Airway complications in a retrospective audit of 1,142 tonsillectomies: further evidence for safety of the laryngeal mask airway
Introduction
Tonsillectomy is a commonly performed surgical procedure in both children and adults. Because airway access is shared by anaesthetist and surgeon, and because airway soiling with blood and other debris can occur, it presents unique risks for complications related to the airway and respiration throughout the peri-operative period. Controversy exists over how to best manage the airway during a tonsillectomy (1,2), with particular theoretical benefits attributable to both endotracheal intubation and use of the laryngeal mask airway (LMA) (3).
Both of these airway management methods have advantages and disadvantages. Endotracheal intubation may be more likely to cause airway irritation, leading to a greater risk of coughing, gagging, laryngospasm and stridor, although there are conflicting data on this outcome (4-7). On the other hand, the LMA provides less airway protection against aspiration, with blood and possibly gastric contents more likely to be aspirated, causing laryngospasm, airway obstruction or pneumonia.
Regular use of the LMA is common, with some institutions describing its use in >90% of cases (8). Airway management for tonsillectomy obviously depends on a range of patient factors, as well as anaesthetist and surgeon preference, however LMAs are widely used in our hospital. This study was conceived in an effort to enumerate the use of particular airway types, and the risk of airway complications, amongst patients in our hospital undergoing tonsillectomy.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-77).
Methods
Albury Wodonga Health (AWH) is a regional referral hospital on the New South Wales-Victoria border that serves a population of around 250,000. A comprehensive range of surgical services are offered by AWH, including an ear, nose and throat (ENT) surgery service that performs around 350 tonsillectomies per year.
The aim of this research was to establish the rate of use of particular airway types during tonsillectomies, and to examine the rate of airway and respiratory complications in this cohort of patients. A key question was the rate of LMA failure where LMA failure was defined as a requirement for the anaesthetist to abandon the LMA in favour of endotracheal intubation for any reason.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived. Following ethics committee approval (Albury Wodonga Human Research Ethics Committee, reference number LNR57-2-2018), a convenience sample of all patients who had undergone tonsillectomy at the Albury campus of AWH from 2014–2017 were identified retrospectively from coding data collated by the Health Information Department. Patients who underwent additional procedures with tonsillectomy (e.g., adenoidectomy, myringotomy) were included, although patients undergoing adenoidectomy alone or more extensive pharyngeal or head and neck surgery (e.g., uvulopalatopharyngoplasty, tonsillectomy with neck dissection) were excluded. Medical records were examined in detail to establish demographic and clinical data including indication for surgery, selected co-morbidities, anaesthesia data and clinical events in the post-anaesthesia care unit (PACU) and ward.
Tonsillectomy was performed predominantly by two surgeons using dissection and/or cautery. Occasional locum surgeons’ cases were included. AWH also has an ENT registrar who regularly performs tonsillectomy under supervision. Surgeon identity and technique were not specifically collated as variables, although all surgeons used a Boyle-Davis gag.
Anaesthesia was provided by a core group of eight regular ENT anaesthetists, although cover by other anaesthetists does occur; identities of specific anaesthetists were not collected.
Data collected included subjects’ age, sex, weight, height, indication for tonsillectomy, history of obstructive sleep apnoea or snoring, intercurrent respiratory infection at the time of surgery, anaesthesia data including premedication, induction and maintenance techniques, opioids used in theatre and PACU, use of adjunctive drugs during anaesthesia (e.g., steroids, α2-agonists, non-steroidal anti-inflammatories), location and staff responsible for airway removal, length of hospital stay, and complications.
Specific complications were LMA failure with endotracheal tube (ETT) insertion, laryngospasm, bronchospasm, coughing intra- or post-operatively, post-operative apnoea, oxygen desaturation (<95% for >1 min) intra-operatively, in PACU or on the post-operative ward, stridor, or need for anaesthetist intervention in PACU or on the ward. Missing data were recorded as such. It was appreciated that recording of complications may have been incomplete in some cases, with a small risk of introducing bias. Data were collected from available information and individual patients or practitioners were not contacted to clarify any missing information.
Descriptive statistics were used for demographic variables. Logistic regression was used to establish odds ratios for the relationship between selected variables and the risk of LMA failure or of any complication. Statistical analyses were performed using Stata version 16 (StataCorp, College Station, Texas, USA). Graphs were created in Microsoft Excel 2013.
Results
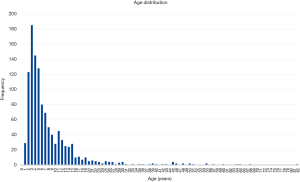
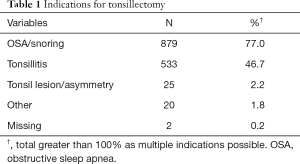
Over the four years of the study, tonsillectomy was performed in 1,142 subjects. Ages ranged from 1–82 years [median (IQR), 5 years (3–10 years)] (Figure 1) and 50.9% of subjects were female. Indications for tonsillectomy are given in Table 1. The major indications were obstructive sleep apnoea/upper airway obstruction/snoring [n=568 (49.7%)], recurrent tonsillitis [219 (19.2%)], or both of these [308 (27.0%)]. ASA physical status was 1 for 71.2% of the cohort, 2 for 28.0% and 3 for 0.8%.
Full table
Premedication was administered to 82.7% (n=945) of subjects, predominantly paracetamol alone 75.7% (n=865), with the others comprising various combinations of paracetamol, midazolam, ranitidine, pregabalin and salbutamol. Anaesthesia induction was inhalational for 869 (76.1%) subjects. Maintenance of anaesthesia was inhalational for 1,106 (96.8%) of subjects. Mean procedure duration was 46 minutes. Airways were removed in PACU in around two-thirds of cases (n=752, 65.8%) and theatre in the other one third (n=365, 32.0%). Length of stay was one night in 96.8% of cases.
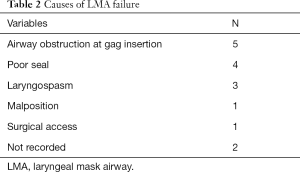
In 1,090 cases (95.4%), a reinforced LMA was utilised without recorded difficulty or complication. In thirty-one cases (2.7%), the primary airway was an ETT and in 16 (1.4%) a LMA failed and required replacement with an ETT. The predominant cause of LMA failure was airway obstruction at the time of insertion of the Boyle-Davis gag (Table 2).
Full table
In addition to LMA failure, other airway and respiratory complications for which data were collected are outlined in Table 3. The vast majority of patients had no recorded complications (982, 86.0%).
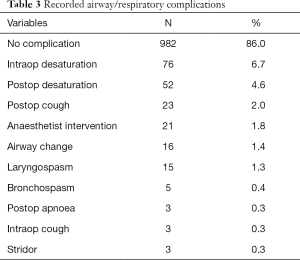
Full table
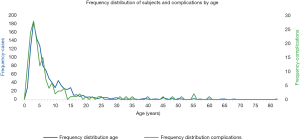
The age profile of subjects with any complication was similar to those without complications. The cohort with any complication had mean age 8.0 years, median (IQR) 4 years (3–8 years). The cohort with no complications had mean age 8.0 years, median (IQR) 5 years (3–10 years). As can be seen in Figure 2, the profile of the number of subjects with complications by age parallels the frequency distribution of subjects by age. This is consistent with the logistic regression findings (see below).
Procedure duration was longer when an ETT was used primarily (mean 57.9 min), or when an LMA required conversion to an ETT (mean 55.9 min), than if an LMA had been used primarily (mean 45.5 min).
In the 1,106 subjects in whom a LMA was the initially selected airway, a complication occurred in 152 (13.7%), including the 16 in whom the LMA was replaced by an ETT. In the 31 subjects in whom an ETT was the initially selected airway, a complication occurred in 8 (25.8%), giving a crude odds ratio for complications in the ETT group of 2.18.
Cases of laryngospasm were examined in some detail and were found to have occurred in both the operating theatre (9 cases) and the PACU (6 cases). Management of laryngospasm consisted of face mask/positive pressure ventilation (6 cases), muscle relaxant administration (5 cases), endotracheal intubation (4 cases) and propofol (3 cases). One further case was noted in which surgery was abandoned after an episode of laryngospasm on induction that was treated with propofol. This case was not specifically identified in our cohort as tonsillectomy was not performed.
Logistic regression revealed that intercurrent respiratory tract infection increased the odds of any complication (Table 4). Other variables such as age, sex, history of snoring, presence of obstructive sleep apnoea and type of airway used had no effect on the odds of a complication.
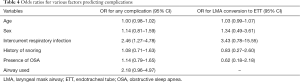
Full table
Conclusions
This series represents a large cohort of subjects undergoing tonsillectomy in whom a LMA has been satisfactorily used in the vast majority. The incidence of conversion from LMA to ETT is comparable to, and in many cases lower than, rates reported by other authors. Higher rates were reported by Lalwani et al. (9), who conducted a similar retrospective study to ours in children undergoing adenoidectomy or adenotonsillectomy. Their LMA failure rate was 6.8%, although they did include subjects undergoing adenoidectomy alone, and this was associated with a lower odds of LMA failure, suggesting that the rate of LMA failure in tonsillectomy patients is likely to have been higher again. Gravningsbråten et al. reported a prospective series of 1,126 children undergoing tonsillectomy or adenoidectomy with a LMA (10). In their tonsillectomy cohort, LMA abandonment in favour of an ETT occurred in 4 out of 589 cases (0.7%).
Several small randomised controlled trials comparing LMA and ETT in the setting of tonsillectomy (and in some studies adenoidectomy as well) have been performed, comparing a variety of outcomes including LMA failure and a range of airway complications (4-7,11-13). The range of LMA failure requiring intubation reported in the LMA groups of these trials varies from 0% to 20%. Reasons for LMA failure cited in these studies include various types of mechanical problems with positioning of the LMA (unable to place correctly, tube kinking, gas leak around the mask), laryngospasm, bronchospasm, aspiration and inadequate surgical access. The importance of sufficient depth of anaesthesia when the tonsil gag is placed and opened has been stressed (14); we did not assess depth of anaesthesia specifically in our cohort.
Complications other than LMA failure have been described in previous studies, and many have found similar rates to ours. Amongst 140 children undergoing routine ENT procedures, Parry et al. found an incidence of laryngospasm of 2.5% and coughing of 5% (15). Lalwani et al. (9), in contrast to our findings, noted an increase in overall complications in their LMA group over their ETT group.
Cooperation between surgeon and anaesthetist is paramount in ensuring the success of LMA use in the setting of tonsillectomy. The anaesthetist must be aware of critical times for LMA failure, such as gag placement, and the surgeon must be comfortable with the altered access that a LMA offers. These issues have been discussed in the literature and letters to the editor at some length (7,16-19). Younger age may be a factor affecting the incidence of airway complications with LMA use (20).
Strengths of our study include the cohort size, the consistency of the clinical care environment (a small number of surgeons and anaesthetists) and the small number of missing data.
The retrospective nature of our data collection is an important limitation. Potential problems with identification of cases and absence of information if not recorded accurately in the medical record, particularly of minor clinical events such as brief episodes of stridor or desaturation, may clearly have influenced our results. We included all patients from our hospital that had had tonsillectomy over the four-year timeframe of the study so that our sample was representative of our population of patients. Selection bias could have influenced the fact that the odds of a complication were higher in the group receiving an ETT primarily, compared to those receiving an LMA. Higher risk patients may well have been intubated for reasons that contributed to this difference (e.g., regurgitation risk). It is interesting to note that regurgitation and aspiration were not recorded in our cohort at all. It is possible that these events did not occur, that high-risk patients were pre-selected for intubation, or that documentation of minor degrees of these phenomena was incomplete. The generalisability of our findings are dependent on the preferences of surgeons and anaesthetists but with appropriate patient selection and careful communication we believe our results could be reproduced in other units.
We believe that our data contribute to the body of evidence confirming the safety of the LMA in the setting of tonsillectomy. Whilst a number of authors have reported frequent use of the LMA for tonsillectomy in particular centres (7,18), a French survey of airway management for tonsillectomy revealed infrequent use in this setting (2%) (21), whilst a survey of British anaesthetists in 2007 revealed a greater than 70% use of ETT for airway management during tonsillectomy in all age groups, and 87% in the <3-year age group (22). An earlier British survey showed a similar low routine rate of use of the LMA (16%) (23). Nevertheless, a more recent literature review has suggested the LMA as an equivalent first-line airway to the ETT (24). We believe our findings confirm the use of the LMA as a practical and safe technique in tonsillectomy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-77
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-77
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-77). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Albury Wodonga Human Research Ethics Committee (reference number LNR57-2-2018) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mandel JE. Laryngeal mask airways in ear, nose, and throat procedures. Anesthesiol Clin 2010;28:469-83. [Crossref] [PubMed]
- Raeder J. Ambulatory anesthesia aspects for tonsillectomy and abrasion in children. Curr Opin Anaesthesiol 2011;24:620-6. [Crossref] [PubMed]
- Ravi R, Howell T. Anaesthesia for paediatric ear, nose, and throat surgery. Contin Educ Anaesth Crit Care Pain 2007;7:33-7. [Crossref]
- Doksrød S, Løfgren B, Nordhammer A, et al. Reinforced laryngeal mask airway compared with endotracheal tube for adenotonsillectomies. Eur J Anaesthesiol 2010;27:941-6. [Crossref] [PubMed]
- Peng A, Dodson K, Thacker L, et al. Use of laryngeal mask airway in pediatric adenotonsillectomy. Arch Otolaryngol Head Neck Surg 2011;137:42-6. [Crossref] [PubMed]
- Sierpina DI, Chaudhary H, Walner D, et al. Laryngeal mask airway versus endotracheal tube in pediatric adenotonsillectomy. Laryngoscope 2012;122:429-35. [Crossref] [PubMed]
- Webster AC, Morley-Foster P, Dain S, et al. Anaesthesia for adenotonsillectomy: a comparison between tracheal intubation and the armoured laryngeal mask airway. Can J Anaesth 1993;40:1171-7. [Crossref] [PubMed]
- Hamilton MA, Patel A. Laryngeal mask airway and tonsillectomy: a question of training. Anesth Analg 2007;104:1312-3. [Crossref] [PubMed]
- Lalwani K, Richins S, Aliason I, et al. The laryngeal mask airway for pediatric adenotonsillectomy: predictors of failure and complications. Int J Pediatr Otorhinolaryngol 2013;77:25-8. [Crossref] [PubMed]
- Gravningsbråten R, Nicklasson B, Raeder J. Safety of laryngeal mask airway and short-stay practice in office-based adenotonsillectomy. Acta Anaesthesiol Scand 2009;53:218-22. [Crossref] [PubMed]
- Ranieri D Jr, Neubauer A, Ranieri D, et al. The use of disposable laryngeal mask airway for adenotonsillectomies. Rev Bras Anestesiol 2012;62:788-97. [Crossref] [PubMed]
- Hern JD, Jayaraj S, Sidhu V, et al. The laryngeal mask airway in tonsillectomy: the surgeon’s perspective. Clin Otolaryngol Allied Sci 1999;24:122-5. [Crossref] [PubMed]
- Williams PJ, Bailey P. Comparison of the reinforced laryngeal mask airway and tracheal intubation for adenotonsillectomy. Br J Anaesth 1993;70:30-3. [Crossref] [PubMed]
- Xue FS, Li T, Liao X. Safe use of a laryngeal mask airway in children undergoing a tonsillectomy. Acta Anaesthesiol Scand 2009;53:684-5. [Crossref] [PubMed]
- Parry M, Glaisyer H, Bailey P. Removal of LMA in children. Br J Anaesth 1997;78:337-8. [Crossref] [PubMed]
- Heath ML, Sinnathamby S. The reinforced laryngeal mask airway for adenotonsillectomy. Br J Anaesth 1994;72:728-9. [Crossref] [PubMed]
- Howard-Griffin RM, Driver I. Laryngeal mask airway in adeno-tonsillectomy in children. Anaesthesia 1996;51:409. [Crossref] [PubMed]
- Presland AH, Evans A, Bailey P, et al. Letter to the editor. Clin Otolaryngol Allied Sci 2000;25:240. [Crossref] [PubMed]
- Erkan AN. The use of laryngeal mask airway in tonsillectomies. Braz J Anesthesiol 2014;64:71. [Crossref] [PubMed]
- Wilson MN, Long L, Ved S, et al. Younger pediatric adenotonsillar surgical patients exhibit more complications at mouth gag insertion with LMA use. Int J Pediatr Otorhinolaryngol 2009;73:1173. [Crossref] [PubMed]
- Ecoffey C, Auroy Y, Pequignot F, et al. A French survey of paediatric airway management use in tonsillectomy and appendicectomy. Paediatr Anaesth 2003;13:584-8. [Crossref] [PubMed]
- Clarke MB, Forster P, Cook T. Airway management for tonsillectomy: a national survey of UK practice. Br J Anaesth 2007;99:425-8. [Crossref] [PubMed]
- Hatcher IS, Stack C. Postal survey of the anaesthetic techniques used for paediatric tonsillectomy surgery. Paediatr Anaesth 1999;9:311-5. [Crossref] [PubMed]
- Costar EJ, Same M. Laryngeal mask airway or endotracheal tube for tonsillectomy? An update. Br J Hosp Med (Lond) 2017;78:418. [Crossref] [PubMed]
Cite this article as: McFarland DM, Tweddle EA, Baitch L. Airway complications in a retrospective audit of 1,142 tonsillectomies: further evidence for safety of the laryngeal mask airway. Aust J Otolaryngol 2021;4:10.