
Staged neck dissection prior to trans-oral surgery provides a safe and effective treatment paradigm for early oropharyngeal carcinoma
Introduction
Due to the high morbidity of open surgery, definitive radiotherapy or chemoradiotherapy has largely been the mainstay of treatment for early stage oropharyngeal malignancy in recent decades (1-3). Despite obvious improvements with conformal techniques, radiotherapy still carries risk of long-term sequelae (4). Inherently, radiotherapy also has the limitation of being deliverable at curative intent dose on only a single occasion.
Comparatively, transoral robotic surgery (TORS) offers a minimally invasive and highly effective primary treatment modality that in selected patients can achieve excellent rates of oncologic control without need for adjuvant treatment. Certainly compared with traditional open surgery, TORS offers significant improvement in functional outcomes, and in patients with low volume early T-stage lesions has been shown to be similar to non-surgical treatment protocols (5). For patients with low volume primary disease, ipsilateral nodal involvement and without evidence of extracapsular extension, TORS as a single modality option has now been widely adopted transforming the management of this patient cohort (6,7).
TORS, however, is not without complication. The most common complication reported is post-operative haemorrhage with rates reported between 3–16% (8-18). Likely contributed by the reduced pharyngeal sensation and subsequent impaired airway protection, many of these bleeds require operative management even if the blood volume loss is reasonably modest. Outcomes can be catastrophic with one study reporting all post-operative deaths secondary to haemorrhage (9).
To date, studies have demonstrated mixed outcomes regarding the timing of neck dissection and vessel ligation and its impact on haemorrhage rate. Suggestions that there is a trend towards less severe post-operative haemorrhage if the supplying vessels are ligated prior to undertaking TORS intuitively make sense (19). Despite this, evidence also demonstrates that delayed neck dissection does not significantly increase the risk of catastrophic haemorrhage. Accordingly, arguments for providing a concurrent neck dissection with TORS include decreased hospital stay, and therefore possible decreased cost, one anaesthetic, one procedure and therefore quicker recovery for the patient (20). However, no clear guidelines exist and current data suggests varied practice (10).
Another consideration relevant to timing of neck dissection is the risk of pharyngocutaneous fistula formation. Although not a common complication of TORS, it has a significant potential to increase patient morbidity, risk of infection, vessel damage and delay adjuvant treatment (21). Few studies have reported rates of pharyngocutaneous fistulas but Moore et al. (22) reported up to a 4% post-operative fistula rate when looking specifically at this complication and Iseli et al. (23) reported 6.5% in a case series of 16 patients when reporting functional outcomes. Performing staged surgery could possibly decrease fistula rates.
This study aims to present a single institution experience of both concurrent and staged neck dissection with vessel ligation prior to TORS and why a staged approach has been effective in minimising rates of post-operative haemorrhage and pharyngocutaneous fistula whilst maintaining good oncological outcomes for select patients. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-55).
Aim
This retrospective case series aims to present the experience of a single institution in performing upfront neck dissection with major vessel ligation prior to TORS for early oropharyngeal squamous cell carcinoma (SCC). The primary aim is to determine whether the risk of post-operative haemorrhage and pharyngocutaneous fistula is minimized with this approach all the whilst maintaining safe oncologic outcomes and minimal surgical morbidity for select patients.
Methods
Ethics approval
Ethics approval was obtained from Gold Coast Hospital and Health District Human Research Ethics Committee (LNR/2020/QGC/57102) and all patients provided informed consent. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Data collection method
A retrospective analysis was performed on data that was prospectively collated onto a secure database between 2013 and 2019.
Patient selection
All patients underwent appropriate investigation with clinical examination, histological confirmation of OPSCC, magnetic resonance imaging (MRI) with intravenous contrast and a fluorodeoxyglucose position emission tomography CT (FDG PET-CT) including dedicated contrast-enhanced CT neck. These results were reviewed at a tertiary centre multi-disciplinary team (MDT) meeting to confirm an appropriate management plan. All patients undergoing TORS lateral oropharyngectomy with either concurrent or initial staged-neck dissection were included in the analysis. Patients who were deemed a high anaesthetic risk; on anticoagulants for significant cardiovascular comorbidities were selected for the concurrent neck dissection group so as to complete treatment in a single procedure.
Treatment and post-operative management
All procedures were carried out by one of two surgeons. During selective neck dissection, elective vessel ligation of either the ipsilateral facial artery, lingual artery or linguofacial trunk was performed. TORS lateral oropharyngectomy was performed using the da Vinci system (Intuitive Surgical Inc, Sunnyvale USA) either concurrently or as a staged second procedure within 7 to 14 days. A single neck drain was utilised in the post-operative period and removed once minimal output within a twenty-four-hour period was achieved. To minimise the impact of other possible variants on the outcome, post-operative instructions were standard. Chemical prophylaxis for venothromboembolism (VTE) was not prescribed. Ibuprofen was prescribed for analgesia in the post-operative period of both operations along with paracetamol and oxycodone or tramadol. Patients were encouraged to have a soft diet as tolerated from day 1 post-operatively. Patients were discharged after the TORS procedure once tolerating sufficient diet to meet nutritional requirements and advised to stay within 40 minutes of the hospital for 2 weeks in case of post-operative haemorrhage.
Follow-up
Histology was discussed at MDT meeting post-operatively to confirm staging and determine the need for chemotherapy or radiation. Patients were seen at one-week post-operation and then at one month. Complications such as bleeding, hospital readmission or fistula formation were assessed and recorded appropriately.
Results
Patient demographics
Sixty-six patients were recruited for the study between July 2013 and July 2019. The key demographic data is outlined in Table 1. Forty-three patients (65.2%) underwent a staged neck dissection prior to TORS resection of their primary lesion. The remainder had concurrent surgery. The average age between the two groups was similar with sixty-one for the staged procedures compared with sixty-three for the concurrent surgery.
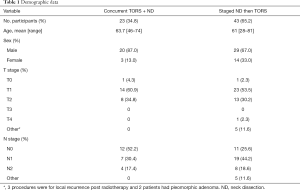
Full table
Post-operative bleeding
Overall, three patients had post-operative haemorrhages (4.5%) outlined in Table 2. Two patients in the concurrent group (8.7%) required return to theatre for control, both patients were primary cases with no concurrent anticoagulation. One patient in the staged group (2.3%) was admitted with a small less severe self-limiting post operative haemorrhage and managed conservatively.
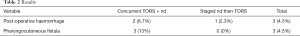
Full table
Pharyngocutaenous fistula
Of the forty-three patients that underwent the staged neck dissection prior to TORS, there were no reports of a pharyngocutaneous fistula. In the concurrent group, three patients developed a fistula (13%). These were all managed conservatively with a nasogastric tube and nil by mouth for four to five days. They all passed a contrast swallow assessment prior to recommencing oral diet and discharged with no further issues. No patients required a return to theatre for surgical repair or free flap reconstruction.
Secondary outcomes
Two patients received elective tracheostomies in the early stages of practice in case of potential bleeding and for airway protection. This practice was ceased during the study period following consensus opinion amongst treating surgeons and is no longer routine. Both patients were decannulated successfully prior to discharge. No patients in either group have required long-term supplemental feeding with any nasogastric tubes removed prior to discharge and no percutaneous endoscopic gastrotomy (PEG) tubes inserted. Average length of stay for the TORS procedure was decreased when performed without neck dissection (1.9 days) compared to those who underwent concurrent surgery (4 days) however this does not allow for the previous admission for neck dissection. There were no deaths during this case series.
Discussion
The appropriate management of the neck in patients with OPSCC can be critical for several reasons. In patients diagnosed with OPSCC the effective management of neck disease is critical to optimizing disease-specific and overall survival (24). High rates of occult metastases (approximately 10% to 40%) and imperfect non-invasive staging methods necessitate that patients with cN0 neck disease undergo elective management of the neck with either irradiation or selective neck dissection (24-26). The extent of treatment, whether referring to radiation dose or levels of lymphadenectomy, can be contended but the principle of management remains sound. That is, elective neck treatment has improved oncological outcome compared with therapeutic neck dissection for clinical N0 necks (25). The treatment modality of the neck should be guided by and correspond to the chosen treatment modality of the primary tumour (24,25).
Safe and effective surgical management is particularly important in patients with early T-stage lesions and low volume regional disease considering these patients are potentially candidates for unimodality treatment. In this highly selected subgroup, especially those who are p16/HPV-positive, safe avoidance of adjuvant treatment in over 80% can be achieved. These results rely on accurate pre-operative clinical and radiological staging, high rates of negative margins on resection of the primary lesion, and appropriate safe dissection of the involved neck disease. Avoidance of surgery-related morbidity and mortality in these instances is critical.
With these factors in mind, the current study demonstrates the accuracy of the pre-operative staging, reflected in the high concordance between clinical and pathological staging. We maintain this is paramount to avoiding unplanned adjuvant treatment. Additionally, the use of intra-operative frozen sections at the time of TORS has negated any necessity for the requirement for secondary resection. Perhaps most importantly, the approach of upfront neck dissection and concurrent selective ligation of major branches of the external carotid system has demonstrated successful avoidance of catastrophic post-operative haemorrhage and pharyngocutaneous fistula formation.
In patients undergoing radical tonsillectomy the inherent risk of encountering and placing at risk larger caliber vessels deep to the pharyngeal constrictor musculature is high (13,19,27). The dominant vessels include the facial artery and its tonsillar branches, with additional contributions from the ascending pharyngeal and lingual arteries, all branches of the external carotid artery. Access during neck dissection allows safe control of potential feeding vessels to the primary site and elective ligation can be readily performed, as necessary. This is supported by the American Society of Clinical Oncology (ASCO) clinical practice guideline published in 2019 (24).
The contrary practice of performing the neck dissection as a staged procedure following TORS has also been reported. In a large retrospective study by Frenkel et al almost 15% of cases were managed in this fashion (20). It provides the chance to take further margins on the primary site if initial pathology showed incomplete resection. As with upfront neck dissection it also limits the risk of pharyngocutaneous fistula rate as communication is avoided in the two-stage approach, though there is no ability to ligate supplying vessels which has the potential to decrease the post-operative haemorrhage severity (11-13).
A single stage procedure of concurrent neck dissection and TORS can still provide the benefit of ligating supplying oropharyngeal vessels and also has the added benefit of only requiring a single operation, anaesthetic, hospital admission and recovery time. Length of stay has been shown to be shorter for concurrent procedures and is likely more cost-effective. However, intra-operatively pharyngocutaneous communications have been reported as high as 29%, many requiring reconstruction and a post-operative fistula rate up to 14% (10).
This higher rate of pharyngocutaneous fistulas was demonstrated in our case series with all three post-operative fistulas occurring in the group undergoing concurrent surgery. Our overall rate of 4% is consistent with the limited published data. Performing the neck dissection prior to TORS allows healing of the lateral neck tissues and skin and thus minimising pharyngocutaneous communication as made evident by having zero fistulas in the staged group.
Post-operative haemorrhage is the most common post-operative complication. Published rates vary widely and most reported post-operative deaths have been attributed to post-operative bleed (9). While there has not been a significant change in the rate of bleed, the volume of loss has trended down with prophylactic ligation of the vessels as discussed above. Our study has had low numbers in both groups indicating the success of vessel ligation but notably in the group undergoing staged surgery with only one patient (2.3%) having a small self-limiting bleed. Previous studies have suggested that prior radiotherapy was an independent risk factor for post-operative haemorrhage (13). In our study three patients underwent surgical resection for recurrence post radiotherapy with a staged procedure and none resulted in a post-operative haemorrhage. Although small numbers this may suggest a safer way to approach the irradiated patient and should be strongly considered in this population.
Although this study has shown this approach to be safe and effective for this unit with the benefits as outlined above, we appreciate that patients should be treated individually on its merits and treatment adapted appropriately. Patients deemed to be at high risk of general anaesthetic or require the need to minimise time off anticoagulants have been managed with concurrent TORS and neck dissection. However, as summarised above, the neck dissection is still performed first to include a prophylactic vessel ligation. Patient preference and consent for only one procedure will also occasionally impact decision making.
This study is limited by its small observational study design and therefore statistical analysis to account for confounding variables was not performed. The data was collected retrospectively, and patient treatment was determined by the Head and Neck MDT and the decision regarding the operative approach; single verses a staged approach was not recorded and may have resulted in bias in the study results.
With respect to performing neck dissection upfront followed by staged TORS primary resection, our study demonstrates a safe and effective treatment philosophy. We also propose that this technique allows for assessment under anaesthetic of the primary lesion for surgical planning prior to definitive TORS resection.
Conclusions
This single-site case series exhibits a safe and effective approach to staged surgical treatment for early oropharyngeal SCC with a low risk of associated complications. Overall, patients undergoing both staged and concurrent neck dissection during the study period demonstrated low risk of severe post-operative haemorrhage and pharyngocutaneous fistula formation. The staged Neck dissection group presenting with one minor less sever post-operative haemorrhage managed conservatively and no pharyngocutanous fistulas. The potential economic impact of increased length of hospital stay that may result from a staged approach has not been considered in this study and maybe of interest for future study. Whilst accepting there is alternative approaches, we believe this surgical strategy offers a safe and effective management paradigm. Ultimately however the decision on timing of neck dissection should be based on the complete consideration of thorough clinical and radiological work up, surgeon preference and experience, as well as relevant individual patient factors including perioperative management and comorbidities.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-55
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-55
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-55). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from Gold Coast Hospital and Health District Human Research Ethics Committee (LNR/2020/QGC/57102) and all patients provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Denittis AS, Machtay M, Rosenthal DI, et al. Advanced oropharyngeal carcinoma treated with surgery and radiotherapy: oncologic outcome and functional assessment. Am J Otolaryngol 2001;22:329-35. [Crossref] [PubMed]
- Poulsen M, Porceddu SV, Kingsley PA, et al. Locally advanced tonsillar squamous cell carcinoma: Treatment approach revisited. Laryngoscope 2007;117:45-50. [Crossref] [PubMed]
- Pignon J-P, le Maître A, Maillard E, et al. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol 2009;92:4-14. [Crossref] [PubMed]
- Siddiqui F, Movsas B. Management of Radiation Toxicity in Head and Neck Cancers. Semin Radiat Oncol 2017;27:340-9. [Crossref] [PubMed]
- Sinclair CF, McColloch NL, Carroll WR, et al. Patient-perceived and objective functional outcomes following transoral robotic surgery for early oropharyngeal carcinoma. Arch Otolaryngol Head Neck Surg 2011;137:1112-6. [Crossref] [PubMed]
- Weinstein GS, Quon H, Newman HJ, et al. Transoral robotic surgery alone for oropharyngeal cancer: an analysis of local control. Arch Otolaryngol Head Neck Surg 2012;138:628-34. [Crossref] [PubMed]
- Dowthwaite S, Panizza B, O’Neill J, et al. Outcomes of primary trans-oral surgical management of early tonsillar squamous cell carcinoma with risk-adapted adjuvant radiotherapy. Aust J Otolaryngol 2019;2:7. [Crossref]
- Asher SA, White HN, Kejner AE, et al. Hemorrhage after transoral robotic-assisted surgery. Otolaryngol Head Neck Surg 2013;149:112-7. [Crossref] [PubMed]
- Chia SH, Gross ND, Richmon JD. Surgeon experience and complications with Transoral Robotic Surgery (TORS). Otolaryngol Head Neck Surg 2013;149:885-92. [Crossref] [PubMed]
- Frenkel CH, Yang J, Zhang M, et al. Compared Outcomes of Concurrent versus Staged Transoral Robotic Surgery with Neck Dissection. Otolaryngol Head Neck Surg 2017;157:791-7. [Crossref] [PubMed]
- Gleysteen J, Troob S, Light T, et al. The impact of prophylactic external carotid artery ligation on postoperative bleeding after transoral robotic surgery (TORS) for oropharyngeal squamous cell carcinoma. Oral Oncol 2017;70:1-6. [Crossref] [PubMed]
- Hay A, Migliacci J, Karassawa Zanoni D, et al. Haemorrhage following transoral robotic surgery. Clin Otolaryngol 2018;43:638-44. [Crossref] [PubMed]
- Kubik M, Mandal R, Albergotti W, et al. Effect of transcervical arterial ligation on the severity of postoperative hemorrhage after transoral robotic surgery. Head Neck 2017;39:1510-5. [Crossref] [PubMed]
- Mandal R, Duvvuri U, Ferris RL, et al. Analysis of post-transoral robotic-assisted surgery hemorrhage: Frequency, outcomes, and prevention. Head Neck 2016;38:E776-82. [Crossref] [PubMed]
- Repanos C, Mirza AH, George M, et al. Timing of neck dissection in association with transoral surgery: A systematic review. Head Neck 2017;39:1020-32. [Crossref] [PubMed]
- Rubek N, Channir HI, Charabi BW, et al. Primary transoral robotic surgery with concurrent neck dissection for early stage oropharyngeal squamous cell carcinoma implemented at a Danish head and neck cancer center: a phase II trial on feasibility and tumour margin status. Eur Arch Otorhinolaryngol 2017;274:2229-37. [Crossref] [PubMed]
- Topf MC, Vo A, Tassone P, et al. Unplanned readmission following transoral robotic surgery. Oral Oncol 2017;75:127-32. [Crossref] [PubMed]
- Zenga J, Suko J, Kallogjeri D, et al. Postoperative hemorrhage and hospital revisit after transoral robotic surgery. Laryngoscope 2017;127:2287-92. [Crossref] [PubMed]
- Pollei TR, Hinni ML, Moore EJ, et al. Analysis of postoperative bleeding and risk factors in transoral surgery of the oropharynx. JAMA Otolaryngol Head Neck Surg 2013;139:1212-8. [Crossref] [PubMed]
- Frenkel CH, Yang J, Zhang M, et al. Trends and the utilization of transoral robotic surgery with neck dissection in New York State. Laryngoscope 2017;127:1571-6. [Crossref] [PubMed]
- Cavalot AL, Gervasio CF, Nazionale G, et al. Pharyngocutaneous fistula as a complication of total laryngectomy: review of the literature and analysis of case records. Otolaryngol Head Neck Surg 2000;123:587-92. [Crossref] [PubMed]
- Moore EJ, Olsen KD, Martin EJ. Concurrent neck dissection and transoral robotic surgery. Laryngoscope 2011;121:541-4. [Crossref] [PubMed]
- Iseli TA, Kulbersh BD, Iseli CE, et al. Functional outcomes after transoral robotic surgery for head and neck cancer. Otolaryngol Head Neck Surg 2009;141:166-71. [Crossref] [PubMed]
- Koyfman SA, Ismaila N, Crook D, et al. Management of the Neck in Squamous Cell Carcinoma of the Oral Cavity and Oropharynx: ASCO Clinical Practice Guideline. J Clin Oncol 2019;37:1753-74. [Crossref] [PubMed]
- Jouhi L, Atula T, Mäkitie A, et al. Management of clinically N0 neck in oropharyngeal carcinoma. Eur Arch Otorhinolaryngol 2019;276:1205-10. [Crossref] [PubMed]
- Van Abel KM, Moore EJ. Focus issue: neck dissection for oropharyngeal squamous cell carcinoma. ISRN Surg 2012;2012:547017 [Crossref] [PubMed]
- Yarlagadda BB, Grillone GA. Anatomic Considerations in Transoral Robotic Surgery. In: Grillone GA, Jalisi S. editors. Robotic Surgery of the Head and Neck: A Comprehensive Guide. New York, NY: Springer New York, 2015:13-27.
Cite this article as: Cooper LN, Crouch S, O’Neill J, Dowthwaite S. Staged neck dissection prior to trans-oral surgery provides a safe and effective treatment paradigm for early oropharyngeal carcinoma. Aust J Otolaryngol 2021;4:11.


