
Head and neck cancer surgery during the COVID-19 pandemic: the Chris O’Brien Lifehouse experience and narrative review
Introduction
The SARS-CoV-2 pandemic, also known as COVID-19, has seen a wave of critically ill patients and a dramatic change in the focus of hospitals and healthcare workers worldwide, shifting medical care away from those with chronic illness and cancer to prepare to treat COVID-19 patients. Head and neck cancer (HNC) patients require timely expert multidisciplinary care for optimum functional and survival outcome. The risk of viral transmission remains high for all therapeutic and diagnostic procedures, but is significantly higher for HNC and lung cancer patients due to the high viral loads of COVID-19 in the upper aerodigestive tract (1). Management of these HNC patients therefore carry particular risk of virus transmission to health care professionals, other patients, carers, family members and society as a whole.
Chris O’Brien Lifehouse (COBLH) is a tertiary oncology hospital which provides high volume, multidisciplinary HNC treatment (among other cancer services) in Sydney, Australia. The multidisciplinary team (MDT) is comprised of surgeons, medical and radiation oncologists, pathologists, radiologists, operating staff, specialised nurses, allied health and support staff. One notable feature allowing us to continue operating in COBLH throughout the pandemic is that, whilst we are geographically close and with clinical teams linked to a large tertiary public hospital treating COVID-19 patients, we are our own free-standing institution with its own independent executive management team. COBLH is a modern, purpose-built, comprehensive cancer care facility providing clinical care, research and education. It has its own separate support services including radiology, clinical sterilization and patient services. As most care is elective—though urgent—we were able to promptly introduce precautionary measures in many areas of the patient experience and clinical pathways.
The patient cancer journey has been profoundly impacted by the pandemic from the initial diagnostic workup, through to operative and adjunctive management, ward care, discharge and follow-up. Around the world, patients have experienced significant delays or have had to compromise with non-operative management such as primary radiotherapy where surgery might have otherwise been indicated (2). Australia has been relatively lucky with low numbers of COVID-19 cases compared to other parts of the world. Fortunately, there have been no cases of COVID-19 at our centre and, as the incidence of COVID-19 in Australia remains low, we have increased our surgical practice beyond only the most urgent cases. Nonetheless we maintain our vigilance to prevent infection spreading in the vulnerable oncology patients and staff caring for them within our hospital. We aim to share some of the challenges and lessons that have contributed to the success of continuing safe, high-level, timely care for our patients as we move into the next phase of maintaining HNC surgical practice in a population potentially carrying COVID-19.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://ajo.amegroups.com/article/view/10.21037/ajo-21-12/rc).
Methods
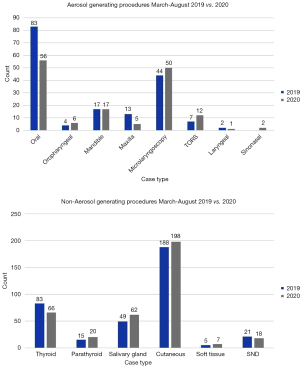
We retrospectively collected data regarding case type, volume, operating time and total anaesthetic time from the period of March to August 2019 and the same time period in 2020 to investigate the impact of COVID-19 on surgical workload and flow. Institutional ethics approval was obtained (HREC X20-0337/LH20.074). Data analysis was performed using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA).
Discussion
General hospital measures
Oncology patients are frequently immunosuppressed and patients are at particularly high risk of spreading COVID-19 infection when undergoing surgery or treatment if infected, by the formation of aerosolised viral particles. One of the key challenges in limiting transmission are asymptomatic carriers amongst patients, contacts and staff, and lack of specific diagnostic testing. Clinical similarity between COVID-19 illness with more common respiratory viral illness, prevalent during the winter season when community spread was at its peak, further complicated matters.
Rapidly changing advice regarding the risk of COVID-19 and best practice for limiting the spread of infection fuelled the high level of anxiety around the pandemic, which undoubtedly impacted staff. Frequent email correspondence from the hospital executive team helped keep everyone abreast of the latest changes, boosting morale and encouraging a cohesive hospital-wide response to COVID-19. Staff wellbeing has been promoted with several novel strategies such as online exercise classes, music therapy and virtual debriefing sessions. The general hospital measures are summarised in Table 1.
Table 1
| Area | Intervention |
|---|---|
| Hospital measures | Single entrance |
| Universal fever and symptom screening | |
| Regular COVID-19 update from executive | |
| Safe distancing with visual cues | |
| Limit of persons in lifts, meeting rooms, common areas | |
| Staff wellbeing measures | |
| Face masks for patient interactions | |
| Patient measures | 14-day home isolation prior to elective surgery |
| 3× COVID-19 screening phone calls during isolation | |
| Telehealth where possible for pre-admission appointment and outpatient follow-up | |
| Single nominated visitor | |
| Pre-operative temperature screening |
MDT meeting and outpatient clinic
At our centre, the head and neck MDT is usually run in a meeting room consistently attended by around 30 clinicians including surgeons, radiation and medical oncologists, pathologists, radiologists and allied health staff—a single infected person could potentially spread to the entire head and neck service. Continued discussion of complex cancer patients at the MDT meeting is also essential to provide the best care (3) and as social distancing was enforced, a transition to utilizing digital tools was required. With expertise from the information technology department, fully equipped video conference rooms have been established with screens for digitalised radiology, histopathology, clinical photography and video viewing capabilities. Security measures for joining the meeting have been implemented due to potential threats to confidentiality and data security with private email lists, personal invitations to the meetings with password protection, a vigilant chairperson, overseen by a dedicated hospital technology team. Pre-COVID-19, patients attended the clinic for discussion and examination. Now with a change to the virtual environment and adaptability of clinicians to continue to present comprehensive patient details, radiology and pathology, there has been no detrimental effect to the high-quality MDT review we are able to deliver.
Operating theatre
Since 16th March 2020, when we first changed our personal protective equipment (PPE) practice in theatres to reflect the increased risk posed by patients potentially infected with COVID-19, we have operated on number of patients similar to our usual case load pre-Covid (Figure 1). The total number of cases from March to August 2019 was 688 compared with 666 in the same time period of 2020. To date, we have had no known COVID-19 positive patients requiring surgery. From the outset, high level airborne precautions were adopted with regular review and update based on guidelines from the British Association of Head & Neck Oncologists (BAHNO), the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS), the Australian Society of Otolaryngology Head and Neck Surgery (ASOHNS) and the Australian Society of Anaesthetists (ASA) recommendations. As COVID-19 case numbers have remained low, our precautions have been tailored accordingly to reflect risk.
Anaesthetic
Outside HNC procedures, anaesthetic staff are at the highest risk due to exposure during routine aerosol generating procedures (AGPs) thus pre-anaesthetic patient handling, intraoperative airway decision making and post-operative recovery practice have all required careful consideration.
All theatres where possible were converted to negative pressure airflow, and patients transported directly into theatre, bypassing the anaesthetic room to minimise potential contamination of equipment and surfaces. Initially, within theatre, induction and intubation was conducted with only the anaesthetist and single anaesthetic nurse in complete airborne PPE with N95 masks and face shields or sterilisable powered air purifying respirators (PAPRs). Following intubation, the theatre is “rested” for 15–30 minutes, determined by hospital engineers as the time for the entire volume of air in the room to be completely refreshed by the internal circulatory system. Necessary tasks such as case-planning and the surgical timeout checklist followed this rest or were conducted by speakerphone to enable communication with anaesthetic staff within the theatre and other staff outside.
Airway and respiratory support measures have been modified to again reduce aerosolization risk. In line with ASA guidelines, there was initial restriction in use of nebulisers, inhalational sedation, open-circuit and non-invasive ventilation, bag-mask ventilation and prohibition of THRIVE (high flow nasal prongs) and jet ventilation (4). Following case completion, staff were again reduced to bare-minimum during extubation and a further rest period was enforced before cleaning the theatre. Patients were transferred to recovery or ICU directly with the transfer team doffing their full PPE after handover and then proceeding to shower and change theatre scrubs between cases
Surgery
HNC operations have been observed to pose the highest risk to involved HCWs due to the high viral replication that occurs in the upper aerodigestive tract, the frequency and duration of AGPs, and use of suction and electrocautery causing continuous aerosolization (5). In the early stages of the pandemic with concerns that cases would overwhelm the health services, government-mandated cessation of elective surgery permitted only category 1 or 2, high-priority cancer cases to continue, limiting unnecessary exposure of personnel and depletion of PPE. The hospital in conjunction with staff sourced a supply of N95 masks in addition to impermeable gowns, eyewear and gloves in order to continue performing urgent cancer surgery without delay. Staff have been trained on correct donning and doffing procedures for PPE in addition to visual aids stationed outside every operating theatre. Strict limits on the numbers of people allowed in each theatre decreased unnecessary foot traffic and exposure of those not directly involved with the case. Non-essential equipment was moved to outside each theatre, initially with an external runner supplying the relevant pieces of equipment as required for high-risk cases. The initial implementation of these measures was time consuming particularly for AGPs where additional PPE was used. The average duration of AGPs was 85 minutes (IQR 455) in March 2019 compared with 180 minutes in March 2020 (IQR 366) but normalised once staff became practiced and restrictions eased (Table 2).
Table 2
| AGPs | Median [IQR], minutes | |
|---|---|---|
| 2019 | 2020 | |
| March | 85 [455] | 180 [388] |
| April | 62 [56] | 135 [344] |
| May | 108 [260] | 95 [144] |
| June | 88 [339] | 823 [262] |
| July | 184 [391] | 106 [444] |
| August | 94 [420] | 79 [141] |
AGP, aerosol generating procedure.
Speciality and case-specific protocols have been developed which guide PPE selection and rationalise use during COVID-19 (Table 3). Oral cavity, oropharyngeal, nasal and laryngeal cases required more comprehensive PPE and PAPRs or N95 masks and complete impermeable gowns are required for all staff in theatre. Procedures not involving the upper aerodigestive tract mucosa, so-called ‘clean neck surgery’ such as thyroid, parathyroid, parotid and cutaneous malignancies are undertaken with traditional surgical PPE due to a lower risk of viral shedding. Furthermore, the sequence of multi-stage ablation and reconstructive procedures has been modified to reduce risk to the teams—the key example being oral and oropharyngeal cavity reconstruction. Neck dissection and free-flap preparation are performed first with the mouth covered by an impermeable plastic adhesive whilst surgical staff don N95 masks and usual PPE. When the upper aerodigestive component is commenced, the entire team rescrubs into PAPRs for the remainder of the case. The upper aerodigestive tract was prepared and washed with betadine and plume suction utilising a smoke evacuation system was performed during resection.
Table 3
| AGP case types | Non-AGP case types |
|---|---|
| Oral cavity | Thyroid gland |
| Oropharyngeal | Parathyroid glands |
| Sinonasal | Cutaneous |
| Nasopharyngeal | Neck dissection |
| Laryngeal | Parotid gland |
| Transoral robotic resections | Submandibular gland |
| Temporal bone resections | Soft tissue tumours |
| Microlaryngoscopy, oesophagoscopy, bronchoscopy, nasendoscopy | |
| Tracheostomy | |
| Gastroscopy and PEG insertion |
AGP, aerosol generating procedure; PPE, personal protective equipment.
Extensive experience in complex major head and neck resection and reconstruction at COBLH has positioned us well to personalise placement of a covering tracheostomy. Combined with the increased risk of viral exposure we have been able to safely avoid routine tracheostomy in substantial number of cases (6), after close discussion with both the surgical and anaesthetic teams in order to avoid significant viral exposure during the case and post-operatively on the ward.
Radiation and medical oncology
In order to minimise the need for patients to attend the hospital, the majority of non-treatment related appointments were converted to Telehealth. No changes were made to chemotherapy administration or choice of regimens for curative treatment of HNCs. However contingency plans were prepared, outlining what treatments would be withheld for certain tumour types and stages in the event that the pandemic resulted in staff or other resource limitations. Fortunately, this did not occur.
Non-surgical and palliative management of HNC patients with chemoradiation has also been impacted during the COVID-19 pandemic. Optimum oncologic and functional outcomes are worse for patients who experience treatment interruption or delays (7), but a balance must be found to maintain healthcare worker safety.
HNC which typically requires operative management such as advanced oral cavity, cutaneous and thyroid has been able to continue at COBLH with heightened PPE and additional precautionary measures. We have not identified any change in definitive management from surgical to non-surgical treatment as a result of COVID-19.
Pathology
Pathology plays an integral role in pre-operative diagnosis, intra-operative frozen section consultations and evaluation of diagnostic and prognostic features in the final resected specimens.
Fine needle aspiration (FNA) procedures are generally the first diagnostic step. All HN FNAs, where the aspirator performing the FNA is in very close proximity to the mouth and nose of the patient were considered AGP and required the use of N95 masks and full PPE including eye protection. A significant reduction in salivary and thyroid FNAs was noted at the initial peak of COVID-19 crisis. However, FNAs of neck lumps continued at a similar rate as under non-COVID circumstances. All aspirated material is divided for rapid on-site evaluation (ROSE) and Papanicolou stain at our center under a PC2 hood.
Intra-operative frozen sections were continued with the use of PC2 hoods, PPE including eye protection and N95 masks with the understanding that the patient is negative for COVID-19. The surgical team were encouraged to send tissues of interest for frozen section rather than the entire 3dimensional complex specimen which would prolong the exposure to HNC through increased requirement of photography, manipulation and keeping the specimen fresh until the intra-operative frozen sections have been finalised and discussed with the surgical team.
All permanent sections were handled by a single pathologist resulting in a lost educational opportunity for the trainees. Physical sharing of slides and multi-header microscope consultations were banned. Thus, if a second opinion was needed, the entire case was handed over to a specialist pathologist. The cases were kept in the pathologists’ office and only removed once the MDT discussions were completed. Following the slides were sprayed with alcohol and kept in decontamination zone for 2 days prior to archiving.
Tumour banking is an important activity at our institution. This was limited to cases on clinical trials and extremely rare diagnoses to rationalise the use of N95 masks and PPE when the supply chains were uncertain. This also reduced foot traffic at the peak of COVID 19 crises.
Ward
The post-operative period for HNC patients continues to pose a risk of viral transmission to staff, family and other patients. The key challenges faced were an urgent need for dynamic policy and guidelines for direct clinical care, staffing and PPE rationalisation with cornerstone of safe and successful patient care in this time being frequent and clear communication from department heads and executives to staff on the front line.
Firstly, clinical care guidelines were developed and distributed for tracheostomy management, decannulation, use of nebulised medication and oxygen supplementation. These have been regularly reviewed and updated as guidelines have changed. We are fortunate to provide single rooms for each patient and have a dedicated negative pressure room on all wards. Negative pressure rooms are utilised in routine care of patients who have URTI symptoms or have increased aerosolization risk, though clinically higher-risk patients are nursed in the closely observed beds opposite the nurses’ station. Emergency packs with pre-assembled airborne PPE and equipment is readily available to allow rapid attendance and safe care in deteriorating HNC patients.
Given the restriction in visitors, digital messaging devices are provided to patients to enable video-calls for family members in lieu of face-to-face hospital visits. Patient liaison officers have been contacting family members to address any of their concerns and ensure they feel supported at home.
Follow-up and outpatient clinic
Integration of digital platforms continues after patients are discharged, with routine follow-up appointments transitioned to videoconference or telephone calls where possible. Outreach clinics to peripheral health districts have been curtailed with again a transition to phone and video calls. For patients who must attend the clinic, waiting rooms and appointments are spaced out to comply with social distancing measures whilst staff wear N95 masks and eye protection during consultations. Flexible nasendoscopy is an AGP and as recommended by the international guidelines judicious selection of patients requiring examination is suggested. For those who require endoscopy, a dedicated single room with full airborne PPE available and an adjacent sterilisation room to clean the scopes and surfaces between patients is used.
Trainees and education
As a large teaching hospital with international fellows, trainees and medical students, education and training opportunities have also been heavily impacted by COVID-19. Reduced non-essential staff has meant medical students and observers are unable to attend clinics and theatres. Several planned face to face courses, seminars and our annual head and neck dissection and reconstruction course have been postponed indefinitely until social distancing restrictions are eased. Fellowships positions which had been filled by international surgeons have had to be replaced due to heavy restrictions on global travel by allocating positions to national candidates.
Whilst some education prospects have been missed, there have been advantages in transitioning to online conference platforms. Several international conferences, lecture series and academic meetings have been able to proceed with greater ease thanks to digital conferencing platforms which may be a positive change that persists into the future.
Conclusions
Management of head and neck oncology patients must continue even during healthcare crises like the COVID-19 pandemic. As a dedicated Covid-free, independent cancer centre, we have been successful in continuing high-level and prompt care with little to no change in case numbers or operating times. This can be achieved by rapidly instituting multi-level changes to all points of patient care, utilising clear communication from executive and a multidisciplinary-team based approach.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ajo.amegroups.com/article/view/10.21037/ajo-21-12/rc
Peer Review File: Available at https://ajo.amegroups.com/article/view/10.21037/ajo-21-12/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ajo.amegroups.com/article/view/10.21037/ajo-21-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Institutional ethics approval was obtained (HREC X20-0337/LH20.074).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gandhi M, Yokoe DS, Havlir DV. Asymptomatic Transmission, the Achilles' Heel of Current Strategies to Control Covid-19. N Engl J Med 2020;382:2158-60. [Crossref] [PubMed]
- Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID-19 pandemic: Reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol 2020;105:104684. [Crossref] [PubMed]
- Heineman T, St John MA, Wein RO, et al. It Takes a Village: The Importance of Multidisciplinary Care. Otolaryngol Clin North Am 2017;50:679-87. [Crossref] [PubMed]
- Brewster DJ, Chrimes N, Do TB, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust 2020;212:472-81. [Crossref] [PubMed]
- Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID-19 pandemic: Reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol 2020;105:104684. [Crossref] [PubMed]
- Dawson R, Phung D, Every J, et al. Tracheostomy in free-flap reconstruction of the oral cavity: can it be avoided? A cohort study of 187 patients. ANZ J Surg 2021;91:1246-50. [Crossref] [PubMed]
- Schutte HW, Heutink F, Wellenstein DJ, et al. Impact of Time to Diagnosis and Treatment in Head and Neck Cancer: A Systematic Review. Otolaryngol Head Neck Surg 2020;162:446-57. [Crossref] [PubMed]
Cite this article as: Phung D, Dawson R, McInnes S, Stokan M, Gupta R, Clark J, Low TH(, Boyer M, Milross C, Elliott MS, Palme CE. Head and neck cancer surgery during the COVID-19 pandemic: the Chris O’Brien Lifehouse experience and narrative review. Aust J Otolaryngol 2022;5:4.


