
Tonsillectomy: does proximity from otolaryngology care influence the intra-operative or post-operative plan?
Introduction
Tonsillectomy is one of the most common procedures performed by Ear, Nose and Throat (ENT) surgeons, with over 40,000 cases performed annually in Australia (1). Indications for tonsillectomy include recurrent tonsillitis, peritonsillar abscess and obstructive sleep apnoea (OSA) (2). In Australia and New Zealand, ENT surgeons are faced with the challenge of providing care across a vast geographical area, with disparity between the number of practicing otolaryngologists in rural and remote areas as compared to major metropolitan areas (3,4). As per the most recent National Health Workforce Survey published in 2017, 85.0% of Australian ENT surgeons primarily practice in a major city (4). For many clinicians, concerns for postoperative haemorrhage influence recommendations in regard to disposition.
Surgeons who operate on patients in regional and rural areas in Australia and New Zealand must acknowledge an adjusted risk profile in regard to timing of discharge and disposition. This is in view of reduced access to emergency and/or otolaryngology care for post-operative complications (1). Anecdotally, there is a lack of consensus regarding patient selection and optimal timing of disposition (discharge from hospital and/or return to place of residence). There is no consensus statement or guideline that dictates proximity to the provider or emergency service in order to address catastrophic haemorrhage and/or death. It is unclear if a change to surgical technique or post-operative care is warranted in patients who reside a significant distance from ENT care. Additionally, there is limited data regarding postoperative tonsillectomy outcomes in relation to geographical distribution.
A survey of Australian Society of Otolaryngology Head and Neck Surgery (ASOHNS) and New Zealand Society of Otolaryngology Head and Neck Surgery (NZSOHNS) members was performed. The primary outcome was to ascertain opinion amongst ENT surgeons as to whether patients should stay in close proximity to an ENT serviced hospital following tonsillectomy. Secondary outcomes captured current trends in practice, operative technique and management preferences. Further opinions from surgeons were sought to determine if the age of the patient or intended disposition instigated a change in usual practice. We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/ajo-21-9).
Methods
Participants were invited to complete a 29-item, structured questionnaire if they were registered ordinary members of ASOHNS and NZSOHNS (Appendix 1). The survey was disseminated to members via email from ASOHNS and NZSOHNS respectively using Survey MonkeyTM. One reminder email was sent 4 weeks later. Completed questionnaires were returned to ASOHNS. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Surgeons participated voluntarily in this survey without personal or financial incentive.
Statistical analysis
The collated data from returned surveys was analysed using Microsoft ExcelTM to produce comparable data between cohorts from Australia and New Zealand.
Results
Demographics
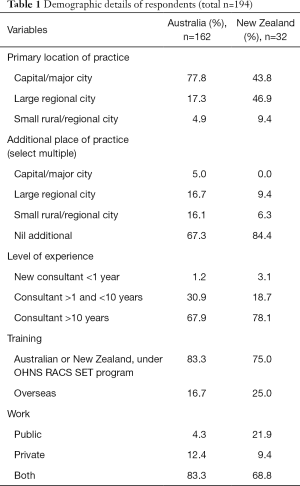
A survey response rate of 162 of 490 members (33.1%) in Australia and 32 of 131 members (24.4%) in New Zealand was achieved. In Australia, the primary place of practice was identified as “Capital/major city” (77.8%), with “Large regional city” (17.5%) and “Small rural/regional” following (4.9%). In New Zealand, the primary place of practice was predominantly “Large regional city” (46.9%), followed by Capital/major city” (43.8%) and “Small rural/regional” (9.4%) (demographic details can be observed in Table 1).
Full table
Surgical technique
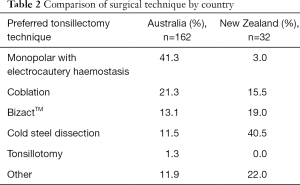
In Australia, the preferred technique of tonsillectomy was reported as “Monopolar with electrocautery haemostasis” (41.3%), followed by “Coblation” (21.3%), “BiZactTM” (13.1%), “Cold steel” (11.3%) and “Tonsillotomy” (1.3%), whilst 11.9% of surgeons employ “Other” methods including bipolar diathermy and dissection scissors (see Table 2). By comparison, surgeons within New Zealand reported “Cold steel” as the most popular technique (40.5%) followed by “Other” (22.0%), “BiZactTM” (19.0%), “Coblation” (15.5%) and “Monopolar with electrocautery haemostasis” (3.0%). The majority of surgeons from both countries reported that they did not change their surgical technique when operating on paediatric patients (85.0% of Australians, 90.1% of New Zealand surgeons).
Full table
Acceptable postoperative proximity
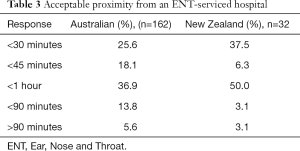
The most acceptable postoperative proximity from an ENT-serviced hospital following tonsillectomy was less than 1 hour in both New Zealand and Australia (50.0% and 36.9% respectively), though a range of responses was noted (Table 3).
Full table
Care preferences in view of geographical proximity
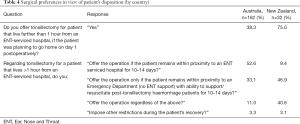
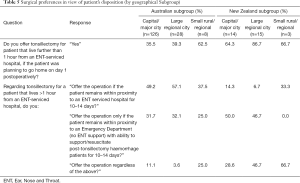
Regarding the primary objective, which may be noted in Table 4, 61.7% of the total Australian cohort would not offer a tonsillectomy if the patient resided beyond 1 hour from an ENT serviced hospital. This can be compared to 25.0% of New Zealand surgeons who would not offer tonsillectomy to patients if they resided over an hour away from an ENT serviced hospital. Most Australian surgeons would only offer a tonsillectomy to these patients if they remained within proximity to an ENT serviced hospital for 10–14 days (52.6%). This may be compared to 9.4% of surgeons in New Zealand who would mandate the same action. Surgeons in New Zealand were more likely to counsel patients to remain in proximity to an Emergency Department that could provide support/resuscitation measures (46.9%) or operate regardless of proximity (40.6%). A further subgroup analysis by primary place of practice was performed as per Table 5.
Full table
Full table
Sub-group analysis—capital/major city
Of the 126 Australian surgeons primarily based in a capital/major city, 18.0% performed tonsillectomy additionally in a large regional city and 13.5% in a small rural/regional centre. 64.5% of surgeons would not offer tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital if the patient was planning on returning home day 1 postoperatively. For these patients, 49.2% of surgeons would offer tonsillectomy only if the patient remained within proximity to an ENT-serviced hospital for 10–14 days postoperatively.
These findings can be compared to surgeons located in major cities in New Zealand. Of the 14 surgeons that were based primarily in a capital/major city, none performed tonsillectomy in a large regional city and 5.5% additionally did so in a small rural/regional centre. Surgeons were more likely to provide tonsillectomy to distant patients, with only 35.7% not offering tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital and were planning on returning home day 1 postoperatively. For the group of patients living more than 1 hour from an ENT-serviced hospital, 14.3% of surgeons would require patients to remain within proximity to an ENT-serviced hospital for 10-14 days postoperatively. We note 50.0% of these surgeons would however prefer patients to remain in proximity to an Emergency Department during the recovery period.
Sub-group analysis—large regional city
Of the 28 Australian surgeons that were based primarily in a large regional city, 25.0% additionally performed tonsillectomy in other large regional cities or small rural/regional centres. The Australian group were again observed to practice more conservatively, with 60.7% of respondents stating they did not offer tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital and were planning on returning home day 1 postoperatively. For the group of patients living more than 1 hour from an ENT-serviced hospital, 57.0% of surgeons would offer tonsillectomy only if the patient remained within proximity to an ENT-serviced hospital for 10–14 days postoperatively.
In New Zealand, of the 15 surgeons that were based primarily in a large regional city or small rural/regional centre, 20.0% performed tonsillectomy in other large regional cities or small rural/regional centres; 13.3% of surgeons would not offer tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital and were planning on returning home day 1 postoperatively. For the group of patients living more than 1 hour from an ENT-serviced hospital, 6.7% of surgeons would only offer tonsillectomy if the patient remained within proximity to an ENT-serviced hospital for 10–14 days postoperatively.
Sub-group analysis—small rural/regional centre
Of the 8 Australian surgeons that were based primarily in a small rural/regional centre, 62.5% performed tonsillectomy in other large regional cities or small rural/regional centres. 37.5% of surgeons would not offer tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital and were planning on returning home day 1 postoperatively. For the group of patients living more than 1 hour from an ENT-serviced hospital, 37.5% of surgeons would offer tonsillectomy only if the patient remained within proximity to an ENT-serviced hospital for 10–14 days postoperatively.
In New Zealand, of the 3 surgeons that were based primarily in a small rural/regional centre, none performed tonsillectomy in other large regional cities or small rural/regional centres. 33.3% of surgeons would not offer tonsillectomy to patients if they lived more than one hour from an ENT-serviced hospital and were planning on returning home day 1 postoperatively. For the group of patients living more than 1 hour from an ENT-serviced hospital, 33.3% of surgeons would offer tonsillectomy only if the patient remained within proximity to an ENT-serviced hospital for 10–14 days postoperatively.
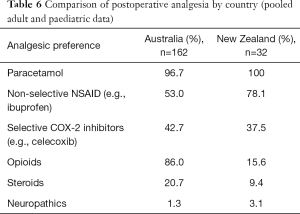
Analgesia
Regarding analgesic regimes, surgeons in Australia reported that their discharge plans included paracetamol (96.5%), opioids (86.0%), non-selective NSAIDS (56.0%), selective COX-2 inhibitors (42.7%), steroids (20.7%) and neuropathics (1.5%) (see Table 6). In New Zealand, all surgeons utilized paracetamol on discharge and appeared more comfortable with use of non-selective NSAID than their Australian colleagues, with 78.1% of respondents including the class routinely. Conversely, only 15.6% of surgeons in New Zealand stated they would routinely utilize opioid medications on discharge compared to 86.0% of Australians reported above. In New Zealand, other analgesic options included selective COX-2 inhibitors (37.5%), steroids (9.4%) and neuropathics (3.1%). For patients residing greater than 1 hour from an ENT-serviced hospital, 96.0% of Australian and 93.5% of surgeons from New Zealand would not alter their standard analgesic regimes or restrict any medications on discharge (92.6% of Australian and 96.9% of New Zealand surgeons).
Full table
Discharge plan
Regarding discharge, 21.5% of Australian surgeons routinely discharged their patients from hospital on the day of surgery, whilst 78.5% preferred to discharge patients on day 1 postoperatively. In comparison, 38.5% of respondents from New Zealand routinely discharged their patients on the day of surgery, whilst 61.5% discharged on postoperative day 1. Most surgeons maintained the same discharge protocol between adult and paediatric patients (90.6% and 90.0% of New Zealand and Australian surgeons respectively). For patients who resided greater than an hour away, 77.9% of Australian surgeons and 62.5% of New Zealand based surgeons did not change their usual discharge practice. For those who did report a shift, 19.9% of Australians and 34.4% of New Zealand reported keeping patients until day 1 postoperative. No surgeons from New Zealand and only 1.9% of Australian surgeons reported keeping patients as an inpatient for more than 1 day if they lived greater than 1 hour away from an ENT-serviced hospital.
Conclusions
According to the ASOHNS administration, the Australian response rate of 33.1% met the expected result for email surveys. The New Zealand response rate was however slightly lower than expected at 24.4%. This has introduced a potential for sample bias and limited generalisability of findings. A study scrutinizing survey methods however, has demonstrated an acceptable response rate may vary between 25.0–33.3% when delivered via email (5). Whilst the advantages of email surveys include immediate, widespread distribution and low expenditure, it is a modality that has been shown to have consistently poorer response rates than paper or face-to-face methods (6).
The demographic results are largely representative of the known ENT community and parallel the distribution noted in the most recent surgical workforce data published in 2017 (4). The majority of ENT surgeons (85.0%) undertake their primary practice in a major city, with occasional work in more isolated settings. ENT services in both Australia and New Zealand are primarily provided via major hospitals, though a more even distribution of surgeons was noted between major cities and large regional centres in New Zealand (4). The smaller geographical size of New Zealand may contribute to this finding, as there are fewer peripheral towns and hospitals than in Australia (7). Despite its smaller size, healthcare in New Zealand is challenged by unique regions of tortuous roadways and landscapes that pose considerable effort to traverse (8). A 2002 study indicated 1.5 million people in New Zealand (38.5% of the population at this time) resided an average of 89.5 minutes from a major hospital, when considering the sinuosity of roadways (8). Interestingly, few respondents from New Zealand indicated that an appropriate destination following tonsillectomy was greater than 90 minutes, however this is likely to represent a significant proportion of the population. Similar challenges also exist in Australia, with significant distance affecting the accessibility of specialist services (9). Approximately 7 million people live outside major cities (representing 29% of the population) (10). Access for these patients can be diverse, as specialist care differs amongst the states and territories. There is a greater proportion of regional ENT health services in more populated states, such as New South Wales, Queensland and Victoria. In Western and South Australia, access to ENT care is largely confined to the capital city and so patients must travel in order to seek surgical care (10). Despite the challenges posed by this distance, there is no geographically based data to suggest that patients living in these regions suffer worse surgical outcomes than their peers in major cities post tonsillectomy.
This study indicated that Australian surgeons are more likely to be conservative in their delivery of tonsillectomy care than their peers in New Zealand. Additionally, the data showed that surgeons in major cities practice more conservatively than their colleagues in smaller regional and rural settings, who may be more comfortable with the concept of reduced access to care, or have greater experience dealing with medical emergencies in a lesser resourced setting. Despite this, few surgeons from either country indicated that a patient’s proximity to surgical care, nor the age of the patient, instigated a change in preferred operative technique or analgesic routine, indicating a generally high degree of confidence in their standard practice. Counselling patients to remain in close proximity following surgery can be associated with significant financial cost; when travel expense, time off work for recovery or caring roles, accommodation fees and cost for families with more than one child are considered. As retrieval and readmission data is not available for patients post tonsillectomy, it is difficult to compare the personal cost of remaining close to care postoperatively to the public health cost of managing complications when they arise. This is a significant gap identified in this study, and would be a valuable area of future study in the face of a growing population and growth in regional and rural populations, to ensure service provision and care is evidence based. The introduction of The Australian Otolaryngology Outcome and Quality Assurance Network (AOQAN) in 2018 may assist in resolving this in time, as a national database which is able to log outcome data securely (11). Further, it would be of value to clarify the instructions provided to patients on disposition to examine the degree of consensus. In this study, there was scope for surgeons to enter free text to the questions regarding their preferred mode of practice, however these were inconsistently utilised and in too low a number to provide meaningful insight on this occasion.
Ultimately, we assume the main reason to counsel patients to remain close to an Emergency or ENT-serviced hospital is the perceived risk of catastrophic haemorrhage postoperatively. Primary haemorrhage, defined as bleeding within 24 hours of the operation, carries a prevalence of 0.2–2.2%, whist the rate of secondary haemorrhage, defined as occurring after 24 hours from surgery, ranges from 0.1–3.0% (3). In other terms, approximately 97.0% of patients will not experience a bleed in the subsequent two weeks post discharge. There has been a significant amount of research dedicated to identifying adjustable factors within routine surgical care, which may contribute to postoperative complications. The choice of tonsillectomy technique is based upon a perceived risk versus benefit assessment with regard to reduced intraoperative or postoperative bleeding and pain (2). The data in this study revealed that Australian surgeons are more likely to prefer “Monopolar with electrocautery haemostasis” technique. This trend is similarly reported amongst other retrospective studies such as the article published by Macfarlane et al. in 2008 (1). This is in contrast to colleagues in New Zealand, who describe a preference for “cold steel” dissection technique. Given that less surgeons in Australia report cold steel technique as their preferred method, it is similarly likely that less trainees are exposed to this technique and thus, it is not a technique commonly used in Australia. Monopolar diathermy has lost favour in the United Kingdom following a large systematic review of the safety of electrosurgery in tonsillectomy published in 2006 (12). This study, which also examined the data from a large national audit of tonsillectomy practice (13), concluded that electrosurgical dissection and haemostasis held a causal relationship with a higher rate of secondary haemorrhage than the cold steel alternative, which required operative intervention (12). Conversely, it also indicated that cold steel techniques may be associated with an increased prevalence of primary haemorrhage (12). This preference for avoiding “hot” surgical techniques has been similarly reported in an observational longitudinal cohort study in Sweden, which observed the outcomes of 98,979 tonsil surgeries (14). This outcome of this study similarly supported evidence that cold surgical techniques were related to a significantly lower risk of late bleeding complications. In keeping with this, the study also reported an associated moderate shift in practice amongst large Swedish ENT centres to adopt more cold techniques as the results became apparent, with two quality improvement projects over which the data was collated (14).Indeed, secondary haemorrhage in patient cohorts in Australia and New Zealand may be considered more important, as they occur in the timeframe that patients may return home and beyond the proximity of an ENT-serviced hospital. A challenging aspect of post-operative care following tonsillectomy, is that a secondary haemorrhage can occur up to 2–3 weeks after the procedure (2). Surprisingly, there is limited data available for when post tonsillectomy haemorrhage occurs most frequently in Australia, though data published in the International Journal of Otolaryngology reported that bleeds most commonly occur at a mean of 6.1 days following surgery (15). In regard to surgical outcomes, technique remains an area of controversy—particularly in view of postoperative disposition and access to emergency care.
Analgesic regimes have also come under scrutiny, particularly in view of NSAID and opioids, which have been associated with an array of complications, including increased severity of post tonsillectomy haemorrhage and respiratory depression (16). In this study, Australian surgeons were less likely than their peers in New Zealand to incorporate NSAIDs into their treatment plan. The routine use of NSAIDs post tonsillectomy remains controversial in view of potential platelet dysfunction and the impact that this has on the frequency and severity of post-tonsillectomy haemorrhage. A Cochrane review suggested insufficient evidence to exclude an increased risk of bleeding with the use of NSAIDs in paediatric cohorts (16). In the same review, the authors found a decrease in post-operative emesis when NSAIDs have been incorporated into the analgesic regime, which may enable increased oral intake and reduced pain (16). Conversely, a systematic review and meta-analysis of 36 randomized controlled trials in 2013 has determined no apparent association between NSAID use and increased bleeding, need for readmission and—importantly for the outcomes of this study, no increased rate of secondary haemorrhage nor return to theatre (17). One revealing study however has noted that whilst the frequency of post tonsillectomy haemorrhage may not increase, the severity and thus need for transfusion is 3 times higher when ibuprofen is utilised (18). Given the spectrum of controversy amongst the literature, it is not surprising to observe disparity amongst the surgeons we surveyed. Australian surgeons are, however, more likely to incorporate opioids routinely on discharge. Care must be advised in regard to the use of opioids in the subgroup of children who have undergone tonsillectomy for OSA, given the risk of respiratory depression (19). Children with OSA symptoms and blood oxygen levels of <85% are more sensitive to opioid medications and are at risk of opioid-related respiratory depression and death (19). Our study did not examine the change in tonsillectomy practice as per indication for tonsillectomy, and so may not have captured relevant changes in this practice. The use of steroids postoperatively similarly remains controversial in regard to the actual benefit they convey, with ongoing variation in routine use between New Zealand and Australia noted in this study. One retrospective study of 1,200 children undergoing tonsillectomy has demonstrated an improvement in both pain and haemorrhage rates with a short course of 3 doses of dexamethasone postoperatively (20). This trend has been similarly identified in adults in a study from Saudi Arabia, with lower rates of pain (21). A concern has been raised however following a meta-analysis of 29 randomized controlled trials, that there is an increased incidence of bleeding episodes which require an intervention (22). This is perhaps of greater significance when considering our outcomes, with a focus on reducing the chance of secondary haemorrhage after patients return to their home. Ultimately, the postoperative analgesic regime is largely formulated based on surgeons training and experiences and requires ongoing evaluation.
Same day discharge post tonsillectomy is popular in Europe and the UK (1). An audit of Australian practice revealed that only 1 in 4 surgeons in Australia routinely practiced same-day discharges in 2008 (1). The data obtained in this study indicates the same trend continues in Australia. Colleagues in New Zealand were slightly more likely to support same-day discharge. This practice carries benefits for improved health care cost efficiency (1). It also however requires careful patient selection to ensure adequate analgesia, recovery from anaesthetic and oral hydration. A retrospective study examining paediatric short stay tonsillectomy found that indeed, a short 3 hour stay for observation, following tonsillectomy was safe and was not associated with significant variation in complication rates (23). Further research may be warranted to better identify patients who are likely to benefit from a more prolonged outpatient observation than those who may be discharged home following surgery.
A limitation of this study includes the response rate outlined above. “Survey fatigue” defined as the sense of over-exposure to the survey process, has been suggested as an emerging challenge in obtaining feedback from participants (24). This may be, particularly relevant, as this study was conducted during the COVID-19 pandemic, when obtaining face-to-face insights has not been possible. As a result, the method utilized bears potential for selection and non-response bias and may be poorly representative of the total New Zealand Otolaryngology workforce, however this is inherent in any open survey. There were no individual financial or personal incentives offered for the completion of this survey. Additionally, the survey did not investigate the availability of retrieval services and how this may affect decision making. This may be an area of future research that could be strengthened by data from the AOQAN in regard to retrieval and readmission rates. Finally, we note that some clinicians are directed by hospital-led guidelines with protocolise timing of discharge and geographic disposition, particularly for paediatric cohorts. It is studies such as the one reported that may influence future guidelines development and shifts in such hospital mandates—particularly when strengthened by future available outcome data.
The results obtained in this study indicate that Australian surgeons are more likely to counsel patients to stay in close proximity to an ENT-serviced hospital than their colleagues in New Zealand despite a lack of clinical evidence for or against. Postoperative proximity to ENT services does not result in changes to preferred operative technique or analgesia routine for children or adults. Data indicates that surgeons in major cities practice more conservatively than their peers in smaller regional and rural settings. This study has highlighted several areas of beneficial future research to guide evidence-based practice, particularly in regard to adverse surgical outcomes in regional centres and retrieval rates post tonsillectomy.
Acknowledgments
This work was supported by the Australian and New Zealand Societies of Otolaryngology Head and Neck Surgery. The authors extend their appreciation for their assistance in disseminating the survey utilized in this study, as well as the members for their participation.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/ajo-21-9
Data Sharing Statement: Available at https://dx.doi.org/10.21037/ajo-21-9
Peer Review File: Available at https://dx.doi.org/10.21037/ajo-21-9
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/ajo-21-9). NJ serves as a paid lecturer and instructor in Smith & Nephew. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Surgeons participated voluntarily in this survey without personal or financial incentive.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Macfarlane PL, Nasser S, Coman WB, et al. Tonsillectomy in Australia: an audit of surgical technique and postoperative care. Otolaryngol Head Neck Surg 2008;139:109-14. [Crossref] [PubMed]
- Gallagher TQ, Wilcox L, McGuire E, et al. Analyzing factors associated with major complications after adenotonsillectomy in 4776 patients: comparing three tonsillectomy techniques. Otolaryngol Head Neck Surg 2010;142:886-92. [Crossref] [PubMed]
- Kwok M, Subramaniyan M, Rimmer J, et al. Post-tonsillectomy haemorrhage in Australia—a multivariable analysis of risk factors. 2018;1.
- Department of Health. Otolaryngology - 2016 Factsheet. 2017. Available online: https://hwd.health.gov.au/webapi/customer/documents/factsheets/2016/Otolaryngology.pdf. Accessed 7th February 2021.
- Nulty D. The adequacy of response rates to online and paper surveys: what can be done? Assessment & Evaluation in Higher Education 2008;33:301-14. [Crossref]
- Lindemann N. What’s the average survey response rate? Survey Anyplace 2019. Available online: https://surveyanyplace.com/average-survey-response-rate/. Accessed 6th February 2021 2021.
- Geoscience Australia. Areas of Australia, States and Territories. Available online: https://www.ga.gov.au/scientific-topics/national-location-information/dimensions/area-of-australia-states-and-territories. Accessed 4th February 2021 2021.
- Brabyn L, Skelly C. Modeling population access to New Zealand public hospitals. Int J Health Geogr 2002;1:3. [Crossref] [PubMed]
- Australian Institute of Health and Welfare. Rural and remote health. 2019. Available online: https://www.aihw.gov.au/reports/rural-remote-australians/rural-remote-health/contents/profile-of-rural-and-remote-australians. Accessed 7th February 2021 2021.
- Gao C, Ogeil R. Australia's Health 2018 Australia's Health and Welfare. 2018. Available online: https://www.aihw.gov.au/getmedia/0c0bc98b-5e4d-4826-af7f-b300731fb447/aihw-aus-221-chapter-5-2.pdf.aspx. Accessed 4th February 2021 2021.
- Australian Society of Otolaryngoloy Head and Neck Surgery. AOQAN - Australian Otolaryngology Quality Assurance Network. The basis for evidence based medicine in Ear Nose and Throat Head and Neck Surgeons in Australia. 2018. Available online: https://www.aoqan.org
- Mowatt G, Cook JA, Fraser C, et al. Systematic review of the safety of electrosurgery for tonsillectomy. Clin Otolaryngol 2006;31:95-102. [Crossref] [PubMed]
- Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope 2007;117:717-24. [Crossref] [PubMed]
- Lundström F, Stalfors J, Østvoll E, et al. Practice, complications and outcome in Swedish tonsil surgery 2009-2018. An observational longitudinal national cohort study. Acta Otolaryngol 2020;140:589-96. [Crossref] [PubMed]
- Hussain S, O'Connell Ferster AP, Carr MM. Time between First and Second Posttonsillectomy Bleeds. Int J Otolaryngol 2017;2017:3275683 [Crossref] [PubMed]
- Lewis SR, Nicholson A, Cardwell ME, et al. Nonsteroidal anti-inflammatory drugs and perioperative bleeding in paediatric tonsillectomy. Cochrane Database Syst Rev 2013;2013:CD003591 [Crossref] [PubMed]
- Riggin L, Ramakrishna J, Sommer DD, et al. A 2013 updated systematic review & meta-analysis of 36 randomized controlled trials; no apparent effects of non steroidal anti-inflammatory agents on the risk of bleeding after tonsillectomy. Clin Otolaryngol 2013;38:115-29. [Crossref] [PubMed]
- Mudd PA, Thottathil P, Giordano T, et al. Association Between Ibuprofen Use and Severity of Surgically Managed Posttonsillectomy Hemorrhage. JAMA Otolaryngol Head Neck Surg 2017;143:712-7. [Crossref] [PubMed]
- Sadhasivam S, Myer CM. Preventing opioid-related deaths in children undergoing surgery. Pain Med 2012;13:982-3; author reply 4. [Crossref] [PubMed]
- Redmann AJ, Maksimoski M, Brumbaugh C, et al. The effect of postoperative steroids on post-tonsillectomy pain and need for postoperative physician contact. Laryngoscope 2018;128:2187-92. [Crossref] [PubMed]
- Al-Shehri AM. Steroid therapy for post-tonsillectomy symptoms in adults: a randomized, placebo-controlled study. Ann Saudi Med 2004;24:365-7. [Crossref] [PubMed]
- Plante J, Turgeon AF, Zarychanski R, et al. Effect of systemic steroids on post-tonsillectomy bleeding and reinterventions: systematic review and meta-analysis of randomised controlled trials. BMJ 2012;345:e5389 [Crossref] [PubMed]
- Lalakea ML, Marquez-Biggs I, Messner AH. Safety of pediatric short-stay tonsillectomy. Arch Otolaryngol Head Neck Surg 1999;125:749-52. [Crossref] [PubMed]
- Patel SS, Webster RK, Greenberg N, et al. Research fatigue in COVID-19 pandemic and post-disaster research: Causes, consequences and recommendations. Disaster Prev Manag 2020;29:445-55. [Crossref] [PubMed]
Cite this article as: Anning R, Cope D, Treble A, Jefferson N. Tonsillectomy: does proximity from otolaryngology care influence the intra-operative or post-operative plan? Aust J Otolaryngol 2021;4:25.


