Partial laryngeal atresia in patients with 22q11 deletion syndrome: findings and surgical outcomes
Introduction
22q11.2 deletion syndrome (22q11.2DS) is a chromosomal disorder with a multisystem set of symptoms that vary significantly in both clinical expression and severity of symptoms. Patients commonly present with congenital cardiac malformations, facial dysmorphism, palatal abnormalities and immunodeficiency (1). While different conditions, including velocardiofacial syndrome (VCFS), DiGeorge syndrome, and conotruncal anomaly have been described, they all encompass clinical manifestations associated with the same 22q11.2 genetic defect, with considerable overlap in clinical characteristics.
Children with 22q11.2DS are at increased risk of airway anomalies (66–71%) when compared with the rest of the paediatric population (1,2). Tracheomalacia, subglottic stenosis, laryngomalacia and partial laryngeal atresia are the most common airway findings and the most common symptoms are stridor, dysphonia and dysphagia.
Laryngeal atresia results from a recanalization failure of the primitive larynx between the 8th and 10th week of gestation. It may present as a thin membranous web at the glottic level, or a thick partial laryngeal atresia with subglottic extension, according to the embryological stage at which the recanalization process ceased (3). Cohen et al. proposed a staging system based on the location of the web within the larynx and the severity of airway obstruction (4). At our institution, a genetic investigation is performed in all patients with glottic webs due to the known association with 22q11.2. The surgical management of airway obstruction secondary to laryngeal atresia will vary according to the severity of the airway obstruction, as well as the patient’s comorbidities.
This study aimed to assess the outcomes of management of partial laryngeal atresia (PLA) among patients with 22q11.2DS. Common associated airway findings and related symptoms will be discussed.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-81).
Methods
This study was conducted by the Otolaryngology Head and Neck Department at Perth Children’s Hospital (PCH), the only stand-alone paediatric institution in Western Australia. An audit of patients with laryngeal atresia and a confirmed diagnosis of 22q11DS at our Institution from 2009 to 2020 was performed. Data were collected from the hospital database, identifying the diagnosis code “laryngeal atresia” and “laryngeal pathology”. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from Child and Adolescence Health Service - Surgical ServicesGEKOQI Group- Perth Children Hospital. Registration 34601. Additionally, data from the Western Australian Register of Developmental Anomalies identifying all diagnosed cases of 22q11.2 DS was obtained. Data collected included age, symptoms at presentation, associated clinical anomalies, detailed microlaryngoscopy and bronchoscopy (MLB) findings, Cohen laryngeal atresia classification, surgical technique, the need for tracheostomy, and follow-up. Children who were diagnosed with glottic webs that did not require airway surgery were excluded. Descriptive statistics were used to summarize the study population and their clinical characteristics.
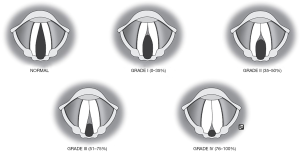
Patients underwent a clinical examination, including nasendoscopy followed by a diagnostic MLB, under general anaesthesia to confirm the suspected pathology and address potential synchronous airway abnormalities. Cohen’s classification for laryngeal atresia was used to categorise the severity of obstruction and guide the surgical plan. The Cohen classification is as follows: type I, less than 35% obstruction; type II, between 35% and 50%; type III, between 50% and 75% with subglottic extension and involvement of the anterior cricoid; and type IV, those with glottic stenosis up to 99%, with associated subglottic stenosis (4) (Figure 1). Secondary airway anomalies were also described.
All patients underwent a clinical swallow assessment by a speech pathologist. Additionally, some patients underwent a videofluoroscopy swallow study (VFSS) pre-operatively. VFSS was performed for all children after the surgical reconstruction to objectively diagnose dysphagia and assess the aspiration risk.
As part of the clinical follow-up, a diagnostic MLB was performed three months post-operatively, regardless of the patient’s symptoms. All children were regularly discussed at our Multidisciplinary Complex Airway Team meetings, including health professionals from respiratory medicine, speech pathology and gastroenterology. During hospital admission and subsequent follow-up, patients were also assessed by speech pathologists, cardiologists, general paediatricians, paediatric intensivists, anaesthetists, and geneticists.
Results
Between 2009 and 2020, according to the Western Australian Register of Developmental Anomalies, a total of 64 patients were diagnosed with 22q11DS. During the same period, 14 (16%) patients were diagnosed with laryngeal atresia at our Institution. Ten of these 14 patients with PLA were positive for 22q11.2DS on genetic testing (aged between 4 days and 17 months at diagnosis). Eight patients underwent airway surgery and they are the focus of this study. Six (85%) were full-term babies at birth, and four (50%) were male. Congenital heart disease was present in six patients (75%) and two required cardiac surgery, all had varying degrees of atrioventricular septal defects. Other common VCFS features were also observed, including craniofacial anomalies (4/8), global developmental delay (5/8), palate defects (6/8), and immunodeficiency (4/8). None of our population required immunotherapy guided by Immunological specialist opinion.
Presentation
Patients presented with a combination of stridor (75%), and dysphonia, or a weak cry (62%). After a clinical and endoscopic assessment, most patients were classified with Cohen’s type III obstruction (62.5%) (Figure 2), and three had synchronous airway anomalies, most commonly tracheomalacia (Table 1). The mean age at surgery was 13 months. Surgical intervention was tailored according to the degree and extension of laryngeal atresia, the presence of a secondary airway anomaly and any comorbidities. All surgery was performed by the senior author. All patients went to the paediatric intensive care (PICU) post-operatively.


Full table
Endoscopic treatment
Three patients with minor glottic obstruction (Cohen grade I and II) (Patients 3, 4 and 8, Table 1) aged 10 days to 17 months, underwent endoscopic division of the laryngeal web with cold steel instruments, steroid injected into the anterior glottis (1ml triamcinolone 40 mg/mL) and a silastic sheet sutured into the anterior commissure to avoid re-stenosis. These patients were extubated the following day without any complications. A planned follow-up MLB one week later was performed to remove the silastic sheet and to evaluate the need for further intervention. Endoscopic examination showed no recurrence of the laryngeal web in all 3 cases.
Laryngotracheal reconstruction
Four patients with Cohen grade III laryngeal atresia underwent laryngotracheal reconstruction (LTR) (Figure 2) (Patients 1, 2, 5, and 6, Table 1). Three children underwent a single-stage LTR with an anterior costochondral graft. One patient underwent a planned double-stage procedure with a tracheostomy and a supra-stomal stent which was removed 2 weeks post-reconstruction. At MLB at week one post-operatively, one patient had no signs of airway obstruction and was successfully extubated (Patient 1). Patient 6 had a residual anterior laryngeal web, requiring endoscopic web division, and was successfully extubated the following day. Patient 5 failed extubation secondary to granulation tissue at the level of the vocal cords and a lower respiratory tract infection. He underwent a tracheostomy to secure the airway and injection of corticosteroids into the granulation tissue. He was successfully decannulated three weeks later with no further endoscopic intervention required. Patient 2, who underwent a planned double-stage LTR, was decannulated six months post airway reconstruction.
Slide thyro-crico-tracheoplasty
One patient with Cohen grade III stenosis underwent a single-stage slide thyro-crico-tracheoplasty (5) (Patient 7, Table 1). The subglottic component of the obstruction was significant (67% obstruction) and a cricoid resection with a slide tracheoplasty (where the trachea was advanced into the laryngofissure and anastomosed to the thyroid laminae) was performed. At one week post-operatively, this patient failed extubation secondary to glottic oedema. Initially, endoscopic balloon dilatation was attempted, however, the obstruction persisted and a tracheostomy was performed. He was decannulated 6 months later. A persistent left vocal cord palsy was diagnosed as a complication of his airway reconstruction.
At the last documented endoscopy, all patients in this series were sized with an age-appropriate airway. One patient had a persistent left vocal cord palsy, as previously described. The mean post-operative follow-up period was 38.3 months (range nine to 60 months). All patients who underwent tracheostomy were successfully decannulated. No patients currently have obstructive airway symptoms.
Dysphagia
Pre-operatively dysphagia was present in 85% of the cases and a combination of thickener and flow rate altering techniques such as modified bottles and teats were implemented by the speech pathology team. Post-operative swallow assessment was undertaken in all patients. VFSS reports of five patients showed different degrees of dysphagia, including hypopharyngeal pooling of secretions, delayed clearance and risk of aspiration requiring thickened fluid diet. Two patients suffered persistent aspiration, both required Naso-gastric tube placement immediately postoperatively. One of these 2 patients required a gastrostomy due to recurrent lower respiratory tract infections. This patient had severe neurological comorbidities including intellectual disability, CP and central hypotonia
Discussion
22q11DS is reported to be the second most common chromosomal anomaly, with some advocating that prenatal investigation of this condition should be routinely performed considering the potential implications (6). Head and neck manifestations are common amongst this population, including craniofacial anomalies, palatal dysfunction, middle ear pathology, and airway obstruction (7). Currently, routine screening for this condition is not practiced, hence a heightened awareness of the diverse clinical presentations is needed.
Partial laryngeal atresia is a well-established cause of airway obstruction among children with 22q11DS. 16% of children with VFCS during the study period were diagnosed with PLA in Western Australia, much higher than the general population prevalence: 1:50,000. Therefore, a genetic assessment should be initiated once this diagnosis is made (8). A standardized endoscopic examination should including an MLB to confirm the diagnosis, precisely assess the sub-glottic extension of laryngeal atresia, the lumen size, any synchronous airway lesion, as well as palatal or laryngeal clefts.
Previous reports have described the need for airway surgery to secure the airway among patients with VCFS (9). Clive et al. detailed newborn twins who presented with severe airway obstruction secondary to type III and IV glottic stenosis requiring resuscitation and tracheostomy. They were both diagnosed with 22q11.2DS (10). To the best of our knowledge, the present study is the first report exclusively on a series of children with a diagnosis of 22q11.2DS and PLA who underwent surgery to treat laryngeal atresia. De Trey et al. reported 12 cases of laryngeal atresia, but only four had VCFS diagnosis (11). We believe our study contributes to a better understanding of the range of the airway phenotype in patients with 22q11.2DS and associated PLA as well as highlighting the importance of a multidisciplinary assessment and individualized surgical approaches and the outcomes of definitive early surgery to minimize the need for prolonged tracheostomy in these patients.
Endoscopic treatment
The primary goals for the management of congenital laryngeal webs are to establish a safe airway size, without dysphagia or dysphonia. In the paediatric population, minor laryngeal webs with a minimal degree of dysphonia may not require treatment. For those with no airway compromise, an endoscopic repair can be postponed until school age. In this series, children with type I and II glottic webs with obstructive symptoms are treated endoscopically with a cold steel technique.
Author’s technique for these cases is an endoscopic alternative for laryngeal keel placement. It is ideal for minor webs whether congenital or acquired. Tracheotomy or intubation may not be necessarily required. The aim is to secure a thin silastic sheet at the anterior commissure covering all raw mucosal surfaces. Two surgeons are usually need for this procedure. This technique involves suspending the larynx with a laryngoscope and endoscopic web division with a sickle knife. With the patient still suspended, the neck is then prepped, and a small horizontal incision is made over the thyroid cartilage. A 4.0 Prolene suture double ended suture is passed through a thin silastic sheet at 2 points aiming to secure the sheet at 2 points: 3–5 mm above and below the anterior commissure. Two IV cannulas are passed through the midline of the thyroid cartilage above and below the vocal folds until they are visible in the airway. The assistant then passes the 2 ends of the suture (with the needle removed) into the IV cannula with a laparoscopic needle holder. The suture is advance until it is visible at the end of the IV cannula in the neck incision. The cannula are then withdrawn. The suture is secured over a segment of an intravenous cannula, with multiple knots. The keel is removed 7 to 14 days later. The patient is again placed in suspension, with the neck incision being partially reopened to remove the suture securing the keel. The silastic sheet is the removed trans-orally (12).
Inflammatory tissue and restenosis are known complications post laryngeal surgery (13), therefore early re-evaluation was performed to allow intervention if granulation tissue was present and for removal of the silastic keel if placed. All patients in the present study with a diagnosis of lower grade laryngeal webs were successfully managed by the technique described above. We don’t believe that the age of the patient should be a limiting factor for the endoscopic approach. In our population study, the youngest patient was 10 days old at the time of endoscopic procedure and was successfully extubated without re-stenosis identified on follow up (as also seen in the other cases treated endoscopically).
The use of Mitomycin C(MC) as an adjuvant treatment in the airway is still debatable. The drug affects wound healing due to its anti-proliferative properties. While some series have shown benefit in using MC in laryngotracheal surgery to treat laryngeal atresia and subglottic stenosis (14), others have shown no difference (15). Based on the uncertain benefit and well described potential side effects of the drug, the senior author does not use MC.
Laryngotracheal reconstruction
Type III webs most often present with a thick, anteriorly based subglottic component, requiring open surgery for successful long term airway patency (16). To illustrate this, one of the patients with a type III laryngeal atresia was initially managed with anterior web division on day four of life. This patient experienced restenosis with persistent airway obstructive symptoms, and LTR was successfully performed months later.
All the patients with more severe airway obstruction in the present study underwent open airway reconstruction. As previously stated by Milczuk et al., the decision on the type of reconstruction for partial laryngeal atresia will depend on the type of laryngeal deformity, airway status, and individual patient factors, such as neurological and cardiac comorbidities. Patients with severe neurological and cardiac pathologies are more likely to require double-stage procedures and long term tracheostomy tube placed (13). LTR is currently the preferred option in children with severe laryngeal atresia (11). Additionally, open airway reconstruction is reported to be safe in young children and may avoid the requirement for a long-term tracheostomy (17). In our study, four patients underwent LTR with an anterior costochondral graft, and all patients had a partial resection of a wedge of the anterior cricoid cartilage. A posterior graft is usually not needed when the inter-arytenoid distancing is preserved and the patient does not present with posterior glottic obstruction.
Severe webs, with a combined cartilaginous subglottic stenosis and cricoid deformity, will require associated resection of the excess cricoid cartilage. For these cases, LTR with an anterior and posterior graft may be an option (16).
However, in this series, a slide thyro-crico-tracheoplasty was performed in one patient with Cohen grade 3 stenosis with significant subglottic stenosis as well. Cricotracheal resection is recommended for patients with high-grade subglottic stenosis and evidence shows that these patients are less likely to require a second open procedure to achieve decannulation (18) In concordance, the only patient who which we performed thyro-crico-tracheoplasty, who presented with a severe cricoid deformity with high-grade type III subglottic stenosis was successfully decannulated 6 months post airway reconstruction and did not require a second open surgical procedure.
Compared with previous reports (11,13), our population was significantly younger (mean age 13 months), and no patient required tracheostomy before LTR, suggesting that open airway reconstruction may be a safe option for young patients with 22q11.2DS laryngeal atresia to avoid the complications of a long-term tracheostomy.
Tracheostomy
Previous reports have described the need for tracheostomy in the management of laryngeal atresia patients. A 12-year review of children with severe laryngeal atresia by De Trey et al. reported that 86% of cases required tracheostomy before airway reconstruction (11). In contrast, none of our patients had a tracheostomy before airway reconstruction, regardless of the severity of glottic obstruction. However, it is important to highlight that none of our patients had the most severe degree of obstruction—Cohen grade IV.
Tracheostomy might be required during peri and post-operative periods as a planned double stage procedure or as a complication of LTR. Obstruction secondary to granulation tissue and oedema is a known complication after LTR (19). Two of our patients (Patients 5 and 7) required an unplanned tracheostomy post-reconstruction due to airway obstruction secondary to granulation tissue and oedema. Both were decannulated with no evidence of restenosis. One patient had a planned double-stage procedure due to co-morbidity and was decannulated six months later. In concordance with previous reports (11) that decannulation can be achieved in most cases, all our patients were decannulated post airway reconstruction.
Dysphonia
Dysphonia is a common symptom among patients with VCFS (13) and five of our case series were noted to be dysphonic on presentation. Small anterior laryngeal webs with no associated significant respiratory or voice problems may initially be misdiagnosed and may present later in life during the investigation of dyspnoea or with dysphonia (20). Additionally, the presence of a secondary airway anomaly may lead to misdiagnosis. Patient 3 in the current study was initially diagnosed with laryngomalacia and underwent a supraglottoplasty by a different otolaryngologist. However, it was only at the age of 17 months, nearly a year following the supraglottoplasty, that the laryngeal web was diagnosed during the investigation of persistent dysphonia and stridor. This patient successfully underwent endoscopic web division with a good outcome. The other patients presented primarily with airway symptoms, but three out of five were also noted to be dysphonic.
A limitation of this study is the retrospective nature of the analysis. Additionally, while subjective reporting of dysphonia was routinely done, the absence of a validated, objective tool for voice assessment was also a limitation. Also, the young age of the patients at the time of the diagnosis made voice evaluation very challenging as many were pre-verbal.
Dysphagia
Dysphagia is frequently present in children with 22q11.2DS. Animal studies have shown the association between craniofacial development disorders and cranial neural circuit disorders leading to oropharyngeal dysfunction and increased aspiration risk, regardless of surgical intervention (21). Additionally, in 2000, Eicher et al. also reported that children with 22q11.2DS have a pattern of feeding difficulty independent of palatal or cardiac involvement. They highlighted the importance of having a contrasted swallow study to objectively evaluate dysphagia in these patients and to better address aspiration risk (22). Pulmonary aspiration is a key symptom to address in this population and that could result from oropharyngeal dysphagia as well as secondary to the laryngeal anomaly. Aspiration increases the risk of lower respiratory tract infection and therefore post-operative complications including long term need for ventilatory support and delayed decannulation. Consistent with this, all of our patients showed evidence of some degree of oropharyngeal dysphagia and increased pulmonary aspiration risk, requiring intervention with thickened fluids during the post-operative period. Only one patient (Patient 7) required a long-term nasogastric tube, eventually, a gastrostomy tube placed and fundoplication performed, due to recurrent aspiration pneumonia associated with severe gastroesophageal reflux disease. This patient was also diagnosed with central hypotonia and cerebral palsy, which also contributed to oropharyngeal incoordination.
Associated pathology
As previously described by Sacca et al., synchronous airway findings are common among children with laryngeal atresia and VCFS (2). In our study, subglottic stenosis was presented in patients with severe partial laryngeal atresia—Cohen grade III, where the glottic obstruction extended into the subglottis (33%), Tracheomalacia was diagnosed in three cases (33%) (Table 1), and one had associated laryngomalacia. Congenital heart disease, including conotruncal defects, conoventricular and/or atrial septal defects, and aortic anomalies were present in 60–80% of patients with 22q11.2 DS (23). Consistent with the literature, 75% of our patients had a diagnosis of congenital heart disease, mostly atrioventricular septal defects. Also, as previously described by Ford et al., otolaryngological findings are relatively common in children with VCFS, and these must be recognized (24). In that study, otitis media was present in 88% of the patients, and 92% of those who underwent nasendoscopy had some degree of palatal dysfunction. In the current study, 75% had palate defects, whereas 50% experienced conductive hearing loss secondary to middle ear effusion.
Conclusions
Partial laryngeal atresia is a feature of 22q11.2DS and a careful endoscopic airway evaluation should be mandatory in cases of stridor. Dysphonia and dysphagia are common in this group. Children with mild laryngeal obstruction may be successfully treated with an endoscopic procedure, however, patients with severe obstruction will require open airway reconstruction. LTR should be considered in these patients at a young age to avoid complications related to long-term tracheostomy.
Acknowledgments
The authors would like to acknowledge and thank Sophia Quick for her excellent diagram (figure 1) depicting the Cohen Classification of laryngeal atresia. Funding: None.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-81
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-20-81
Peer Review File: Available at http://dx.doi.org/10.21037/ajo-20-81
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-81). SV serves as an unpaid editorial board member of the Australian Journal of Otolaryngology from Jan 2019 to Dec 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from Child and Adolescence Health Service - Surgical ServicesGEKOQI Group- Perth Children Hospital. Registration 34601.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jones JW, Tracy M, Perryman M, et al. Airway Anomalies in Patients With 22q11.2 Deletion Syndrome: A 5-Year Review. Ann Otol Rhinol Laryngol 2018;127:384-9. [Crossref] [PubMed]
- Sacca R, Zur KB, Crowley TB, et al. Association of airway abnormalities with 22q11.2 deletion syndrome. Int J Pediatr Otorhinolaryngol 2017;96:11-4. [Crossref] [PubMed]
- Moore KL, Persaud TVN. The developing human: clinically oriented embryology. In: 5TH ed. Philadelphia; 1993.
- Cohen SR. Congenital glottic webs in children. A retrospective review of 51 patients. Ann Otol Rhinol Laryngol Suppl 1985;121:2-16. [Crossref] [PubMed]
- Kim SM, Han SJ, Choi HS, et al. Slide Thyrocricotracheoplasty: A Novel Surgical Technique for Congenital Laryngeal Atresia. Pediatr Surg Int 2008;24:383-6. [Crossref] [PubMed]
- Grati FR, Molina Gomes D, Ferreira JCPB, et al. Prevalence of recurrent pathogenic microdeletions and microduplications in over 9500 pregnancies: Prevalence of recurrent pathogenic copy number in prenatal population. Prenat Diagn 2015;35:801-9. [Crossref] [PubMed]
- Grasso F, Cirillo E, Quaremba G, et al. Otolaryngological features in a cohort of patients affected with 22q11.2 deletion syndrome: A monocentric survey. Am J Med Genet A 2018;176:2128-34. [Crossref] [PubMed]
- Miyamoto RC, Cotton RT, Rope AF, et al. Association of Anterior Glottic Webs with Velocardiofacial Syndrome (Chromosome 22q11.2 Deletion). Otolaryngol Head Neck Surg 2004;130:415-7. [Crossref] [PubMed]
- Fokstuen S, Bottani A, Medeiros PF, et al. Laryngeal atresia type III (glottic web) with 22q11.2 microdeletion: report of three patients. Am J Med Genet 1997;70:130-3. [Crossref] [PubMed]
- Clive B, Corsten G, Penney LS, et al. Severe laryngeal stenosis in newly born twins with 22q11.2 deletion syndrome: A case report. J Neonatal Perinatal Med 2016;9:223-6. [Crossref] [PubMed]
- de Trey LA, Lambercy K, Monnier P, et al. Management of severe congenital laryngeal webs – a 12 year review. Int J Pediatr Otorhinolaryngol 2016;86:82-6. [Crossref] [PubMed]
- Kuo IC, Rutter M. Surgical Management of Anterior Glottic Webs. Front Pediatr 2020;8:555040 [Crossref] [PubMed]
- Milczuk HA, Smith JD, Everts EC. Congenital laryngeal webs: surgical management and clinical embryology. Int J Pediatr Otorhinolaryngol 2000;52:1-9. [Crossref] [PubMed]
- Amir M, Youssef T. Congenital glottic web: Management and anatomical observation: Congenital anterior glottic web. Clin Respir J 2010;4:202-7. [Crossref] [PubMed]
- Shvidler J, Bothwell NE, Cable B. Refining indications for the use of mitomycin C using a randomized controlled trial with an animal model. Otolaryngol Head Neck Surg 2007;136:653-7. [Crossref] [PubMed]
- Monnier P. Pediatric Airway Surgery, Management of laryngeal webs [Internet]. Springer; 2011. DOI:
10.1007/978-3-642-13535-4 10.1007/978-3-642-13535-4 - Bottero S, Peradotto F, Roma R, et al. Laryngotracheal reconstruction in glottic-subglottic stenosis associated with DiGeorge syndrome in a four and a half-month-old infant. Acta Otorhinolaryngol Ital 2015;35:53-7. [PubMed]
- Hartley BEJ, Cotton RT. Paediatric airway stenosis: laryngotracheal reconstruction or cricotracheal resection? Clin Otolaryngol Allied Sci 2000;25:342-9. [Crossref] [PubMed]
- Bitar MA, Al Barazi R, Barakeh R. Airway reconstruction: review of an approach to the advanced-stage laryngotracheal stenosis. Braz J Otorhinolaryngol 2017;83:299-312. [Crossref] [PubMed]
- Parelkar KA, Thorawade VP, Shah KA, et al. A Misdiagnosed Laryngeal Web: Treated with an Innovative Self-Made Keel. J Clin Diagn Res 2017;11:MD04-6. [Crossref] [PubMed]
- LaMantia A-S, Moody SA, Maynard TM, et al. Hard to swallow: Developmental biological insights into pediatric dysphagia. Dev Biol 2016;409:329-42. [Crossref] [PubMed]
- Eicher PS, McDonald-McGinn DM, Fox CA, et al. Dysphagia in children with a 22q11.2 deletion: Unusual pattern found on modified barium swallow. J Pediatr 2000;137:158-64. [Crossref] [PubMed]
- Goldmuntz E. 22q11.2 deletion syndrome and congenital heart disease. Am J Med Genet C Semin Med Genet 2020;184:64-72. [Crossref] [PubMed]
- Ford LC, Sulprizio SL, Rasgon BM. Otolaryngological Manifestations of Velocardiofacial Syndrome: A Retrospective Review of 35 Patients. Laryngoscope 2000;110:362-7. [Crossref] [PubMed]
Cite this article as: Smith AL, Herbert H, Uwiera T, Vijayasekaran S. Partial laryngeal atresia in patients with 22q11 deletion syndrome: findings and surgical outcomes. Aust J Otolaryngol 2021;4:26.