
A retrospective cohort study on false positive diffusion weighted MRI in the detection of cholesteatoma
Introduction
Cholesteatoma is a common inflammatory middle ear process characterised by trapped keratinous debris within a squamous epithelial sac exhibiting autonomous growth and bony erosion. Management of cholesteatoma is almost always surgical unless a patient is not considered fit for surgery. A variety of surgical procedures have been described for this condition, but typically the options for disease involving the Prussak’s space include canal-wall up mastoidectomy or canal-wall down (modified radical) mastoidectomy with the latter often reserved for more extensive disease in sclerotic mastoids or where there is labyrinthine involvement or complications. While morbidity is minimised by canal wall-up mastoidectomy techniques in preserving the bony external auditory canal and avoiding the creation of a mastoid cavity, residual disease rates of approximately 35% and recurrence rates around 18% have been quoted necessitating a second-look procedure (1). Due to the presence of an intact canal wall, the clinical detection of recurrence also becomes difficult.
In recent years, the utilisation diffusion-weighted imaging (DWI) on magnetic resonance imaging (MRI) has been utilised as a non-invasive method to detect cholesteatoma (2). With advent of non-echoplanar sequences, the accuracy of DWI in detecting cholesteatoma has been further increased. In addition, DWI avoids the necessity for intravenous contrast and has shorter procedural times (2).
Given its utility in detecting cholesteatoma non-invasively, DWI has been proposed as an alternative to second look surgery. This has been supported by a recent meta-analysis showing that the sensitivity and specificity of DWI in detecting residual and recurrent disease to be 90% and 95% respectively, with some studies quoting up to 99% sensitivity (3). The effectiveness of DWI in detecting residual/recurrent disease has the potential to reduce the requirement for second look surgery and its associated operative risks. The presence of a positive DWI scan also means surgical exploration is usually prompted unless the decision is made to observe for growth of a potential focus of cholesteatoma. Studies have shown that to detect cholesteatoma by DWI MRI the disease needs to be 3 mm or greater in size, (2) which means many scans may have a false negative result if the disease is not large enough to be picked up on imaging.
Conversely, false positive DWI patients have been rarely reported in the literature to date.
This study presents a retrospective review of the 11 patients with false positive DWI and a review of the current literature on false positive DWI MRI for detection of cholesteatoma.
We present the following article in accordance with the TREND reporting checklist (a vailable at http://dx.doi.org/10.21037/ajo-20-57).
Methods
The cases were consecutively identified in the course of a tertiary otology centre as part of routine clinical practice over the research period (years 2016 to 2019). Patients were only included in this series if they had a positive DWI and an operative decision was made to undergo surgery during which cholesteatoma was not identified both intraoperatively and histopathologically.
MRI scanning was reported by fellowship trained head and neck radiologists. The imaging findings documented included the type of MRI scan used, DWI sequence, location of the diffusion restriction, size and the Computed tomography (CT) scan findings.
A thorough retrospective evaluation of the medical records was undertaken including review of the operative notes, radiological findings and histopathology. In all patients the following specific information was obtained: age, sex, presenting otological symptoms and otological operative history. The specific symptoms assessed were the presence of otalgia, otorrhoea, imbalance, tinnitus and hearing loss. The otological examination findings assessed were the presence of a tympanic membrane perforation, retraction, discharging ear, tympanosclerosis and abnormal vestibular examination. The audiogram prior to surgery was recorded to assess the air and bone conduction thresholds as well the air-bone gap.
The operative findings assessed included the macroscopic presence or absence of cholesteatoma, the status of the ossicular chain, the status of the tympanic membrane and status of the middle ear mucosa.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the South Metro Health Service Ethics committee human research committee. A waver of consent was approved for this project.
Results
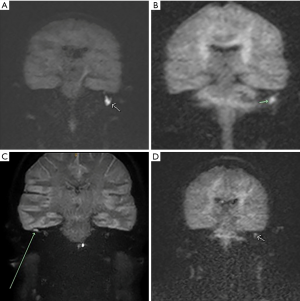
A total of 11 patients (5 males and 6 females) were included as having false positive DWI MRI for cholesteatoma (four examples noted in Figure 1. 5 males and 6 females. The mean age of the patients was 53 years with an age range from 6 years to 82 years of age. Three patients had no symptoms related to the ear and were therefore classed as clinically asymptomatic. The remaining 8 patients (73%) had varying symptoms including otalgia, otorrhoea, hearing loss, tinnitus and imbalance. 9 of the 11 patients had had previous otological surgery. 3 patients had predominantly sensorineural hearing loss (SNHL), the rest having either conductive hearing loss or a mixed hearing loss pattern (https://cdn.amegroups.cn/static/public/ajo-20-57-1.pdf).
In 7 cases (64%) it was felt that the positive DWI MRI was the key feature which triggered the decision to operate. In the remainder (36%) a combination of the patient’s clinical picture and CT findings (such as ossicular erosion, opacification or scutal erosion) contributed to the decision for middle ear exploration. In all cases, cholesteatoma was not positively identified clinically prior to surgery and the DWI MRI scan was requested in order to exclude cholesteatoma.
Where the diffusion abnormality was able to be measured (in 10 out of 11 patients) the mean focus of diffusion abnormality was 10.3 mm (range from 3 to 30 mm). Diffusion restrictions were noted to be in the epitympanum in 6 patients (54%). Four patients had diffusion restriction in the mastoid and 1 patient in the mesotympanum. Five patients were scanned using 1.5 Tesla and 6 were scanned using 3 Tesla strength MRI scanner. Non Echo-planar technique was used on all patients. Within the group who were scanned with 1.5 T, the size of the DWI lesion was on average larger (mean 11.5 mm, range 5–30 mm, n=5) than the patients with 3T (mean 9.1 mm, range 3–20 mm, n=5, patient 6 excluded due to punctate size lesions), however this was not statistically significant (t-value 0.43, P-value 0.33). There was no specific pattern of pathology when these two groups were compared. CT was performed on 8 of 11 patients and in 5 of these patients, there was opacification on the CT corresponding to the location of diffusion restriction seen on MRI (https://cdn.amegroups.cn/static/public/ajo-20-57-1.pdf).
The histopathological findings in 6 cases (2 cases of chronic inflammation, and one case each of non-specific inflammatory tissue, granulation tissue with fibrosis, middle ear mucosal adhesions and ceruminous impaction) were benign. In these cases, it could be argued that their surgery in these 6 cases (55%) was unnecessary. In the remaining 5 cases (one case of ceruminous adenoma and 4 cases of cholesterol granuloma), whilst the surgery did not find cholesteatoma, removal of a middle ear adenoma and cholesterol granuloma was arguably still indicated (https://cdn.amegroups.cn/static/public/ajo-20-57-1.pdf).
An evaluation of the patients identified from the literature review identified additional aetiology not included in our cohort which produced a false positive DWI MRI signal including the presence of a silastic sheet, thick tympanosclerosis, bone graft material and motion artefact on MRI (https://cdn.amegroups.cn/static/public/ajo-20-57-2.pdf).
Discussion
The utilisation of canal wall up versus wall down approaches in the management of primary cholesteatoma is a long-standing debate in otological practice. It is anticipated with increasing familiarity and training, in coming years endoscopic management will continue to play an increasing role in management. While the primary surgical aim in the treatment of cholesteatoma is the creation of a safe, dry and disease-free ear, the morbidity, especially in younger, more active patients of a more radical canal wall down procedure can be limiting. This can be partly overcome by techniques such as reconstruction of the canal wall and mastoid cavity obliteration. The canal wall-up procedure in comparison allows for preservation of anatomical structures, improves postoperative drainage thereby reducing the need for routine cavity toileting and does not limit recreational water exposure. The major disadvantage these techniques is the clinical detection of residual or recurrent cholesteatoma. The presence of the posterior canal wall limits visualisation of crucial areas and therefore the canal wall down approach provides improves microscopic view to clear disease from the anterior epitympanum and supratubal recess. One meta-analysis demonstrated the relative risk of recurrence in CWU vs CWD surgery to be 2.87 Jeny(4). While most of the data included in this review was non-randomised, it does highlight the limitation of CWU surgery. Traditional practice therefore in this setting was to perform a routine “second-look” procedure after at least 6 months to reassess the presence of residual disease.
CT imaging, widely utilised for preoperative planning in the setting of initial mastoidectomy for cholesteatoma, performs poorly in the setting of recurrent cholesteatoma. Tierney and colleagues found the sensitivity (42.9%), specificity (48.3%) and positive predictive value (28.6%) for CT in the detection of residual or recurrent cholesteatoma to be poor (5). The difficulty in using CT for this purpose is ascribed to the difficulty in discriminating residual or recurrent disease from granulation tissue, scar tissue or trapped fluid on this modality.
Magnetic resonance imaging relies on the interaction between protons in tissue in an electromagnetic field. Diffusion weighted imaging sequences specifically looks at the interactions of protons to opposing magnetic field gradients. The two main types of DWI are echoplanar (EPI) and non-echo-planar imaging (non-EPI). Non-EPI is typically used in assessing cholesteatoma as it utilises thinner slices and minimises artefact and distortion (2).
Although a baseline T2 sequence is required to create and interpreter a DWI sequence, the provision of additional MRI sequences does not appear to increase the sensitivity in detecting cholesteatoma, thereby reducing MRI procedural times and obviating the requirement for intravenous contrast. De Foer et al found the sensitivity of gadolinium-enhanced T1 to be 56.7% and that of Non-EPI DWI to be 82.6% in detecting cholesteatoma. The addition of the T1 sequence only improved the combined sensitivity marginally to 84.2% (6).
In recent years there has been a considerable interest in DWI in reducing the amount of negative second-look procedures for evaluation of recurrent cholesteatoma. A recent meta-analysis on the topic reviewed 1,152 patients across 26 studies including patients with histopathologically confirmed cholesteatoma (7). The study found that the overall sensitivity and specificity of DWI in detecting cholesteatoma was 91% (95% CI: 87–95%) and 92% (95% CI: 86–96%) respectively. On subgroup analysis the respective values for recurrent cholesteatoma were found to be 93% (95% CI: 84–97%) and 91% (95% CI: 85–94%). The high sensitivity and specificity found in this study lends support to the practice of replacing second look surgery with serial DWI MRI follow-up.
To identify potential aetiologies for false positive DWI MRI not included in our cohort, a review of the literature was performed to determine the number of reported patients with a positive DWI study who underwent surgical exploration and who had histopathology which was not cholesteatoma. A PubMed search using the terms “False positive and MRI and Cholesteatoma” was undertaken. Of the 28 articles reviewed 6 papers with a total of 9 patients met our inclusion criteria and the findings summarised in https://cdn.amegroups.cn/static/public/ajo-20-57-2.pdf and therefore our cohort represents the largest case series of patients in the literature to date.
The aetiologies reported include bone graft used to seal the lateral semicircular canal during initial surgery (8), Otis media was found in two patients (9,10), scar tissue in the mastoid cavity (9), Silastic sheet (11), cholesterol granuloma (12), tympanosclerosis (13), motion artefact and granulation tissue (14). Some studies reported cases were no abnormality was identified at this site of positive DWI (15).
A common feature in our patients was the fact that the clinical examination findings in all patients were not typical for cholesteatoma. It could be argued that if cholesteatoma was identified on clinical examination preoperatively, an MRI scan may not have been required. Our study suggests that in the absence of clinical features of obvious cholesteatoma, one should be prepared for the presence of a false positive finding of the MRI if it was requested to exclude cholesteatoma when there is a reasonable cause to find one but could not be completely excluded clinically. However, the absence of clinical features of cholesteatoma does not of course, suggest that most cases of cholesteatoma may not be present as clinically occult disease is well known to occur. In our study, DWI MRI scans were not performed for no apparent reason or without reasonable justification and therefore, indiscriminate DWI MRI scan requesting does not seem to be the sole reason for the presence of false positive scans. However, more widespread adoption of DWI MRI scans has led this to be an alternative to either watchful waiting or exploratory surgery which would have been the default alternative for our cohort of patients.
One of the criticisms of DWI MRI is the limited ability to detect cholesteatoma under 3 mm in diameter. However, in our series, the mean size of the diffusion abnormality was much higher than this at 8.6 mm. This suggests that size of the abnormality alone does not exclude a false positive diagnosis.
In our study we identified several pathological processes showing DWI signal during MRI examination. These included ceruminous adenoma, cholesterol granuloma, non specific inflammation, ceruminous impaction and granulation tissue with fibrosis. Cholesterol granuloma was the most common non-benign finding. Previous otological surgery appears to be a specific risk factor for false positive DWI MRI with 9 of 11 of the patients presented having had previous surgery. Whilst the detection of cholesteatoma is the main purpose of the DWI MRI, the detection of cholesterol granuloma which can lead to chronic ear pathology, suggests that the one should still perform MRI scans in these patients. Perhaps future refinements of the DWI MRI sequence should be focussed on being able to distinguish between cholesterol granuloma and non-specific inflammatory tissue.
This study was limited by the fact that we did not examine all patients who had undergone a DWI MRI study during the study period and neither did we examine the number of true positive DWI MRI cases. This means that we were unable to define a false positive rate for DWI MRI studies in our cohort of patients. In addition, we did not examine those patients who had a positive DWI study but did not undergo surgery because of patient preference or because the surgeon decided to monitor the patient due to a perceived false positivity from a lack of clinical features suggesting cholesteatoma. We also did not arrange MRI scans for those patients who routinely undergo 2nd look surgery following cholesteatoma and who were subsequent found to not have cholesteatoma. Future studies which can capture all positive DWI cases may be required to obtain a more accurate false positive DWI MRI scan rate.
DWI MRI has a high positive predictive value for cholesteatoma and is therefore used in both primary detection of cholesteatoma and when there is diagnostic uncertainty and for follow up after cholesteatoma surgery. Given the possibility of false positive DWI MRI in either setting, we conclude that DWI MRI should be used in conjunction with the patient’s clinical picture and other radiological findings, including CT findings, when making the decision for middle ear exploration. Additionally patients should be counselled on the possibility that an alternative pathological process may be present which may alter the surgical requirements and long term management and monitoring needs.
Acknowledgments
Professor Marcus Atlas for contribution to patient identification.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-57
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-57
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-57). Dr. JK serves as an unpaid editorial board member of the Australian Journal of Otolaryngology from Jan 2019 to Dec 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the South Metro Health Service Ethics committee human research committee. A waver of consent was approved for this project.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kerckhoffs KG, Kommer MB, van Strien TH, et al. The disease recurrence rate after the canal wall up or canal wall down technique in adults. Laryngoscope 2016;126:980-7. [Crossref] [PubMed]
- Henninger B, Kremser C. Diffusion weighted imaging for the detection and evaluation of cholesteatoma. World J Radiol 2017;9:217-22. [Crossref] [PubMed]
- Muzaffar J, Metcalfe C, Colley S, et al. Diffusion-weighted magnetic resonance imaging for residual and recurrent cholesteatoma: a systematic review and meta-analysis. Clin Otolaryngol 2017;42:536-43. [Crossref] [PubMed]
- Tomlin J, Chang D, McCutcheon B, et al. Surgical technique and recurrence in cholesteatoma: a meta-analysis. Audiol Neurootol 2013;18:135-42. [Crossref] [PubMed]
- Tierney PA, Pracy P, Blaney SP, et al. An assessment of the value of the preoperative computed tomography scans prior to otoendoscopic 'second look' in intact canal wall mastoid surgery. Clin Otolaryngol Allied Sci 1999;24:274-6. [Crossref] [PubMed]
- De Foer B, Vercruysse JP, Bernaerts A, et al. Middle ear cholesteatoma: non-echo-planar diffusion-weighted MR imaging versus delayed gadolinium-enhanced T1-weighted MR imaging--value in detection. Radiology 2010;255:866-72. [Crossref] [PubMed]
- Lingam RK, Bassett P. A Meta-Analysis on the Diagnostic Performance of Non-Echoplanar Diffusion-Weighted Imaging in Detecting Middle Ear Cholesteatoma: 10 Years On. Otol Neurotol 2017;38:521-8. [Crossref] [PubMed]
- Osman NM, Rahman AA, Ali MT. The accuracy and sensitivity of diffusion-weighted magnetic resonance imaging with Apparent Diffusion Coefficients in diagnosis of recurrent cholesteatoma. Eur J Radiol Open 2017;4:27-39. [Crossref] [PubMed]
- Jeunen G, Desloovere C, Hermans R, et al. The value of magnetic resonance imaging in the diagnosis of residual or recurrent acquired cholesteatoma after canal wall-up tympanoplasty. Otol Neurotol 2008;29:16-8. [Crossref] [PubMed]
- Fitzek C, Mewes T, Fitzek S, et al. Diffusion-weighted MRI of cholesteatomas of the petrous bone. J Magn Reson Imaging 2002;15:636-41. [Crossref] [PubMed]
- Venail F, Bonafe A, Poirrier V, et al. Comparison of echo-planar diffusion-weighted imaging and delayed postcontrast T1-weighted MR imaging for the detection of residual cholesteatoma. AJNR Am J Neuroradiol 2008;29:1363-8. [Crossref] [PubMed]
- Kösling S, Bootz F CT. Eur J Radiol 2001;40:113-8. [Crossref] [PubMed]
- Evlice A, Tarkan O, Kiroglu M, et al. Detection of recurrent and primary acquired cholesteatoma with echo-planar diffusion-weighted magnetic resonance imaging. J Laryngol Otol 2012;126:670-6. [Crossref] [PubMed]
- von Kalle T, Amrhein P, Koitschev A. Non-echoplanar diffusion-weighted MRI in children and adolescents with cholesteatoma: reliability and pitfalls in comparison to middle ear surgery. Pediatr Radiol 2015;45:1031-8. [Crossref] [PubMed]
- Locketz GD, Li PM, Fischbein NJ, et al. Fusion of Computed Tomography and PROPELLER Diffusion-Weighted Magnetic Resonance Imaging for the Detection and Localization of Middle Ear Cholesteatoma. JAMA Otolaryngol Head Neck Surg 2016;142:947-53. [Crossref] [PubMed]
Cite this article as: Esmaili AA, Hasan Z, Withers SJ, Kuthubutheen J. A retrospective cohort study on false positive diffusion weighted MRI in the detection of cholesteatoma. Aust J Otolaryngol 2021;4:18.


