cite this article as: Pastuszek A, Lomas J, Grigg C, De R. Is mastoiditis being over-diagnosed on computed tomography imaging? —radiological versus clinical findings. Aust J Otolaryngol 2020;3:31.