
A survey of Queensland medical education in otolaryngology
Introduction
Ear, nose and throat (ENT) as a specialty is historically under-represented in the medical school curriculum. Universities within Queensland have varying levels of ENT teaching and many students will never have clinical experience with an ENT service. With the recent influx of medical school students within Australian schools, the need for a more effective and appropriate medical school curriculum is paramount.
Otolaryngology presentations are common in both general practice and emergency medicine (1). ICD-10 diseases of the ear and mastoid process (H60-95) comprised 98,245 emergency department (ED) presentations across Australia in 2017–2018 (2). A 2013 study in Australian Family Physician indicated that acute otitis media (AOM) and mouth/tongue/lip disease were at the 50th and 75th diagnostic centiles for the most frequently managed problems in general practice (3). Altogether, ENT problems comprise approximately 1 in 4 adults and 1 in 2 paediatric general practice consultations (1,4).
In spite of the frequency of ENT presentations in clinical practice, medical students in the UK, US, Canada and Australia receive little teaching and clinical exposure to ENT (5-7). Studies conducted in these countries reveals that students receive little education on ENT and its scope, and have little time allocated to ENT in their clinical placements (5). It was demonstrated in the UK that the mean mandatory placement in ENT was 8 days in duration, while only 53 per cent of students had access to mandatory placements (8). Over a third of participating medical schools did not offer any ENT placement (8). Where clinical time is offered, it has marked variability (8). A survey of all 16 Canadian medical schools demonstrated that the mean duration of clinical placement in ENT was 4.6 days, with only 6 medical schools providing mandatory placements (9). Significant variability also existed between US medical schools, with 33.6 per cent of 125 medical schools having a required rotation in ENT (10).
Consequently, when surveyed, medical graduates have consistently expressed a lack of preparedness and confidence in dealing with ENT problems in clinical practice (1,6). In 2016, a survey of 111 junior doctors in the UK reported that 75 per cent “lacked confidence in their ability to manage epistaxis” (11), while only 18 per cent felt confident to perform nasal cautery (11).
Particularly in Australia, there is a paucity of recent data on undergraduate ENT education and competencies. A 2001 survey of New South Wales interns identified the management of epistaxis as the top procedural skill for which more medical school preparation was necessary (7). Examination of the ENT ranked as the second most acknowledged core practice lacking medical school preparation (7). Our search of the literature in Australia using MeSH terms ‘otolaryngology’ and ‘education’, and key terms ‘undergraduate’ and ‘exposure’ did not yield any more recent data.
We hypothesise that the ongoing trends concerning the lack of undergraduate otolaryngology medical education in other English-speaking countries remain true in Australia. This survey sought to gather recent Queensland data on undergraduate ENT education, exposure and competencies in order to identify current trends in medical education. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-87).
Methods
The study was designed as a prospective cohort study. Hospitals employing medical interns in Queensland Health were identified through the Queensland Health website. To recruit respondents, twenty-one hospitals in total were contacted through their medical education departments and paper questionnaires were handed out during regular intern teaching. These were anonymous and voluntary in order to maintain confidentiality and minimise response bias. The survey asked 21 questions regarding the individual ENT experience of the participant, both in medical school and as an intern, and utilised the Yes/No format and Likert scales (Appendix 1). The universities where interns studied medicine were identified as potential confounders and data were collected regarding the alma maters of respondents. The duration of medical school ENT teaching and time attached to a specialist ENT service were also asked of respondents. The options used in the Likert scales to measure duration were chosen to reflect common lengths of time of teaching and placement in medical schools.
Responses were collected in the second half of 2019 and first half of 2020, and the majority of responses were obtained from one cohort of interns from the 2019 intern year. A second set of responses was gathered from The Royal Brisbane & Women’s Hospital in the 2020 intern year. For the purposes of this study, we have aggregated these results. The completed surveys were either scanned and returned via email, or sent via post to the principal investigator. Survey responses were then collated and analysed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Multi-site ethics approval was obtained from Royal Brisbane and Women’s Hospital Human Research Ethics Committee (LNR/2019/QRBW/51023) and all respondents provided informed consent.
Statistical analysis
Interns’ self-reported skills in clinical examination, diagnosis and management of common conditions was compared according to the amount of ENT teaching they reported receiving, and whether or not they had an attachment to a specialist ENT service. Observational statistics were derived from survey data and statistically analysed using the 2-sample t-test (https://cdn.amegroups.cn/static/public/ajo-20-87-1.xlsx; https://cdn.amegroups.cn/static/public/ajo-20-87-2.xlsx), assuming equal variance between groups. The aggregate means of each group and P values obtained using the t-test were then compared.
Results
Results were collected over a 6-month period. Some hospitals were excluded due to difficulty contacting medical educators or attaining site specific approval within appropriate timeframes. Some hospitals declined participation. At the time of the survey, 787 interns were employed in Qld Health. Our sample size altogether comprised 106 respondents from 6 intern cohorts. Nine of the respondents were excluded from the survey as they were either medical students or residents above PGY1, leaving 97 interns who were included in the analysis (Figure 1). For questions in individual surveys that were not answered by individual respondents, the data point was excluded from the analysis.
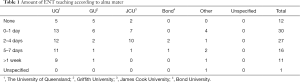
The largest group of respondents came from The Royal Brisbane & Women’s Hospital, which comprised over half of our sample (55%). Students attended various universities including University of Queensland (52%), James Cook University (20%), Griffith University (16%) and Bond University (3%).
The first group of questions was aimed at determining the amount of ENT teaching that each intern had during medical school. Interns were asked to choose from responses on Likert scales ranging from no teaching and over one week. A majority (71%) reported less than 5 days of teaching in ENT, with 12% reporting no ENT teaching at all. Of those who received more than 5 days of teaching, only 33% found the teaching useful or extremely useful.
As few as 31% of interns spent time attached to a specialist ENT service in medical school, and within this cohort the duration of placement was typically between 1–4 weeks. In comparison to ENT teaching, 80% of interns found this experience to be useful to extremely useful. There was marked variability in the amount of ENT teaching and duration of placement within individual medical schools (Tables 1 and 2).
Full table

Full table
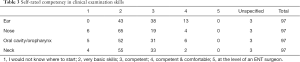
The second group of questions was aimed at establishing the participants’ perceived skillset in diagnosing and managing common ENT pathologies. The first of these questions asked participants to rate their clinical examination skills in the ear, nose, oral cavity/oropharynx and neck. In all areas, most interns only felt they had very basic skills in clinical examination (Table 3). The results demonstrated they were least confident in the examination of the nose, with 67% reporting only basic skills.
Full table
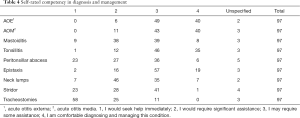
The next questions required interns to rate their ability to manage common ENT pathologies (Table 4). The conditions included acute otitis externa (AOE), AOM, tonsillitis, and more acute or life-threatening conditions such as stridor. The results were, as expected, varied according to the type of pathology. Interns felt more confident in diagnosing and managing AOE, AOM and tonsillitis with the majority rating themselves as only requiring some assistance or being comfortable in diagnosing and managing this condition. Thirty-nine per cent said they would need significant assistance with managing mastoiditis. The range of answers with regards to peritonsillar abscess was broad, with some interns seeking help immediately (24%) and some (37%) feeling they would only need some assistance. When asked regarding management of epistaxis, 78% of participants felt they would only need some assistance or felt comfortable managing this on their own. Forty-seven per cent felt they would need significant assistance with the management of neck lumps. The last two pathologies in this question set evaluated competence in the management of more serious conditions. When asked regarding the management of stridor, some participants were surprisingly comfortable, with an answer range similar to that of peritonsillar abscess. Only 24% of interns would seek help immediately when faced with a stridulous patient and 42% of interns felt they could manage this condition with only some assistance. Participants felt uncomfortable managing tracheostomies and 60% would seek immediate help to manage this.
Full table
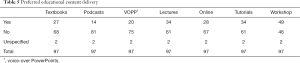
With rapidly evolving internet and medical technologies, our teaching methods must also adapt. Our secondary aim for this survey was to establish if our current methods in teaching are useful and up to date. Forty-two per cent of interns reported they did not have access to any electronic resources on ENT. Interns were then asked whether particular resources would have been of value. The most popular answer was a workshop-based day of ENT teaching, with 51% of respondents indicating they would have found this useful (Table 5). Other resources such as podcasts (84%) were not deemed useful. More traditional pedagogical methods including tutorials and lectures were still considered helpful learning resources, scoring higher than other methods.
Full table
The final group of questions was aimed at determining how much ENT teaching interns feel they should have had in medical school. Seventy per cent of respondents believed that there should be a minimum of 5 days of teaching in medical school. This is in comparison to only 28% actually having this experience during their degree.
When asked if medical students should have an attachment to an ENT service, 74% of respondents agreed they should. Of these respondents, 64% felt the time allocated should be between 4 days and 4 weeks, and within this range, an allocation of 1 to 2 weeks was the most commonly chosen response.
Interns were also asked if they felt their ENT exposure was sufficient to prepare them as a junior doctor. A high proportion (66%) answered ‘no’ to this question. Eighty-five per cent of surveyed interns agreed that ENT should be a compulsory part of the medical school curriculum.
A further question asked how much experience as an intern junior doctors should have, if any. A third recommended that they should have a 3- to 5-week rotation (Table 6). Sixty nine per cent overall recommended a minimum rotation of 1 to 3 weeks.
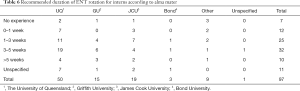
Full table
The final question in our survey asked the likelihood that respondents would pursue a career in ENT. Sixty-nine per cent reported being very unlikely or unlikely to follow this pathway.
Analysis
We compared interns’ self-reported clinical skills in Questions 11 and 12 of the survey according to the amount of ENT teaching they reported (Question 3), and whether or not they had an attachment to a specialist ENT service (Question 5). Two-sample t-testing was performed assuming equal variance between groups.
Responses from Question 3 were sorted into two groups: ‘1 week or less’ and ‘greater than 1 week’. The pooled analysis comprising all data from Question 11 (Table 7) concerning clinical examination skills demonstrated a statically significant difference between the groups, with the group receiving greater than 1 week of teaching having a higher aggregate mean score of 11.091 compared to 9.461 (P=0.017). Thus, the group receiving more teaching self-reported higher levels of competence in clinical examination broadly.
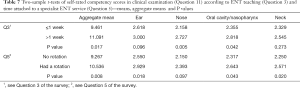
Full table
Notably however, when looking at differences in effect within individual categories of examination, not all groups were significantly different. Self-reported competence in examination of the ear (P=0.096) and neck (P=0.273) individually were not significantly different between the groups, while there was a significant increase in self-reported competence between groups for examination of the nose (P=0.005) and oral cavity/nasopharynx (P=0.042).
For self-reported competence in diagnosis and management (Question 12) no significant difference was observed between groups in the pooled analysis (Table 8). The group receiving more teaching had an aggregate mean score of 25.361 compared to 23.355 (P=0.123) for the group receiving less teaching.

Full table
When comparing the self-reported competence between groups for individual ENT diagnoses/treatments, all items with the exception of tracheostomies (P=0.025) demonstrated no significant difference.
Similarly, respondents’ answers to Question 5 were used to compare their self-reported clinical skills. Those who had a rotation attached to a specialist ENT service had a statistically significant increase in their aggregate mean score for Question 11 of 10.536 compared to 9.267 (P=0.008) for those who did not (Table 7). Therefore, the exposed group self-reported higher competence in clinical examination skills.
Individually, there was a statistically significant increase in self-reported competence for examination of the ear (P=0.018), oral cavity/nasopharynx (P=0.043), and neck (P=0.020). There was no significant difference between groups for examination of the nose (P=0.097).
There was no significant difference in aggregate mean scores between the groups for Question 12 (Table 8): those who had an ENT rotation scored 24.250 compared to 23.333 (P=0.321) for those who did not. Likewise, there was no significant difference (P>0.05) in scoring between groups concerning ENT diagnoses/treatment when these were assessed individually.
Discussion
These survey data draw our attention to the current state of ENT teaching in Queensland. In particular, it demonstrates the lack of formal ENT teaching received by medical students and the sentiment by interns that their formal ENT teaching was insufficient, especially in the context of the frequency of encountering ENT pathologies in clinical practice. While there is a lack of recent Australian data into the inadequacy of teaching and placement time in ENT, our results reflect the broader trends to this effect seen in the UK, US and Canada (12-15).
The time allocated to ENT varies between universities and as with all specialties, requires integration with all aspects of medicine. It is imperative that the time allocated to ENT teaching is of high utility and value to medical students. Although some students felt they had sufficient teaching in medical school, a majority felt it was lacking in utility. Of students allocated to a specialist ENT service, a majority found this significantly more valuable than what is learned in a classroom. Unfortunately, in a practical sense, there is insufficient time to allocate every student to an ENT service. Challenges also pertain to the geographical distribution of ENT services within Queensland. Only 12 hospitals within Queensland Health have an active ENT service, making it quite difficult to allocate all medical students in Queensland, especially those placed in rural and regional areas. Notably, there was significant variability with respect to the amount of ENT teaching and duration of placement (if any) within individual universities, making this less likely to be a confounder.
It should be of no surprise that many interns felt they were lacking in basic clinical examination skills in ENT. An Australian survey by Rolfe et al. (7) found that 73.9% of interns (PGY1) reported they needed more medical school preparation in the examination of the ENT. In the same survey, 73.8% of medical students felt they needed more skills in packing a bleeding nose. Niermeyer et al. (15) recently highlighted a similar situation in the US, where 65% of respondents reported receiving less ENT training than expected, with concomitantly low confidence in otoscopic examination. Our results reflect the literature with the highest number of respondents reporting only basic skills in all areas of clinical examination.
Questions regarding the diagnosis and management of common ENT pathologies yielded varying and insightful responses. Many interns felt comfortable diagnosing and managing the most common ENT pathologies. The majority of interns reported being relatively comfortable treating epistaxis. Often in epistaxis, the clinical situation can escalate rapidly making it difficult to manage, even for the experienced otolaryngologist. Their self-reported inadequacy of medical school education was further demonstrated in how the majority of interns responded that they ‘may require some assistance’ when asked regarding stridor. A stridulous patient should serve as a warning for a potentially serious condition and airway compromise. Management of stridor should almost immediately involve senior help or specialist ENT advice. This suggests that junior doctors may not be able to recognise this potentially life-threatening sign and seek appropriate and timely help, and is consistent with a Canadian study which identified that the majority of respondents “lacked confidence recognizing conditions requiring emergent referral” (13).
The response to management of tracheostomies is somewhat as expected. Tracheostomies are often viewed as foreign and many doctors lack the confidence to manage tracheostomies. Often, this is due to lack of knowledge from clinicians outside of ENT and critical care, and having some hesitancy with management of this condition is not unreasonable. Issues with tracheostomies may be competently managed by an ENT surgeon, however it is important for junior doctors to have an understanding of the concepts of tracheostomy as applied in emergency and critical care contexts.
Our two tailed analysis of the data demonstrated that interns who in medical school received more than 1 week of ENT teaching or had an attachment to a specialist ENT service self-rated their competence in clinical examination more highly. As expected, these subjective benefits did not extend to the diagnosis and management of common conditions, as medical students typically participate more in clinical examination and less in diagnosis and management. This is corroborated with data from other countries including the US and Canada, where ENT exposure was positively associated with clinical knowledge, and in turn, comfort in managing ENT pathologies (13,16).
Our secondary aim in this survey was to assess the value of various types of learning resources. From the responses of the interns surveyed, traditional lectures and tutorials still maintain a vital role in learning. Most participants had access to online resources, but newer modalities such as voice-over PowerPoints and podcasts were not ranked as very helpful. Many ENT pathologies require practical input including use of equipment such as otoscopes and insertion of nasal packs. These could easily be demonstrated on an education day for students and would likely be highly valuable. The most popular suggestion was a workshop-based clinical experience with practical learning. The utility of this suggestion is supported by the results of a recent systematic review by Yip et al. (14), where practical solutions including an ENT boot camp involving simulation, and nasolaryngoscopy training, were associated with marked and objective improvements in clinical knowledge and skills. Although valuable, this teaching method would require dedicated preparation and funding by medical schools to enable effective delivery (14).
The responses to the final group of questions provide insight into what interns view as important with respect to time-allocation. Interns believed that a minimum of 5 days of ENT teaching and greater than 1 week allocated to a specialist ENT service was appropriate for their learning. Enabling this within the confines of a busy medical school placement schedule is a large undertaking which is practically difficult to overcome. It is obvious from our survey that interns believe this is an important aspect of their curriculum and the majority feel they had insufficient ENT exposure during medical school.
Limitations
We acknowledge that it is difficult to draw significant conclusions about ENT teaching in medical school in Queensland within the constraints of a voluntary survey. Although efforts were made to maximise our sample size, our response rate was low. The final sample included in our analysis was small and involved a small number of hospitals, resulting in decreased study power. It is worth noting that the majority of interns surveyed graduated from The University of Queensland and were employed at The Royal Brisbane and Women’s Hospital. Our capacity to determine the external validity of this study was also limited through the lack of demographic data collected, particularly gender and rurality. This information would also have been useful in evaluating the influence of ENT exposure on potential career choices and importantly, the diversity of trainees entering the profession. In spite of this, we believe this is representative of the intern cohort in Queensland as exposure and experiences in ENT even within individual universities were also very heterogeneous.
It was not the aim of this survey to scrutinise individual medical schools and their curricula; rather, to identify potential areas of improvement. Our results encompass a heterogenous group of interns at the end of their hospital year and interns at the start of their hospital year. Although curriculum and syllabus information was sought from each Queensland medical school, information regarding the number of ENT teaching days was not provided or available. This is also a recognition that teaching can often be ad hoc rather than formal. In addition, ENT placement availability differs according to the hospital a student is placed at, or according to a student’s choice of elective. The inherent heterogeneity of this means there is no set number of teaching or placement days that can be provided per hospital or medical school, and thus, in practice is unable to be reliably quantified objectively. We acknowledge that the external validity of our results may be reduced as a consequence of this, especially in relation to the clinical questions asked of respondents.
The subjectivity of interns self-reporting their competence in relation to clinical skills limits the utility of the results. Objective measures of clinical skills in ENT would be needed to bolster the internal validity of the results of future surveys. Likert scales and questionnaires are also inherently limited by response bias and restricted choice. Further to this, when two groups were compared in our analysis, the sizes of the individual groups were quite small, and one group was significantly larger than the other. This limited our ability to measure statistically valid outcomes, and the direction and magnitude of the effect.
Conclusions
In all areas of medicine, it is our professional duty as clinicians to educate our junior doctors and medical students. Their preparedness in managing common ENT conditions is at least in part our responsibility, and the establishment of a solid framework in knowledge and clinical acumen begins in medical school. Our survey identifies that education in medical school is lacking in our speciality and this can significantly affect patient care and outcomes. There is insufficient breadth and duration of ENT teaching delivered in medical schools. We demonstrated that interns value interactive, in-person ENT education and find attachments to specialist ENT services useful for their knowledge and clinical skills. Time attached to specialist ENT services was associated with higher levels of self-reported clinical knowledge and skills among respondents. Most respondents reported they had insufficient ENT exposure as medical students and agreed that ENT should be a compulsory part of the medical school curriculum, including attachments to specialist ENT services.
Methods to improve medical education in ENT will require substantial work with medical schools to identify areas of deficiency and means of improvement. In particular, education could be improved through establishing ENT teaching and placement as part of the core curriculum. This could entail more dedicated teaching time using favoured in-person pedagogical methods including tutorials, simulations, and workshops, and the introduction of ENT teaching where it is not present. To achieve this, we would need the recruitment of experienced registrars or consultants as educators. Integrating medical student teaching into the curriculum of training ENT registrars would assist us in realising this goal. This would provide a valuable resource for medical students and also cultivate one of the core clinical competencies underpinning surgical training. The establishment and integration of medical student teaching into training would require significant collaboration with The Royal Australasian College of Surgeons.
The literature shows practical skills sessions including interactive workshops are most effective for improving clinical knowledge and skills, although these require extensive medical school engagement and funding to develop. Recent adaptations in the delivery of healthcare could assist in developing innovative teaching methods to ensure that students outside of ENT-serviced hospitals are provided with the same educational experience. The establishment of an online live tutorial focusing on practical skills and stations with utilisation of local staff and equipment may provide an invaluable resource.
Further to this, the provision of ENT teaching resources including lecture materials and texts is imperative. The inclusion of placements with specialist ENT services would also be of significant benefit, given that interns rated their experiences on placement as highly useful, and there were measurable improvements in self-reported clinical skills associated with placements. We acknowledge that the implementation of the above suggestions would necessitate significant efforts from medical schools and consultation with health services to facilitate additional student placements.
Further research in this area could encompass interns and other resident medical officers working in other Australian states and territories, while including further demographic information including gender and rurality. The value of medical student opinion in this area must also not be discounted, given their contemporaneous experience of medical school curricula. This may also provide some insight into how other medical schools may be approaching this challenging issue in medical education.
Acknowledgments
The authors acknowledge and thank the following for their contributions: This work was supported by the medical education units of respective hospitals who assisted us with the distribution and collection of surveys.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-87
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-87
Peer Review File: Available at http://dx.doi.org/10.21037/ajo-20-87
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-87). AC serves as an unpaid editorial board member of the Australian Journal of Otolaryngology from Jan 2019 to Dec 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Multi-site ethics approval was obtained from Royal Brisbane and Women’s Hospital Human Research Ethics Committee (LNR/2019/QRBW/51023) and all respondents provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferguson GR, Bacila IA, Swamy M. Does current provision of undergraduate education prepare UK medical students in ENT? A systematic literature review. BMJ Open 2016;6:e010054 [Crossref] [PubMed]
- Australian Institute of Health and Welfare. Emergency department care 2017–18: Australian hospital statistics. Health services series No 89, 2018.
- Cooke G, Valenti L, Glasziou P, et al. Common general practice presentations and publication frequency. Aust Fam Physician 2013;42:65-8. [PubMed]
- Clamp PJ, Gunasekaran S, Pothier DD, et al. ENT in general practice: training, experience and referral rates. J Laryngol Otol 2007;121:580-3. [Crossref] [PubMed]
- Ishman SL, Stewart CM, Senser E, et al. Qualitative synthesis and systematic review of otolaryngology in undergraduate medical education. Laryngoscope 2015;125:2695-708. [Crossref] [PubMed]
- Chawdhary G, Ho EC, Minhas SS. Undergraduate ENT education: what students want. Clin Otolaryngol 2009;34:584-5. [Crossref] [PubMed]
- Rolfe IE, Pearson S, Sanson-Fisher RW, et al. Identifying medical school learning needs: a survey of Australian interns. Educ Health (Abingdon) 2001;14:395-404. [Crossref] [PubMed]
- Khan MM, Saeed SR. Provision of undergraduate otorhinolaryngology teaching within General Medical Council approved UK medical schools: what is current practice? J Laryngol Otol 2012;126:340-4. [Crossref] [PubMed]
- Campisi P, Asaria J, Brown D. Undergraduate otolaryngology education in Canadian medical schools. Laryngoscope 2008;118:1941-50. [Crossref] [PubMed]
- Haddad J, Shah J, Takoudes TG. A Survey of US Medical Education in Otolaryngology. Arch Otolaryngol Head Neck Surg 2003;129:1166-9. [Crossref] [PubMed]
- Fox R, Nash R, Liu ZW, et al. Epistaxis management: current understanding amongst junior doctors. J Laryngol Otol 2016;130:252-5. [Crossref] [PubMed]
- Wong K, Jang M, Gilad A, et al. Quantifying Medical Student Education and Exposure to Otolaryngology. Ann Otol Rhinol Laryngol 2017;126:493-7. [Crossref] [PubMed]
- Rosvall BR, Singer Z, Fung K, et al. Do Medical Students Receive Adequate Otolaryngology Training? A Canadian Perspective. Ann Otol Rhinol Laryngol 2020;129:1095-100. [Crossref] [PubMed]
- Yip HM, Soh TCF, Lim ZZ. Current innovations in otolaryngology medical education in the UK: a systematic literature review. J Laryngol Otol 2020;134:284-92. [Crossref] [PubMed]
- Niermeyer WL, Philips RHW, Essig GF Jr, et al. Diagnostic accuracy and confidence for otoscopy: Are medical students receiving sufficient training? Laryngoscope 2019;129:1891-7. [Crossref] [PubMed]
- Pasick LJ, Benito D, Zapanta P, et al. Assessing Medical Student Basic Otolaryngology Knowledge: A Multi-Institutional Study. Ear Nose Throat J 2019;98:44-9. [Crossref] [PubMed]
Cite this article as: Yau S, Wong M, Cervin A. A survey of Queensland medical education in otolaryngology. Aust J Otolaryngol 2021;4:20.



