
Unilateral choanal atresia first diagnosed in adulthood and repaired via endoscopic posterior septectomy—a case series and review of the literature
Introduction
Congenital choanal atresia (CA) is defined as the developmental absence of the normal communication between the posterior nasal cavity and the nasopharynx. It has a reported incidence of 1:5,000–1:8,000 live births and may be associated with several congenital anomalies and syndromes, most commonly the CHARGE (coloboma, heart defects, choanal atresia, mental retardation, genital and ear malformations) syndrome (1-4). Bilateral congenital CA is rare and typically presents in the first days of life. It is potentially life threatening, and may present as cyclical respiratory distress and cyanosis that is relieved by crying, as well as feeding difficulty. On the other hand, unilateral atresia is far more common and accounts for around two-thirds of cases (5). It typically presents later, during infancy or childhood, with unilateral nasal obstruction, ipsilateral rhinorrhoea or mouth breathing (6). Very rarely, with only a few cases documented in the literature, does unilateral atresia present in adulthood (5,7).
The embryological aetiology of congenital CA continues to elude consensus. Four proposed theories have been suggested: (I) persistence of the buccopharyngeal membrane at weeks four to six of gestation; (II) abnormal migration of mesoderm causing the formation of nasochoanal adhesions; (III) persistence of the nasobuccal membrane of Hochstetter; and (IV) misdirection of neural crest migration and subsequent mesodermal flow (3,8,9). Review of the anatomical characteristics of CA has reported that approximately 70% are bony whilst the remainder are a mixed bony-membranous atresia (10).
The three most commonly described approaches to surgical correction of CA are trans-palatal; trans-nasal and trans-septal (5-7,11-15). Since 1990, with the increasing use of endoscopic nasal surgery, endoscopic-assisted repairs have been increasingly described (16). However, to date, no single approach has been demonstrated to be superior. A Cochrane review examining factors predicting successful repair in CA repair failed to identify sufficient literature to draw meaningful recommendations as to the advantages or disadvantages of any specific surgical technique (14). Other adjunctive treatments, including use of stenting, topical mitomycin C, or the form of routine post-operative care following sinonasal procedures (such as saline douching) remain controversial (17-20). The evidence regarding the management of CA in the adult population is even weaker.
Nevertheless, the primary goals of treatment are to provide adequate choanal patency, with a low rate of re-stenosis. Secondary goals include minimising post-operative pain, procedure complication profile and length of hospital stay. In this case series, we describe the work up, management and outcomes in four patients with unilateral CA who remained undiagnosed until adulthood and were successfully managed surgically. To the best of our knowledge this is the largest case series in the literature of previously undiagnosed adults managed via endoscopic posterior septectomy.
In compiling this case series, the authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Due to the low risk nature of the reporting, the local research and ethics committee waived the need for informed consent. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-63).
Case presentation
Case 1
A 37-year-old female was referred to a tertiary otolaryngology centre with chronic right-sided rhinorrhoea and nasal obstruction refractory to medical management. Fibreoptic nasendoscopy demonstrated a blind ending right nasal cavity. CT of the paranasal sinuses demonstrated a right-sided mixed bony-membranous CA (Figure 1). The left choana was noted to be patent.
Repair was undertaken under general anaesthesia via an endoscopic-assisted trans-septal approach. Topical decongestion was performed using Moffet’s solution (cocaine, adrenaline, sodium bicarbonate and saline) and submucosal infiltration to the septum and inferior turbinates with 2% lignocaine in 1:80,000 adrenaline. A right endoscopic powered turbinate reduction was first performed to improve access. A left hemitransfixion incision was made and a subperichondrial flap raised to the osseocartilaginous junction. The quadrilateral cartilage was disarticulated from the bony septum and the flap was continued posteriorly to the atretic plate on the right side, and until the choana was reached on the left. A posterior bony septectomy was performed from within the septal pocket, preserving the septal mucosal flaps, utilizing a combination of an endoscopic drill with a 4 mm cutting burr, a 6 mm osteotome and Jansen-Middleton Septum forceps. The mucosa on the anterior aspect of the atretic plate was incised and elevated laterally and the bony atretic plate was then drilled from medial to lateral back to the level of the lateral nasal wall. The intact mucosa of the left posterior septum was then incised in an axial plane superiorly and a coronal plane anteriorly, then laid down over the midline floor of the nose to cover all exposed bone. Excessive mucosa of the right posterior septum was debrided to avoid mucosal overlap. A routine cartilaginous septoplasty and left turbinoplasty was then performed to address the left sided nasal obstruction. No nasal packing was required.
The patient was admitted overnight and discharged home the following day on oral antibiotics and saline nasal spray, to avoid flap displacement. She was reviewed at 1-week post-operatively for nasal toilet and commenced on a saline irrigation via a rinse bottle 4 times per day. The patient subsequently attended further second weekly review for 6 weeks for repeat nasal toilet. At 6 months post-surgery the patient had complete resolution of symptoms and a patent choana bilaterally with no evidence of restenosis.
Case 2
A 65-year-old male was referred to the outpatient clinic with symptomatic unilateral CA in the setting of multiple right-sided congenital craniofacial anomalies. The patient had suffered from chronic unilateral rhinorrhea, nasal obstruction and was also diagnosed with obstructive sleep apnea following polysomnography, but was unable to tolerate continuous positive airway pressure (CPAP) via a nasal mask. Flexible nasendoscopy demonstrated a right-sided atretic plate, while the left choana was patent. A non-contrast CT scan of the paranasal sinuses demonstrated a mixed membranous-bony atretic plate with thickening of the vomer and bowing of the pterygoid process of the sphenoid. There was associated hypoplasia of the right maxilla and orbit, along with a cleft palate.
Repair was undertaken via the endoscopic, trans-septal approach. Decongestion was achieved using topical Moffet’s solution and injection infiltration with 2% lignocaine in 1:80,000 adrenaline. The left hemitransfixion incision and septal flaps were raised in the same manner as for case 1. The patient required more extensive bone removal and to achieve a better angle of approach with both the osteotomes and the endoscopic drill, septal mucosal incisions were made early in the case. The septal flaps were laid down laterally along the floor of the nose for their protection and bone removal was then undertaken trans-nasally rather than trans-septally. Once this was complete the septal flap from the non-atretic left side was laid across the posterior floor of the nose, and excessive mucosa on the right was debrided (Figure 2A,B).
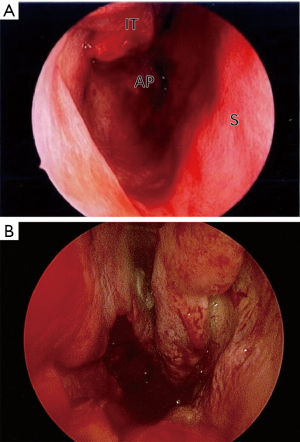
This patient was admitted overnight and discharged the following morning with instructions for nasal saline spray and oral antibiotics. The patient was reviewed at 1 week following surgery and second weekly thereafter for endoscopic examination and nasal toilet. Saline bottle irrigation was commenced. There was no evidence of re-stenosis or granulation tissue formation at 6-month follow up and this patient also experienced complete resolution of his pre-operative symptoms.
Case 3
A 28-year-old female was referred with several years of right-sided nasal obstruction, purulent rhinorrhoea, facial pain and hyposmia. Rigid nasendoscopy demonstrated a right-sided CA. CT of the paranasal sinuses suggested that this was purely membranous.
The patient subsequently underwent CA repair utilising a completely trans-nasal endoscopic approach. A posterior septectomy was performed and the membrane debrided without the need to cover denuded bone with mucosal flaps. In addition to the procedure, the patient also underwent bilateral uncinectomy, middle meatal antrostomy and anterior ethmoidectomies, and inferior turbinoplasties for concomitant chronic rhinosinusitis. The patient was discharged the following day on 5 days of oral antibiotics, 3 days of oxymetazoline spray and regular saline douches. The patient was reviewed for nasal toilet at 2, 8 and 20 weeks. At final follow-up (5 months), the patient was discharged with excellent anatomical and clinical patency.
Case 4
A 55-year-old female was referred with a long history of bilateral nasal obstruction and purulent rhinorrhoea refractory to medical treatment. Nasendoscopy demonstrated a blind ending right nasal cavity and CT scans confirmed a right sided mixed bony-membranous atretic plate (Figure 3). The left choana was patent. The patient underwent initial septoplasty and inferior turbinoplasty performed to improve access to the nasopharynx. Using CT image navigation, the atretic plate was drilled out in an endoscopic trans-nasal fashion until the posterior choana was reestablished. On this occasion a posterior septectomy was not performed, and a nasopharyngeal airway (NPA) was inserted and secured to the septum to stent open the reconstruction. The patient was discharged on oral antibiotics, oxymetazoline spray and regular saline douches.
The patient underwent NPA removal at 2 weeks post-operatively. At 3 months post-operatively there was clinical and anatomical patency. However, at 6 months post-operatively the patient remained symptom free, but there was evidence of early re-stenosis on flexible nasendoscopy. At 12 months post-operatively the patient had clinical relapse and required revision surgery. On this occasion, a posterior septectomy was undertaken in an endoscopic trans-nasal fashion, and choanal splints were left in situ for 4 weeks post-operatively. At 16 weeks following revision surgery the patient had durable anatomical and clinical patency, and continues to present for ongoing follow up.
Discussion
Unilateral congenital CA is typically identified in the neonate. However, unlike bilateral CA, it rarely may remain undiagnosed until adulthood. It is also less likely to be associated with other congenital anomalies and syndromes (21). One series suggests 53.2% of cases of unilateral CA occur de novo. In the remainder of cases the CHARGE syndrome remains the most commonly associated syndrome (21). For unilateral CA, many authors advocate delaying operative management to avoid both the technical challenges of operating in the neonatal nasal cavity as well as damage to midfacial growth centers (22). Whilst most surgical repair occurs in childhood or adolescence, there are several series that include adult patients (5,7,15,20,23). In paediatric patients, low-level evidence has suggested that comorbid gastro-oesophageal reflux, younger age at repair and the surgical learning curve all increased the rate of restenosis following repair. However, no previous studies have examined the factors that predict successful surgical repair in the adult population (24).
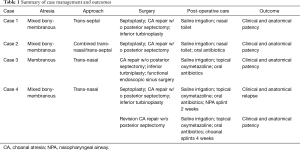
The goals of surgery should be to provide enduring relief from symptoms with minimal morbidity and restenosis. Since 1990 endoscopic assisted trans-nasal procedures have been described with overall good success (16,25). Some authors have advocated for a simple trans-nasal atresia puncture and dilation of the neochoanae using a device such as a urethral sound, while others have suggested that posterior septectomy, including resection of up to half of the bony posterior septum is necessary to ensure enduring patency (7,20,22,23). This series appears to support the latter—the only case that did not undergo initial posterior septectomy (case 4) experienced restenosis, and ultimately required revision surgery involving resection (Table 1). Wormald, in a series of 16 mostly paediatric patients, advocates an even more extensive endoscopic assisted trans-septal approach where, in addition to a posterior septectomy, resection of the posterior wall of the maxillary sinus and medial pterygoid plate as well as the floor, anterior wall and body of the sphenoid is performed (15).
Full table
Other authors have also emphasized the importance of meticulous preservation of nasal mucosal flaps so as to not leave any denuded bone, which may promote the formation of granulation tissue, and subsequent restenosis (7,15,20). However, Durmaz conducted a meta-analysis of 238 cases in 20 studies and revealed that the use of a mucosal flap did not influence the postoperative success rate (5). In fact, only a history of previous surgery for CA appeared to significantly decrease the post-operative success rate.
The decision to utilize either a trans-septal or trans-nasal approach in this study was dependent on several premorbid anatomical factors. Utilising the trans-septal approach allows the operator to address any septal deformities and improve exposure. Is also reduces the need for additional incisions to raise nasal mucosal flaps from the atretic plate at the level of the choana. The trans-nasal approach was utilised when there was adequate trans-nasal access without the need for a septoplasty and when the bony atretic plate was so dense as to necessitate the use of an endoscopic drill.
Several authors have also examined the role of adjuncts to surgical repair. Mitomycin C has gained popularity in recent years owing to its reported anti-fibroblastic properties and use in laryngotracheal stenosis (18). However, its efficacy in CA remains contentious (26). A retrospective review by Carter demonstrated that Mitomycin C was associated with decreased granulation tissue formation and a decreased need for revision surgery (17). However, other studies failed to demonstrate the same benefit (4,27). None of the patients in the present study underwent Mitomycin C treatment, however, all ultimately experienced persistent successful outcomes. The use of routine post-operative stenting is also controversial. Some studies have suggested that stents are associated with longer hospital length of stay, increased granulation tissue formation, biofilm formation and pressure necrosis (4,19). The effect of stents on the rate of restenosis and need for revision surgery varies amongst different studies (4,7,19).
Despite the successful outcomes, there remain limitations to this study. With only four cases, most of which underwent treatment following a similar paradigm, there cannot be any meaningful comparison of techniques or statistical analysis. Additionally, all cases were managed by tertiary rhinologists, and therefore these results may not necessarily be extrapolated to the general otolaryngologist. Nevertheless, the published literature on CA surgery in adults is extremely porous, and the documented experience with these four patients is of value. This case series demonstrates the operative and perioperative aspects considered by two rhinologists when managing unilateral adult CA.
Further research, with higher powered and potentially prospective studies should be pursued to greater clarify the optimal surgical and adjunctive techniques for CA in adults. When sufficient studies with adequate numbers are identified, consideration for pooled analysis in the form of systematic review and meta-analysis should also be pursued.
Conclusions
Undiagnosed unilateral CA is an uncommon finding in adults that should be suspected in patients with long standing unilateral obstruction and ipsilateral mucoid rhinorrhea. It is readily identified using routine nasendoscopy and confirmed with sinus CT scan. In this series of patients, surgical correction using endoscopic assisted posterior septectomy appeared to provide enduring patency and patient satisfaction. Whilst the optimal surgical technique and adjunctive treatment for this condition has not yet been established, this case series suggests that failure to resect the posterior vomer may be a predictive factor for re-stenosis. Further, higher-powered studies are required to establish more conclusive evidence on this topic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-63
Peer Review File: Available at http://dx.doi.org/10.21037/ajo-20-63
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-63). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Due to the low risk nature of the reporting, the local research and ethics committee waived the need for informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Flake CG, Ferguson CF. Congenital choanal atresia in infants and children. In: Archives of Otolaryngology. Chicago: American Medical Association, 1965.
- Menasse-Palmer L, Bogdanow A, Marion RW. Choanal atresia. Pediatr Rev 1995;16:475-6. [Crossref] [PubMed]
- Hengerer AS, Brickman TM, Jeyakumar A. Choanal atresia: embryologic analysis and evolution of treatment, a 30-year experience. Laryngoscope 2008;118:862-6. [Crossref] [PubMed]
- Newman JR, Harmon P, Shirley WP, et al. Operative management of choanal atresia: a 15-year experience. JAMA Otolaryngol Head Neck Surg 2013;139:71-5. [Crossref] [PubMed]
- Durmaz A, Tosun F, Yldrm N, et al. Transnasal endoscopic repair of choanal atresia: results of 13 cases and meta-analysis. J Craniofac Surg 2008;19:1270-4. [Crossref] [PubMed]
- Kwong KM. Current updates on choanal atresia. Front Pediatr 2015;3:52. [Crossref] [PubMed]
- Karligkiotis A, Farneti P, Gallo S, et al. An Italian multicentre experience in endoscopic endonasal treatment of congenital choanal atresia: Proposal for a novel classification system of surgical outcomes. J Craniomaxillofac Surg 2017;45:1018-25. [Crossref] [PubMed]
- Hengerer AS, Strome M. Choanal atresia: a new embryologic theory and its influence on surgical management. Laryngoscope 1982;92:913-21. [Crossref] [PubMed]
- Verma SP, Geller K. Persistent buccopharyngeal membrane: report of a case and review of the literature. Int J Pediatr Otorhinolaryngol 2009;73:877-80. [Crossref] [PubMed]
- Brown OE, Pownell P, Manning SC. Choanal atresia: a new anatomic classification and clinical management applications. Laryngoscope 1996;106:97-101. [Crossref] [PubMed]
- McIntosh WA. Trans-septal approach to unilateral posterior choanal atresia. J Laryngol Otol 1986;100:1133-7. [Crossref] [PubMed]
- Samadi DS, Shah UK, Handler SD. Choanal atresia: a twenty-year review of medical comorbidities and surgical outcomes. Laryngoscope 2003;113:254-8. [Crossref] [PubMed]
- Schoem SR. Transnasal endoscopic repair of choanal atresia: why stent? Otolaryngol Head Neck Surg 2004;131:362-6. [Crossref] [PubMed]
- Cedin AC, Atallah AN, Andriolo RB, et al. Surgery for congenital choanal atresia. Cochrane Database Syst Rev 2012.CD008993. [PubMed]
- Wormald PJ, Zhao YC, Valdes CJ, et al. The endoscopic transseptal approach for choanal atresia repair. Int Forum Allergy Rhinol 2016;6:654-60. [Crossref] [PubMed]
- Stankiewicz JA. The endoscopic repair of choanal atresia. Otolaryngol Head Neck Surg 1990;103:931-7. [Crossref] [PubMed]
- Carter JM, Lawlor C, Guarisco JL. The efficacy of mitomycin and stenting in choanal atresia repair: a 20 year experience. Int J Pediatr Otorhinolaryngol 2014;78:307-11. [Crossref] [PubMed]
- Gangar M, Bent JP. The use of mitomycin C in pediatric airway surgery: does it work? Curr Opin Otolaryngol Head Neck Surg 2014;22:521-4. [Crossref] [PubMed]
- Strychowsky JE, Kawai K, Moritz E, et al. To stent or not to stent? A meta-analysis of endonasal congenital bilateral choanal atresia repair. Laryngoscope 2016;126:218-27. [Crossref] [PubMed]
- Saraniti C, Santangelo M, Salvago P. Surgical treatment of choanal atresia with transnasal endoscopic approach with stentless single side-hinged flap technique: 5 year retrospective analysis. Braz J Otorhinolaryngol 2017;83:183-9. [Crossref] [PubMed]
- Burrow TA, Saal HM, de Alarcon A, et al. Characterization of congenital anomalies in individuals with choanal atresia. Arch Otolaryngol Head Neck Surg 2009;135:543-7. [Crossref] [PubMed]
- Kim H, Park JH, Chung H, et al. Clinical features and surgical outcomes of congenital choanal atresia: factors influencing success from 20-year review in an institute. Am J Otolaryngol 2012;33:308-12. [Crossref] [PubMed]
- Llorente JL, López F, Morato M, et al. Endoscopic treatment of choanal atresia. Acta Otorrinolaringol Esp 2013;64:389-95. [Crossref] [PubMed]
- Teissier N, Kaguelidou F, Couloigner V, et al. Predictive factors for success after transnasal endoscopic treatment of choanal atresia. Arch Otolaryngol Head Neck Surg 2008;134:57-61. [Crossref] [PubMed]
- Park AH, Brockenbrough J, Stankiewicz J. Endoscopic versus traditional approaches to choanal atresia. Otolaryngol Clin North Am 2000;33:77-90. [Crossref] [PubMed]
- Hartnick CJ, Hartley BE, Lacy PD, et al. Topical mitomycin application after laryngotracheal reconstruction: a randomized, double-blind, placebo-controlled trial. Arch Otolaryngol Head Neck Surg 2001;127:1260-4. [Crossref] [PubMed]
- Prasad M, Ward RF, April MM, et al. Topical mitomycin as an adjunct to choanal atresia repair. Arch Otolaryngol Head Neck Surg 2002;128:398-400. [Crossref] [PubMed]
Cite this article as: Shute WG, Wong EH, Agar NJM, Singh NP. Unilateral choanal atresia first diagnosed in adulthood and repaired via endoscopic posterior septectomy—a case series and review of the literature. Aust J Otolaryngol 2021;4:2.




