
Stylohyoid pain syndrome—an Australian case series and review
Introduction
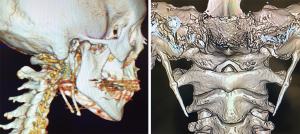
Stylohyoid pain syndrome was first formally described by Watt Eagle in 1937, although anatomists have recognised the structural abnormality of an elongated styloid process for over 300 years. Eagle’s syndrome describes a constellation of cervicopharyngeal symptoms with radiological evidence of an elongated styloid bone or calcification of the stylohyoid ligament. Patients may present with throat, neck or neuropathic pain on head turning, dysphagia or cerebral ischaemic-like symptoms. In symptomatic patients, this may be due to direct compression of nearby structures or insertion tendonitis and there are two described ‘syndromes’ of symptoms. The more common, ‘classic syndrome’ describes pain due to compression of structures of the pharynx and hypopharynx, in particular the glossopharyngeal nerve. The ‘carotid artery syndrome’ is a constellation of cerebrovascular and neurological symptoms due to compression of either the internal or external carotid artery (1). The Langais system of classification from 1986 is used to define the anatomy of the styloid process, with Type I referring to an uninterrupted, elongated styloid process; Type II indicating a pseudo-segmented styloid process linked to a mineralised stylohyoid ligament; whereas Type III is a segmented styloid process formed by short, discontinuous portions of the styloid process (2). Clinical examination and radiology are performed with the aim to exclude other pathologies, such as otitis media, trigeminal or glossopharyngeal neuralgia, masticatory muscle disorders, dental or salivary gland disease and head and neck cancer. MRI is essential in excluding occult soft tissue pathologies. Head and neck CT with 1 mm slices and 3D reconstruction is the imaging modality of choice in Eagle’s syndrome in identifying the extent and orientation of the stylohyoid ligament ossification (3,4).
Styloidectomy can be performed via a trans-oral or trans-cervical approach but there are few large studies comparing the risks of each method. We outline a single operator’s series of styloidectomy and perform a review of the literature with the view of determining the associated risks of each surgical approach. We present the following case series in accordance with the PROCESS reporting checklist (available at https://dx.doi.org/10.21037/ajo-21-5).
Methods
A retrospective review was undertaken of a single consultant otolaryngologist’s consecutive cases of styloidectomy in a regional centre over a 15-year period from 2005 to 2019. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from St John of God Health Care Human Research Ethics Committee (reference 1830) and a waiver of consent was granted by the ethics committee. Patients considered appropriate for inclusion in this case series were any adult patient undergoing styloidectomy for management of stylohyoid pain syndrome at either a local public or private hospital. All included patients underwent elective styloidectomy under general anaesthetic, either via the standard trans-oral or trans-cervical approach as described below. Patients were followed up for three months post-operatively and their symptoms assessed subjectively via clinician-assessed and patient reported pain levels or neurovascular symptoms. Three months was considered a minimum adequate time to assess the efficacy of the surgery (resolution of pain) and the development of any complications. There was no missing data or patients lost to follow up.
Ovid Medline was searched for “Eagle’s syndrome” with parameters limited to ‘English language’ and publication between 1937–2020. Case series of patients treated surgically via either the trans-oral or trans-cervical approach were included. Articles considered for inclusion could examine patients of any age or gender. Case reports of one patient or studies discussing non-surgical management or novel techniques were excluded. Collected data included the age and sex of the patients, history of tonsillectomy, indications for surgery, surgical approach, surgeon performing surgery, outcomes and complications.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS, IBM Corporation., Chicago, IL, USA) software version 25. Chi-square test with a P value of <0.05 was used to indicate significance and odds ratio was determined using the Mantel-Haenszel method. Post-operative issues considered to be complications included difficult trans-oral access requiring abandonment or conversion to trans-cervical approach; significant post-operative pain, trismus or respiratory distress; and nerve palsies or paraesthesias. Post-operative issues such as subcutaneous emphysema or oedema that did not affect discharge timeframe were not considered complications.
Trans-oral approach
This method was first described by Eagle in 1937, requiring tonsillectomy if not previously performed and relies on palpation of the styloid process via the tonsillar fossa (1). The airway is managed with either an oral endotracheal tube or laryngeal mask. The senior author performs styloidectomy via a 1 cm incision in the tonsillar bed. Following denudement of its muscular and ligamentous attachments, an incision through the periosteum is made and a hypophysis ring curette is utilised to fracture the styloid process close to the base.
Trans-cervical approach
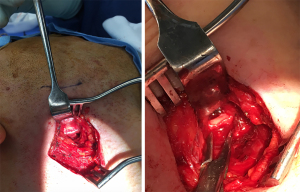
This approach was first described by Loeser and Cardwell in 1942 (5) and is the senior author’s preferred method of styloidectomy. After intubation, positioning with a shoulder roll, neck hyperextension and placement of a facial nerve integrity monitor (NIM), a high oblique neck crease incision or Risdon approach is made and subplatysmal flaps raised. The superficial layer of deep cervical fascia is incised along the anterior border of sternocleidomastoid and continued to the posterior body of digastric. The dissection is continued into the parapharyngeal space to gain exposure. Subsequently, the styloid process is palpated and its location confirmed. Sub-periosteal dissection is performed to reflect the periosteum and muscular and ligamentous attachments. Rogeur forceps are utilised to fracture the styloid process close to the base (see Figures 1 and 2).
Results
Patient information
During the review period, 19 patients required styloidectomy for Eagle’s syndrome. The majority of patients were male (14, 73.7%), while a minority were female (five, 26.3%). The age of the patients ranged from 38 to 61 years of age. All 19 patients suffered from pain and one (5.3%) suffered from neurovascular symptoms, which consisted of syncope on turning of the head, speech alteration and vertigo. Nine of the patients (47.4%) had trialled treatment for temporo-mandibular joint dysfunction and three (15.8%) had previously undergone tonsillectomy.
Diagnosis
All patients were referred to the surgeon with the diagnosis already suspected by either the referring practitioner or the patient themselves. Eagle’s syndrome is primarily a diagnosis of exclusion, with the main positive clinical finding being elicitation of pain on palpation of the styloid process in the tonsillar fossa. In order to exclude other pathologies, all patients underwent the routine pre-operative workup, including recognition of any dental disease via clinic examination and orthopantomogram (OPG) and flexible nasendoscopy and magnetic resonance imaging (MRI) to exclude an occult skull base or submucosal oropharyngeal lesions. Computered tomography with three-dimensional reconstruction (3D-CT) was utilised as a diagnostic adjunct to determine styloid process length (see Figure 3). All patients had bilateral styloid process elongation over 25 mm. Five patients (26.3%) had symptoms isolated to the side with the radiologically shorter (but still elongated) styloid process and, given the frequency of bilateral elongation, the decision to operate was always based on lateralising symptoms.
Management and outcomes
Styloidectomy was performed via the trans-cervical approach in 16 patients (84.2%) while three patients (15.8%) underwent trans-oral approach. Two of the patients undergoing trans-oral approach had previously undergone tonsillectomy and the other required tonsillectomy at the time of surgery. One of these cases was abandoned due to inability to palpate the styloid process trans-orally and this patient subsequently underwent styloidectomy via trans-cervical approach. Two patients (10.5%) required bilateral surgery. With regards to post-operative complications, two patients suffered from temporary greater auricular nerve hypoaesthesia but there were no long-term sequelae. All patients were followed up at three months and questioned about their perception of change in symptomatology. Sixteen patients (84.2%) reported complete resolution of pain, globus or neurovascular symptoms while three patients (15.8%) had ongoing symptoms despite styloidectomy.
Literature review
Twenty-nine studies were included with a total of 401 patients undergoing surgical management for Eagle’s syndrome (see Table 1). The patients ranged in age from 17 to 78 years old. There was a female predominance, with 270 females (67.3%) compared to 115 males (28.9%), while the sex was not determinable in 16 cases; 212 (52.9%) patients had previously undergone tonsillectomy while 56 (14%) had no history of tonsillectomy (in 133 cases, prior tonsillectomy status could not be determined). In the great majority of patients, the indication for surgery was pain, dysphagia and/or globus sensation (397 patients, 99%). Four patients (1%) presented with carotid artery syndrome.
Table 1
| Investigator | Year | Country | Surgical cases | Approach | ||||
|---|---|---|---|---|---|---|---|---|
| Trans-cervical | Trans-oral | |||||||
| N | Complications | N | Complications | |||||
| Eagle (1) | 1937 | USA | 2 | 2 | ||||
| Eagle (6) | 1949 | USA | 2 | 2 | 0 | |||
| Moffat (7) | 1977 | UK | 3 | 3 | 1: transient marginal nerve weakness | |||
| Strauss (8) | 1985 | Israel | 8 | 2 | 6 | 0 | ||
| Chase (9) | 1986 | Sweden | 2 | 1 | 0 | 1 | 1: difficult access | |
| Fini (10) | 2000 | Italy | 11 | 11 | 0 | |||
| Diamond (11) | 2001 | Canada | 4 | 4 | 3: greater auricular nerve paraesthesia | |||
| Prasad (12) | 2002 | India | 58 | 58 | 0 | |||
| Buono (13) | 2005 | Italy | 5 | 5 | 0 | |||
| Beder (14) | 2005 | Turkey | 19 | 19 | 0 | |||
| Zhibin (15) | 2006 | China | 9 | 9 | 0 | |||
| Nayak (16) | 2007 | India | 34 | 34 | 6: difficult access | |||
| Martin (17) | 2008 | USA | 5 | 5 | 2: transient marginal nerve weakness | |||
| Ceylan (18) | 2008 | Turkey | 61 | 61 | 2: transient marginal nerve weakness | |||
| Chrcanovic (19) | 2009 | Brazil | 5 | 5 | 1: post-operative trismus, pain, respiratory distress | |||
| Mohanty (3) | 2009 | India | 28 | 1* | 0 | 28 | 1: difficult access | |
| Peng (20) | 2011 | China | 22 | 22 | 0 | |||
| Naik (21) | 2011 | India | 15 | 15 | 0 | |||
| Müderris (22) | 2014 | Turkey | 8 | 4 | 1: transient marginal nerve weakness | 4 | 0 | |
| Scheller (23) | 2014 | Germany | 6 | 6 | 0 | |||
| Torres (24) | 2014 | Colombia | 11 | 0 | 11** | 0 | ||
| Kiralj (25) | 2015 | Serbia | 2 | 1 | 0 | 1 | 0 | |
| Kumai (26) | 2016 | Japan | 7 | 7 | 0 | |||
| Jalisi (27) | 2017 | Saudi Arabia | 6 | 3 | 0 | 3 | 1: transient lingual nerve hypoaesthesia | |
| Pigache (4) | 2018 | France | 2 | 2 | 0 | |||
| Malik (28) | 2018 | India | 9 | 9 | 0 | |||
| Waters (29) | 2019 | USA | 32 | 31 | 4: temporary weakness of marginal mandibular nerve in 2, hypoglossal nerve in 2 | 1 | ||
| Hajare (30) | 2019 | India | 10 | 10 | 0 | |||
| Czako (31) | 2020 | Poland | 15 | 14 | 1: temporary marginal mandibular nerve paresis | 1 | ||
| Total | 401 | 159 | 14 | 242 | 10 | |||
*, one patient underwent combined trans-oral and trans-cervical approach due to difficult access. **, tonsil-sparing trans-oral approach.
Overall, the trans-oral approach was preferred, being employed in 242 (60.4%) cases, while the other 159 (39.7%) underwent trans-cervical access. Most study authors had a preference with regards to surgical approach, with 25 studies utilising one approach more frequently. Sixteen study authors favoured the trans-oral approach, while nine preferred trans-cervical access. Seventy-nine (19.7%) of the studies were conducted by oromaxillofacial (OMFS) units, while the other 322 (80.3%) were written by otolaryngologists. Assuming that the same unit who conducted the studies also performed the surgeries, there was a statistically significant difference in surgical approaches-otolaryngologists performed trans-oral surgery in 66.8% of their cases, while OMFS performed trans-oral surgery in 34.2% (P<0.001).
Symptoms were relieved in 354 (88.3%) and partially improved in 30 (7.5%) cases. There was no change in symptoms in the remaining 17 cases (4.2%). There was no difference in success rates between trans-oral versus trans-cervical approach (88.9% vs. 87.4%, P=0.35). Complications occurred in 24 cases: 14 in the trans-cervical group, an incidence of 8.8% of surgeries; and 10 in the trans-oral group, occurring in 4.1% of cases (P=0.054). The odds ratio for a complication in a patient undergoing trans-cervical compared to trans-oral access was 2.24 (95% CI: 0.97–5.18, P=0.06). The trans-oral approach complications included difficult access in eight cases, requiring conversion to trans-cervical approach in one case; significant post-operative trismus, pain and respiratory distress in one case and transient lingual nerve paraesthesia in one patient. There were six cases of self-resolving subcutaneous emphysema, but we considered this to be an expected post-operative finding rather than a complication. Those complications related to open trans-cervical approach included eight cases of transient marginal nerve paresis, two cases of transient hypoglossal nerve paresis and three cases of greater auricular nerve paraesthesia.
Discussion
The cause of symptoms in cases of Eagle’s syndrome may be difficult to ascertain, particularly given that mineralisation of the stylohyoid complex is not uncommon, and many patients may be asymptomatic. According to Eagle, the styloid process is elongated in up to 4% of people but only 4% of subjects are symptomatic (6). The anatomical abnormalities of the styloid process or stylohyoid ligament that contribute to patient symptoms include a styloid process longer than 25 mm; stylohyoid or stylomandibular ligament ossification of more than 30 mm; and orientation and position of the styloid process, in particular angulation and proximity to the first cervical vertebral transverse process. The aetiology of styloid process or ligament ossification is unclear but may be related to trauma and fibrosis as a result of tonsillectomy or other pharyngeal surgery, degeneration or congenital elongation due to persistent vestigial cartilage (5,6). Similarly, the cause of resultant symptoms is also subject to debate, with theories including traumatic styloid fracture and subsequent granulation formation placing pressure on surrounding structures, compression of neural structures (glossopharyngeal, trigeminal or chorda tympani), insertion tendonitis due to degenerative and inflammatory changes, irritation of the pharyngeal mucosa and impingement of the carotid vessels and sympathetic chain (7).
Our case series of 19 patients with Eagle’s syndrome treated surgically represents a large cohort. Although the literature suggests that there is a predominance in female patients and the syndrome is most common in the 30–50-year-old age range, our study’s patients were mostly male. Patient symptoms are frequently bilateral, with two of our patients requiring bilateral styloidectomy. The majority of our patients suffered from the ‘classic syndrome symptom cluster,’ although one patient experienced the ‘carotid artery syndrome’, presenting with a constellation of cerebrovascular and neurological symptoms due to compression of the internal carotid artery. The diagnosis of Eagle’s syndrome in our series was based on suggestive symptoms and pain on palpation of the styloid process, both intraorally and externally. Reduction of pain on lignocaine infiltration can be a useful test for prediction of the results of styloidectomy (32) but was not performed in this series of patients because it was felt not to help discriminate from other mylohyoid pain syndromes.
Several treatments have been described for Eagle’s syndrome, including non-surgical treatment, styloidotomy and styloidectomy. Most authors agree that styloidectomy is the most effective treatment as medical treatment (including anti-inflammatory medications, neuromodulators, mandibular rest, soft diet, steroid and local anaesthetic injection or transpharyngeal styloid manipulation) usually only provides temporary relief (3,4,9,27,33). Styloidectomy can be performed via a trans-oral or trans-cervical approach with comparable results (22). There is minimal published data directly comparing the two approaches, hence, a review on the published case series has been performed. The trans-oral approach predominated but there was no significant difference between the two methods with regards to outcomes or complications. Most study authors had a preference with regards to surgical approach—sixteen study authors favoured the trans-oral approach, while nine preferred trans-cervical access.
The trans-oral approach avoids an external incision, is a shorter procedure and can be done under local anaesthetic. However, it relies on the ability to palpate the styloid tip; concurrent tonsillectomy has associated risks of post-operative haemorrhage; and the possibility of neurological and infective complications or abandonment of procedure. Difficult access can be exacerbated by a laterally placed styloid, contraction of the stylohyoid muscle and a deeper calcified segment (3). The trans-cervical approach allows for greater surgical exposure and total styloidectomy to eliminate the possibility that ongoing symptoms are due to residual stump. However, it has attendant risks such as scarring, internal carotid artery thrombosis and subcutaneous emphysema (33). In our review of the literature, trans-cervical approach not was associated with a significantly increased rate of complications compared to the trans-oral approach. There are a number of suggested reasons why the trans-oral route is preferred in the literature. The number appears to be strongly influenced by the six studies from India, which account for 63.6% of the trans-oral surgeries in the literature. The predilection for this surgical approach in the Indian studies may be related to the risk of keloid scarring and the cephalometrics of this patient population (34). The majority of the surgeries were conducted by otolaryngologists, who may be more comfortable operating through the tonsillar fossa, compared to OMFS, and patients in otolaryngology-conducted case series were more likely to undergo surgery via the trans-oral route. At least 52.9% of patients in the literature had a history of tonsillectomy, which affords trans-oral access and ability to palpate the styloid tip in the tonsillar fossa. In recent years, novel approaches to styloidectomy have been discussed in the literature, including trans-oral tonsil-sparing styloidectomy (35) and intra-operative navigation equipment (36).
In our cohort of 19 patients, the trans-cervical approach was preferred over the trans-oral approach because the complications associated with trans-oral access (e.g., difficult access, conversion, post-operative trismus and respiratory distress) could be considered more serious than the temporary neuropraxias associated with the trans-cervical approach. In the hands of an experienced skull base surgeon and with use of the NIM, the rate of motor neuropraxia in our series was zero. The rate of prior tonsillectomy in our series (15.8%) was much lower than in the general literature, making trans-oral access and palpation of the styloid tip more difficult. Via the trans-cervical approach, all styloid tips can be palpated and clearly visualised, thereby mitigating the risk of parapharyngeal infection and neurovascular injury. Great auricular nerve hypoaesthesia can be minimised through identification and careful retraction.
Overall, there was a low risk of complications among our patient cohort and 84.2% had relief of symptoms. While this is one of the largest and the only Australian case series in the literature, it is limited by being retrospective and non-randomised and also due to single-operator selection bias. A randomised trial comparing the outcomes and complication rates of trans-oral versus trans-cervical approach would contribute to the international literature.
Conclusions
To the authors’ knowledge, we present the only Australian case series of surgically managed Eagle’s syndrome and demonstrate that styloidectomy is a safe procedure that can provide symptomatic relief to a majority of patients. Although trans-oral surgery is preferred in the literature, there is no significant difference in complications and the authors of this paper prefer the trans-cervical approach, with our series of 19 patients demonstrating a low rate of associated complications. In appropriately selected patients, styloidectomy can be a beneficial procedure for the management of an otherwise potentially debilitating condition.
Acknowledgments
The authors of this article would like to thank the patients whose data contributed to this study.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PROCESS reporting checklist. Available at https://dx.doi.org/10.21037/ajo-21-5
Data Sharing Statement: Available at https://dx.doi.org/10.21037/ajo-21-5
Peer Review File: Available at https://dx.doi.org/10.21037/ajo-21-5
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/ajo-21-5). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from St John of God Health Care Human Research Ethics Committee (reference 1830) and a waiver of consent was granted by the ethics committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eagle WW. Elongated Styloid Process: Report of Two Cases. Arch Otolaryngol 1937;25:584-7. [Crossref] [PubMed]
- Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized stylohyoid ligament complex: a proposed classification and report of a case of Eagle's syndrome. Oral Surg Oral Med Oral Pathol 1986;61:527-32. [Crossref] [PubMed]
- Mohanty S, Thirumaran NS, Gopinath M, et al. Significance of styloidectomy in Eagle's syndrome: an analysis. Indian J Otolaryngol Head Neck Surg 2009;61:262-5. [Crossref] [PubMed]
- Pigache P, Fontaine C, Ferri J, et al. Transcervical styloidectomy in Eagle's syndrome. Eur Ann Otorhinolaryngol Head Neck Dis 2018;135:433-6. [Crossref] [PubMed]
- Loeser LH, Cardwell EP. Elongated styloid process: A cause of glossopharyngeal neuralgia. Arch Otolaryngol 1942;36:198-203. [Crossref]
- Eagle WW. Symptomatic elongated styloid process; report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol 1949;49:490-503. [Crossref] [PubMed]
- Moffat DA, Ramsden RT, Shaw HJ. The styloid process syndrome: aetiological factors and surgical management. J Laryngol Otol 1977;91:279-94. [Crossref] [PubMed]
- Strauss M, Zohar Y, Laurian N. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope 1985;95:976-9. [Crossref] [PubMed]
- Chase DC, Zarmen A, Bigelow WC, et al. Eagle's syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol 1986;62:625-9. [Crossref] [PubMed]
- Fini G, Gasparini G, Filippini F, et al. The long styloid process syndrome or Eagle's syndrome. J Craniomaxillofac Surg 2000;28:123-7. [Crossref] [PubMed]
- Diamond LH, Cottrell DA, Hunter MJ, et al. Eagle's syndrome: a report of 4 patients treated using a modified extraoral approach. J Oral Maxillofac Surg 2001;59:1420-6. [Crossref] [PubMed]
- Prasad KC, Kamath MP, Reddy KJ, et al. Elongated styloid process (Eagle's syndrome): a clinical study. J Oral Maxillofac Surg 2002;60:171-5. [Crossref] [PubMed]
- Buono U, Mangone GM, Michelotti A, et al. Surgical approach to the stylohyoid process in Eagle's syndrome. J Oral Maxillofac Surg 2005;63:714-6. [Crossref] [PubMed]
- Beder E, Ozgursoy OB, Karatayli Ozgursoy S. Current diagnosis and transoral surgical treatment of Eagle's syndrome. J Oral Maxillofac Surg 2005;63:1742-5. [Crossref] [PubMed]
- Zhibin W, Min J. Design and clinical application of the 'styloidectome' styloid process cutter. J Laryngol Otol 2006;120:753-8. [Crossref] [PubMed]
- Nayak DR, Pujary K, Aggarwal M, et al. Role of three-dimensional computed tomography reconstruction in the management of elongated styloid process: a preliminary study. J Laryngol Otol 2007;121:349-53. [Crossref] [PubMed]
- Martin TJ, Friedland DR, Merati AL. Transcervical resection of the styloid process in Eagle syndrome. Ear Nose Throat J 2008;87:399-401. [Crossref] [PubMed]
- Ceylan A, Köybaşioğlu A, Celenk F, et al. Surgical treatment of elongated styloid process: experience of 61 cases. Skull Base 2008;18:289-95. [Crossref] [PubMed]
- Chrcanovic BR, Custódio AL, de Oliveira DR. An intraoral surgical approach to the styloid process in Eagle's syndrome. Oral Maxillofac Surg 2009;13:145-51. [Crossref] [PubMed]
- Peng GG, Chen WL, Wu JW, et al. Eagle's syndrome treated with dissection of the styloid process via an extraoral approach combined with antidepressants. Chin J Dent Res 2011;14:37-40. [PubMed]
- Naik SM, Naik SS. Tonsillo-Styloidectomy for Eagle's Syndrome: A Review of 15 Cases in KVG Medical College Sullia. Oman Med J 2011;26:122-6. [Crossref] [PubMed]
- Müderris T, Bercin S, Sevil E, et al. Surgical management of elongated styloid process: intraoral or transcervical? Eur Arch Otorhinolaryngol 2014;271:1709-13. [Crossref] [PubMed]
- Scheller K, Eckert AW, Scheller C. Transoral, retromolar, para-tonsillar approach to the styloid process in 6 patients with Eagle's syndrome. Med Oral Patol Oral Cir Bucal 2014;19:e61-6. [Crossref] [PubMed]
- Torres AC, Guerrero JS, Silva HC. A modified transoral approach for carotid artery type Eagle syndrome: technique and outcomes. Ann Otol Rhinol Laryngol 2014;123:831-4. [Crossref] [PubMed]
- Kiralj A, Illić M, Pejaković B, et al. Eagle's syndrome - A report of two cases. Vojnosanit Pregl 2015;72:458-62. [Crossref] [PubMed]
- Kumai Y, Hamasaki T, Yumoto E. Surgical management of Eagle's syndrome: an approach to shooting craniofacial pain. Eur Arch Otorhinolaryngol 2016;273:3421-7. [Crossref] [PubMed]
- Jalisi S, Jamal BT, Grillone GA. Surgical Management of Long-standing Eagle's Syndrome. Ann Maxillofac Surg 2017;7:232-6. [Crossref] [PubMed]
- Malik JN, Monga S, Sharma AP, et al. Stylalgia Revisited: Clinical Profile and Management. Iran J Otorhinolaryngol 2018;30:335-40. [PubMed]
- Waters CM, Ho S, Luginbuhl A, et al. Surgical Management of Stylohyoid Pain (Eagle's) Syndrome: A 5-Year Experience. Ann Otol Rhinol Laryngol 2019;128:220-6. [Crossref] [PubMed]
- Hajare P, Puneeth Nayak S, Deepthi B, et al. Eagle's Syndrome: An Underdiagnosed Condition-Case Series in a Tertiary Care Hospital. Indian J Otolaryngol Head Neck Surg 2019;71:949-52. [Crossref] [PubMed]
- Czako L, Simko K, Thurzo A, et al. The Syndrome of Elongated Styloid Process, the Eagle's Syndrome-From Anatomical, Evolutionary and Embryological Backgrounds to 3D Printing and Personalized Surgery Planning. Report of Five Cases. Medicina (Kaunas) 2020;56:458. [Crossref] [PubMed]
- Singhania AA, Chauhan NV, George A, et al. Lidocine Infiltration Test: An Useful Test in the Prediction of Results of Styloidectomy for Eagle's Syndrome. Indian J Otolaryngol Head Neck Surg 2013;65:20-3. [Crossref] [PubMed]
- Williams JV, McKearney RM, Revington PJ. Eagle's syndrome: a novel surgical approach to the styloid process using a preauricular incision. J Oral Maxillofac Surg 2011;69:1617-22. [Crossref] [PubMed]
- Janakiraman M, Ramakrishnan KM, Jayaraman V, et al. Etiology and management of ear lobule keloid in South India. Plast Reconstr Surg 2007;119:435-7. [Crossref] [PubMed]
- Cai Y, Gu W, Wang J. Evaluation of postoperative pain after tonsil-sparing styloidectomy. Eur Arch Otorhinolaryngol 2020;277:2011-5. [Crossref] [PubMed]
- Dou G, Zhang Y, Zong C, et al. Application of surgical navigation in styloidectomy for treating Eagle's syndrome. Ther Clin Risk Manag 2016;12:575-83. [PubMed]
Cite this article as: Nicholson OA, Nicholson R. Stylohyoid pain syndrome—an Australian case series and review. Aust J Otolaryngol 2021;4:33.



