
Tonsillectomy in regional Australia: management and outcomes
Introduction
Tonsillectomy is the most common procedure performed by otolaryngologists. Between July 2018 and June 2019 around 30,000 tonsillectomies were performed in Australia (1). Indications include sleep related issues and recurrent tonsillitis among other less common indications. There are expected complications of pain, decreased oral intake, fevers, nausea and vomiting, referred otalgia and voice change. However, it is the bleeding complications which are used as a key performance indicator. This is due to the significant morbidity, increased health care costs and risk of mortality associated with these complications (2).
Rates of post-tonsillectomy bleeding (PTB) vary between studies. Recent Australian data report primary bleeding (bleeding within 24 hours of operation) from 0.3% to 1.5% and secondary bleeding (bleeding greater than 24 hours post-operatively) from 4.7% to 7.7% (3-7). Routine management of these patients includes prompt beside assessment and initial attempts at conservative medical management. However, significant episodes may require return to the operating theatre and/or blood transfusion. Risk factors for PTB including increasing age or age <2 years, male, hot tonsillectomy technique for dissection or haemostasis, surgeon experience, pre-existing coagulopathy and indication for tonsillectomy Quinsy > Recurrent tonsillitis > Sleep related issues have all been identified in the literature (2,8,9).
Wagga Wagga Base Hospital (WWBH) is located within the Murrumbidgee Local Health District in Central South New South Wales, an area encompassing 123,233 sq/km, with an estimated population of 240,000. It is the referral hospital to one base hospital and fifteen district and community hospitals and the only facility with ear, nose and throat (ENT) services (10). This geographic sparsity results in patients from remote locations ≥100 km from WWBH undergoing tonsillectomy. Many practitioners advocate patients remain within proximity to a hospital ENT service (Less than 60 minutes) (11). Whilst this pragmatic approach is sensible and safe it not always achievable outside of metropolitan settings and presents a challenge for rural and regional practitioners and equitable access to health care.
This study primarily aims to investigate the PTB rate in a contemporary regional Australian centre and the risk factors associated with bleeding complications. The study also aimed to determine if patients who lived greater that 100 km from WWBH had a higher rate of complications.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/ajo-21-3).
Methods
Retrospective audit of all patients who had a tonsillectomy at WWBH from January 2014 until June 2018 was conducted. Patients were identified using coding from the medical record department for tonsillectomy and adenotonsillectomy. Tonsillectomies for malignant processes were excluded from the analysis.
Deidentified data for patient demographics, the type of operation, indication, primary operator (consultant or registrar) and postoperative medications, were collected for all cases. In PTB cases we additionally identified rates of primary and secondary bleeding, transfer method, time to surgical or ENT review, subsequent management (medical, surgical and/or transfusion) and geographical distance from WWBH based on home address post code.
Tonsillectomies were preformed or supervised by two consultant surgeons using either cold steel dissection with monopolar haemostasis or monopolar diathermy with monopolar haemostasis. Post-operative analgesia regime included regular paracetamol and ibuprofen for all patients with additional breakthrough oxycodone for adult patients. All cases remained in hospital a minimum of one night post-operatively. Antibiotics were routinely given post-operatively for patients under one of the consultant surgeons and only given if there was a fever recorded overnight for the other. During the study period there was no restriction placed on the discharge destination of the patient. In our practice tonsillectomies are not performed in patients under the age of 2 and those with severe sleep apnoea or other high-risk co-morbidities are referred to metropolitan children’s hospitals in collaboration with the local Paediatricians. Acute medical management of bleeding episodes variably included intravenous antibiotics, tranexamic acid (TXA), and hydrogen peroxide gargle during the study period; however, a draft guideline was introduced in 2019 (Figure S1).
Statistical analysis
All statistical analyses were done using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and conclusions made at 5% significant levels unless otherwise specified. Data values are expressed as mean (SD) or count (%). Two sample t-test, Chi-square test (or Fisher exact test) as well as univariate logistic regression were used to compare the variables between those who had PTB and those who did not. Multivariate logistic regression was used to assess the independent association between the independent variables and PTB. Variable redundancy was done using divisive principal component variable clustering to reduce multicollinearity between variables (SAS Certified Statistical Business Analyst Using SAS 9: Regression and Modelling, SAS Institute Inc., Cary, NC, USA). The final model building was done using Best-subset and Stepwise selection procedures and the best parsimonious model was chosen based on smallest AIC or BIC, and highest AUC values. Results from the chosen model was expressed as odds ratio, OR (95% CI). A variable is considered significantly associated with the PTB if its 95% CI does not contain 1.
Ethics
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from Greater Western Human Research Ethics Committee (2018/ETH00481) and individual consent for this retrospective analysis was waived.
Results
Over the four and a half year study period, a total of A total of 1,209 patients met the inclusion criteria for the cohort. The mean age was 11 [SD: 10] years. There was a preponderance of female (53%) patients. Recurrent tonsillitis (602, 50%) was the most common indication, followed by undocumented (425, 35%), sleep related issues (143, 12%), quinsy (31, 3%) and tonsilloliths (7, 0.7%).
Bleeding rates
Of the total cohort, 45 (4%) had bleeding complications (1% primary, 3% secondary), while 12 (1%) represented with non-bleeding complications (Pain, nausea, decreased oral intake, hypovolaemia). Of those who had bleeding, 7 (14%) presented twice and 1 (2%) presented three times, 3 (7%) returned to theatre, 1 (2%) was admitted to ICU for airway monitoring, and 2 (4%) had blood transfusions. Secondary bleeding occurred at a median of 6 days (range, 2–15).
Geographical distance
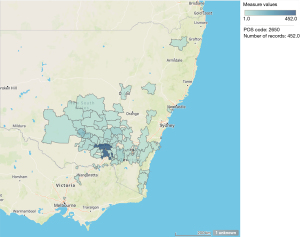
WWBH covers a vast catchment area (Figure 1) with around one third (360, 30%) of patients in our cohort living ≥100 km away based on home address Postcode. Of the patients presenting with PTB the majority (30, 66%) came directly to WWBH however the remainder presented to surrounding facilities (15, 33%). Of those transferred from surrounding facilities (5, 11%) the median (q1, q3) time was 4.1 (1.2, 14.8) hours and all were transferred via road ambulance.
Risk factors
Individuals with PTB are more likely to be older (16 vs. 11 years), have large tonsil size (31% vs. 21%), use opiates (16% vs. 6%) and TXA (11% vs. 1%) on discharge and have comorbidity (38% vs. 25%) (Table 1). Table 2 shows the results from Univariate and Multivariate Binomial Logistic Model for the association of variables events with PTB. In a univariate model, Age, Tonsil size, use of opiates and TXA on discharge are individually associated with PTB. In a multivariate logistic regression, only Age, Tonsil size and use of TXA on discharge are independently associated with the onset of PTB: being older by a year (adjusted odds ratio, AOR =1.03, 95% CI: 1.01–1.06), having larger tonsil size (AOR =5.87, 95% CI: 1.31–26.3), and use of TXA on discharge (AOR =7.15, 95% CI: 2.36–21.6) are all significantly associated with higher odds of having PTB.
Table 1
| Variables | No PTB | PTB | Total | P value |
|---|---|---|---|---|
| N | 1,164 [96] | 45 [4] | 1,209 | |
| Age, years$ | 11 [9] | 16 [11] | 11 [10] | 0.0005 |
| Distance from WWBH, km | 0.64 | |||
| ≤100 km | 816 [70] | 33 [73] | 849 [70] | |
| >100 km | 348 [30] | 12 [27] | 360 [30] | |
| Length of stay post-op, days | 0.26 | |||
| 1 | 188 [16] | 9 [20] | 197 [16] | |
| 2 | 915 [79] | 32 [71] | 947 [78] | |
| 3+ | 31 [3] | 3 [7] | 34 [3] | |
| Unknown | 30 [3] | 1 [2] | 31 [3] | |
| Male | 550 [47] | 21 [47] | 571 [47] | |
| Principal operator | 0.0011 | |||
| Consultant | 1003 [86] | 39 [87] | 1042 [86] | |
| Registrar | 150 [13] | 3 [7] | 153 [13] | |
| Unknown | 11 [1] | 3 [7] | 14 [1] | |
| Tonsil size | 0.06 | |||
| Small | 17 [1] | 0 | 17 [1] | |
| Moderate | 214 [18] | 2 [4] | 216 [18] | |
| Large | 250 [21] | 14 [31] | 264 [22] | |
| Unknown | 683 [59] | 29 [64] | 712 [59] | |
| Method of tonsillectomy | 0.39 | |||
| Cold steel diathermy | 650 [56] | 28 [62] | 678 [56] | |
| Needle tip diathermy | 514 [44] | 17 [38] | 531 [44] | |
| Indications for tonsillectomy | 0.49 | |||
| Recurrent tonsillitis | 579 [50] | 23 [51] | 602 [50] | |
| Sleep related issues | 139 [12] | 4 [9] | 143 [12] | |
| Quincy | 31 [3] | 0 | 31 [3] | |
| Tonsil stones | 7 [0.6] | 1 [2] | 8 [0.7] | |
| Unknown | 408 [35] | 17 [38] | 425 [35] | |
| Method of intubation | 0.34 | |||
| ETT | 1,086 [93] | 43 [96] | 1,129 [93] | |
| LMA | 12 [1] | 1 [2] | 13 [1] | |
| Unknown | 66 [6] | 1 [2] | 67 [6] | |
| Comorbidity (any) | 296 [25] | 17 [38] | 313 [26] | 0.06 |
| Asthma | 163 [14] | 5 [11] | 168 [14] | 0.58 |
| Discharge medications | ||||
| Antibiotics | 537 [46] | 20 [44] | 557 [46] | 0.82 |
| Opiates | 75 [6] | 7 [16] | 82 [7] | 0.0171 |
| Steroid | 2 [0.2] | 0 | 2 [0.2] | 1 |
| Tranexamic acid | 14 [1] | 5 [11] | 19 [2] | 0.0004 |
$, data values presented as mean [SD]. Data presented as n [%] unless otherwise specified. PTB, post-tonsillectomy bleeding; WWBH, Wagga Wagga Base Hospital; ETT, endotracheal tube; LMA, laryngeal mask airway.
Table 2
| Variables | Univariate | Multivariate |
|---|---|---|
| N [%] | 1,164 [96] | 45 [4] |
| Age, years | 1.04 (1.02, 1.06) | 1.03 (1.01, 1.06) |
| Distance from WWBH, km | ||
| ≤100 km | 1.17 (0.59, 2.29) | |
| >100 km (ref) | ||
| Length of stay post-op, days | ||
| 1 (ref) | ||
| 2 | 0.73 (0.34, 1.56) | |
| 3+ | 2.02 (0.52, 7.88) | |
| Male | 0.97 (0.53, 1.77) | |
| Principal operator | ||
| Consultant | ||
| Registrar | 0.51 (0.15, 1.68) | |
| Tonsil size | ||
| Small to moderate | ||
| Large | 6.47 (1.45, 28.76) | 5.87 (1.31, 26.3) |
| Method of tonsillectomy | ||
| Cold steel and diathermy | ||
| Needle tip diathermy | 0.77 (0.42, 1.42) | |
| Indications for tonsillectomy | ||
| Recurrent tonsillitis | ||
| Sleep related issues | 0.72 (0.25, 2.13) | |
| Quincy or tonsil stones | 0.66 (0.08, 5.04) | |
| Method of intubation | ||
| ETT | ||
| LMA | 2.11 (0.27, 16.55) | |
| Comorbidity (any) | 1.78 (0.96, 3.29) | |
| Asthma | 0.77 (0.29, 1.97) | |
| Discharge medications | ||
| Antibiotics | 0.93 (0.51, 1.70) | |
| Opiates | 2.68 (1.16, 6.19) | |
| Tranexamic acid | 10.3 (3.52, 29.9) | 7.15 (2.36, 21.6) |
Data presented as AOR (95% CI) unless otherwise specified. PTB, post-tonsillectomy bleeding; WWBH, Wagga Wagga Base Hospital; ETT, endotracheal tube; LMA, laryngeal mask airway.
Discussion
Despite advancement in patient selection, surgical technique and medical management, PTB remains a key performance indicator and an area of ongoing research and quality improvement. The rate of PTB during the study period, 3.0% for secondary and 0.7% for primary bleeding, was within the range of the published data. Among the risk factors identified increasing age (every 1 year increase) is consistently found to be a risk factor for PTB (2,3,8). Having larger tonsil size (AOR =5.87, 95% CI: 1.31–26.3) can likely be contributed to difficulty of dissection or increased vascularisation of the tonsil bed. What has not previously been identified, to our knowledge, is an increased risk with post-operative TXA (AOR =7.15, 95% CI: 2.36–21.6). However, this is unlikely to reflect a true increased risk given the low number of patients given TXA in our cohort (20, 1.6%).
TXA
TXA is an antifibrinolytic agent that inhibits activation of plasminogen to plasmin (12). It has been in use for over 60 years and has proven effectiveness in reducing blood loss and transfusion requirements across a diverse range of surgical and medical disciplines, most notably in major trauma and post-partum haemorrhage (12). It can be administered as an intravenous, oral or topical solution. More recently it has gained increasing popularity for several ENT applications including epistaxis, PTB and endoscopic sinus surgery (13).
The use of TXA in our study may reflect a change in practice during the study period, TXA use was only seen in tonsillectomies from mid 2015 to 2018 and never given routinely. This results in concurrent selection bias of those patient already deemed at high risk of PTB by the primary operator or supervising consultant surgeon. The operative comment was most often—large volume ooze intraoperatively.
Koizumi et al. (14) took data from the Diagnosis Procedure Combination database in Japan. From their cohort of 110,928 patients they found administration of TXA from Day 0 (n=50,501) showed no statistically significant reduction in the rate of PTB, risk of return to theatre or transfusion. However, there were limitations from the database being able to distinguish administration of TXA after PTB from planned administration on the day of tonsillectomy.
Pittore et al. (15) divided their cohort of 236 children into those who had no TXA and those who took a 10-day course. They found that that there was no statistically significant difference in the proportion of post PTB in the study group with TXA 2.01% vs. without TXA 3.44%. However, their population size was likely underpowered to detect statistical differences.
Robb et al. (16) in a pilot study gave their whole cohort (n=476) perioperative intravenous TXA as a single dose with a resulting primary bleed rate of 0.4%. The authors concluded there was possible evidence that TXA may reduce the incidence of primary bleeding.
Chan et al. (17) conducted a systematic review and meta-analysis looking at 7 studies mostly published from 1970–1980. They concluded that TXA lead to a significant reduction in the volume of blood loss and the duration of bleeding but not the overall rate of PTB or those requiring further intervention.
More recently Smith et al. (18) looked at patients admitted with secondary PTB and the effect intravenous TXA had on the rate of return to theatre and need for transfusion. They found a statistically significant reduction in the rate of return to theatre in those who received TXA 13% vs. those who did not receive TXA 23% (P=0.042). Reassuringly none of the studies identified any significant side effects of TXA administration.
Given the limited conclusive data, the decisions to use TXA needs to be based on its intended indication. Either given in the perioperative period to reduce primary bleeding or in an acute emergency setting following a secondary bleed to reduce duration and volume of bleeding and rate of return to theatre. Furthermore, oral solutions have been shown to maintain therapeutic levels in the saliva for more than two hours post administration and may be a useful adjunct therapy to systemic administration (12).
Geographic distance
Of those patients who presented to other facilities with PTB, a minority were transferred to WWBH. With a median transfer time of 4.1 hours and all were transferred via road ambulance. However, ten PTB were not transferred and remained at their facility of initial presentation. This suggests that patients who are outside of “safe” geographical boundaries can be managed remotely and transferred as clinically indicated. Remote management requires familiarity with surrounding health services and capabilities and reliance on proactive and early referral to the ENT service. Whilst during the study period there were no increased adverse outcomes, further data is required to establish whether there is an increased risk with patients who live in geographically remote locations without immediate access to an ENT service.
Surveillance and quality improvement
Given the relatively low rates of tonsillectomy bleeding, isolated studies generally do not have the necessary sample sizes to detect small effects on outcomes. Several overseas initiatives attempted to look at this.
The National Prospective Tonsillectomy Audit (NPTA) (19) in the United Kingdom 2003/04 had several recommendations from their 50,531 cases. Namely avoidance of hot tonsillectomy techniques and ongoing audit and review of department tonsillectomy data.
The National tonsil surgery register in Sweden (NTSRS) has been used in several studies to date. In 2014, 15,734 cases were analysed and showed all hot tonsillectomy techniques were associated with a higher rate of tonsillectomy bleeding when compared with cold steel (20). Then in 2018 the National tonsil surgery register was again used to target quality improvement programs in centres with above national average PTB rates. These programs included education, evidence updates and training on local data analysis. This resulted in a drop of PTB rates 12.7% to 7.1%. whilst no drop was seen in the control group of centres which did not receive the quality improvement program (21).
Centralised data allows for large datasets and targeted systemic quality improvement strategies. The newly established Australian Society of Otolaryngology Head and Neck Surgery (ASOHNS) tonsillectomy data registry will provide national data to better inform current and future trends in Australia.
Limitations
There are several limitations to our study, in addition to those inherent in a retrospective case series. Firstly, we include data from a single institution. Secondly, we did not include data from patients operated on in the private hospital, which would potentially double the number of cases in the series. Thirdly, we did not include patients who presented with PTB from other institutions. Finally, the bleeding rate may be higher than reported due to patients either not presenting, presenting to facilities outside of the local health district or not detected at routine follow-up as this is generally with local medical officers rather than the ENT service. Underreporting of PTB rate has been noted in previous guidelines as minimal bleeding episodes may be managed at home and medical attention never sort (2).
Conclusions
This retrospective study provides data on contemporary regional Australian practice. We observed primary and secondary bleeding rates within acceptable levels. In our series patients living in areas ≥100 km from and ENT service did not have increased complications due to PTB based on geographical distance and all bleeds were successfully managed either remotely or with transfer to WWBH. Further prospective trails and larger dataset analysis with provide improved evidence for future management options and quality improvement strategies.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/ajo-21-3
Data Sharing Statement: Available at https://dx.doi.org/10.21037/ajo-21-3
Peer Review File: Available at https://dx.doi.org/10.21037/ajo-21-3
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/ajo-21-3). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from Greater Western Human Research Ethics Committee (2018/ETH00481) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Medicare Item Reports. [Internet]. Human Services Department. 2020 [cited 2020 Mar 10]. Available online: http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp
- Mitchell RB, Archer SM, Ishman SL, et al. Clinical Practice Guideline: Tonsillectomy in Children (Update). Otolaryngol Head Neck Surg 2019;160:S1-S42. [Crossref] [PubMed]
- Kwok MM, Subramaniyan M, Rimmer J, et al. Post-tonsillectomy haemorrhage in Australia—a multivariable analysis of risk factors. Aust J Otolaryngol 2018;1:2. [Crossref]
- Hinton-Bayre AD, Noonan K, Ling S, et al. Experience is more important than technology in paediatric post-tonsillectomy bleeding. J Laryngol Otol 2017;131:S35-40. [Crossref] [PubMed]
- Morris S, Hassin E, Borschmann M. Overnight in-hospital observation following tonsillectomy: retrospective study of post-operative intervention. J Laryngol Otol 2018;132:46-52. [Crossref] [PubMed]
- Walker P, Gillies D. Post-tonsillectomy hemorrhage rates: are they technique-dependent? Otolaryngol Head Neck Surg 2007;136:S27-31. [Crossref] [PubMed]
- Cadd B, Rogers M, Patel H, et al. (Ton)silly seasons? Do atmospheric conditions actually affect post-tonsillectomy secondary haemorrhage rates? J Laryngol Otol 2015;129:702-5. [Crossref] [PubMed]
- Tomkinson A, Harrison W, Owens D, et al. Risk factors for postoperative hemorrhage following tonsillectomy. Laryngoscope 2011;121:279-88. [Crossref] [PubMed]
- Francis DO, Fonnesbeck C, Sathe N, et al. Postoperative Bleeding and Associated Utilization following Tonsillectomy in Children. Otolaryngol Head Neck Surg 2017;156:442-55. [Crossref] [PubMed]
- Gilchrist K. The Murrumbidgee Local Health District 2018. Available online: https://www.mlhd.health.nsw.gov.au/getmedia/6dd77cb1-27e0-4fa2-afc0-48af0823e869/Report-Murrumbidgee-Summary-Health-and-Population-Profile
- Anning R, Cope D, Treble A, et al. Tonsillectomy: Does proximity from otolaryngology care influence the intra-operative or post-operative plan? Aust J Otolaryngol 2021;4:25. [Crossref]
- Tengborn L, Blombäck M, Berntorp E. Tranexamic acid--an old drug still going strong and making a revival. Thromb Res 2015;135:231-42. [Crossref] [PubMed]
- Robb PJ. Tranexamic acid - a useful drug in ENT surgery? J Laryngol Otol 2014;128:574-9. [Crossref] [PubMed]
- Koizumi M, Ishimaru M, Matsui H, et al. Tranexamic acid and post-tonsillectomy hemorrhage: propensity score and instrumental variable analyses. Eur Arch Otorhinolaryngol 2019;276:249-54. [Crossref] [PubMed]
- Pittore B, Pelagatti CL, Fraser L, et al. Tranexamic Acid in the Management of the Post Adeno- Tonsillectomy Phase. Annals of Otolaryngology and Rhinology 2015;2:1060.
- Robb PJ, Thorning G. Perioperative tranexamic acid in day-case paediatric tonsillectomy. Ann R Coll Surg Engl 2014;96:127-9. [Crossref] [PubMed]
- Chan CC, Chan YY, Tanweer F. Systematic review and meta-analysis of the use of tranexamic acid in tonsillectomy. Eur Arch Otorhinolaryngol 2013;270:735-48. [Crossref] [PubMed]
- Smith AL, Cornwall HL, Zhen E, et al. The therapeutic use of tranexamic acid reduces reintervention in paediatric secondary post-tonsillectomy bleeding. Aust J Otolaryngol 2020;3:10. [Crossref]
- BAO-HNS, RCS. National Prospective Tonsillectomy Audit. Royal College of Surgeons of England, 2005.
- Söderman AC, Odhagen E, Ericsson E, et al. Post-tonsillectomy haemorrhage rates are related to technique for dissection and for haemostasis. An analysis of 15734 patients in the National Tonsil Surgery Register in Sweden. Clin Otolaryngol 2015;40:248-54. [Crossref] [PubMed]
- Østvoll E, Sunnergren O, Stalfors J. Increasing Readmission Rates for Hemorrhage after Tonsil Surgery: A Longitudinal (26 Years) National Study. Otolaryngol Head Neck Surg 2018;158:167-76. [Crossref] [PubMed]
Cite this article as: Jones A, Grant A, Saputra L, Lathif A, Krishan B. Tonsillectomy in regional Australia: management and outcomes. Aust J Otolaryngol 2021;4:41.


