Peri-operative measures to prevent middle turbinate lateralisation and adhesion formation in endoscopic sinus surgery—a systematic review of the literature
Introduction
Chronic rhinosinusitis (CRS) is a common sinonasal pathology with a prevalence of approximately 5–12%, often requiring referral to an otolaryngologist (1-3). Endoscopic sinus surgery (ESS) is performed with the goal of re-establishing sinus ventilation and function. ESS is supported by a significant evidence base where maximal medical management, often a combination of saline nasal irrigation, systemic/topical corticosteroids and antibiotic therapy, has been insufficient to control disease, is contraindicated or not tolerated. However, surgical management is largely considered not to be curative for patients, rather, it serves to optimise patency of anatomical drainage pathways, facilitate mechanical lavage of inflammatory debris and hypersecretory mucin with saline irrigation, and maximise topical medication distribution to diseased mucosa (4).
The ostiomeatal complex (OMC) is a critical area, routinely addressed as one of the earliest steps of ESS. The OMC includes the maxillary ostium, ethmoidal infundibulum, bulla ethmoidalis, uncinate process and hiatus semilunaris. It incorporates the “common drainage pathway” of the maxillary, frontal and anterior ethmoid sinuses, and is commonly affected in patients with CRS of various endotypes (5,6). However, even with meticulous surgical technique and appropriate post-operative care, synechiae (adhesions) may form between the middle turbinate (MT) and lateral nasal wall, as both structures are immediately adjacent and may have matching exposed mucosal abrasions (7,8). It is reported that approximately 14% of patients undergoing endoscopic sinus surgery (ESS) will require revision surgery at a later stage (7). Previous studies have suggested that ESS failures requiring revision surgery are often secondary to middle turbinate lateralisation and adhesion formation (MiTLAF), ostial scarring/stenosis, and incomplete surgical clearance of disease (8).
MiTLAF and maxillary ostial stenosis are distinct complications sharing common pathophysiology, ultimately leading to impaired sinus drainage and reduced sinus ventilation which fails to improve with both systemic or topical treatment. MiTLAF may sometimes be severe enough to cause sinus ostial stenosis. Ramadan et al., in a study of 682 post-ESS patients, found that 27% had maxillary ostial stenosis and scarring (9); similarly, Musy and Kountakis found 39% of 80 post-ESS patients studied had maxillary ostial stenosis secondary to synechiae, often in conjunction with MT lateralisation (10). In addition to maxillary ostial stenosis, the frontal sinus outflow tracts were also affected by synechiae formation. Otto and Delgaudio in 2010 investigated the pathology of revision ESS and, in 289 patients studied, 30% had synechiae with lateralised MTs (11).
Bassiouni et al. investigated the pathophysiologic processes surrounding synechiae development and identified that aberrant wound healing and wound contraction occurs at the MT axilla due to opposing mucosal abrasions between the MT and lateral nasal wall (12). Patients with synechiae demonstrate poorer quality-of-life scores specific to sinus disease and experience less improvement in Rhinosinusitis Disability Index (RSDI) (13.53±2.38 vs. 21.41±1.28, P<0.05), and Chronic Sinusitis Survey (CSS) (14.58±4.05 vs. 21.23±1.59, P=n.s.) than those without (13).
Synechiae are thought to cause nasal obstruction by reducing airflow and increasing resistance at the middle meatus. Synechiae formation is also postulated to result in impaired frontal sinus drainage, and obstruction of the anterior ethmoid cavity and middle meatal antrostomy. MT synechiae are implicated in reduced sinus ostial ventilation, impaired sinus lavage and topical medication distribution, leading to recurrent disease and symptom recurrence (12).
As a result, prophylactic techniques to minimise synechiae formation during ESS are indicated to reduce their incidence, and associated complications. Various techniques for synechiae prevention have been described including Bolgerisation (14-16), middle turbinate conchopexy (16-20), silastic splint placement (21-25), absorbable and non-absorbable middle meatal spacers (26-34), hyaluronic acid packing (35-38), and middle turbinate resection (39-45). However, there is limited evidence in the literature comparing the efficacy, safety (complication rate), ease-of-use and patient-discomfort with each technique. We present the following article in accordance with the PRISMA reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-6/rc).
Aims
This study aimed to systematically review the literature regarding MiTLAF prevention techniques in ESS. The primary outcome of the study was the efficacy of each technique with regard to MiTLAF prevention. Secondary outcomes included complication rates, CRS outcome-measures, ease-of-use for surgeons and patient-discomfort.
Methods
Ethics
The study adhered to the tenets of the Declaration of Helsinki. Human research ethics committee (HREC) approval was not required as no human subject participants were involved. Reported data was extracted from existing literature.
Study design
Systemic review was performed on literatures related to preoperative techniques for preventing MiTLAF in ESS.
Search strategies
A review of the published literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Embase, Ovid-Medline, and Ovid-PubMed databases were searched for eligible studies using the search terms/strategies reported in Appendix 1-3. The complete historical range from each database through to October 2020 was explored. Searches were limited to those involving human subjects, published in the English Language and with full-text availability.
Inclusion and exclusion criteria
Published articles were included if they assessed operative techniques in the prevention of middle turbinate synechiae formation for ESS in adult patients (age >18).
Only studies that investigated the rate of synechiae formation in the study design, with or without comparison against a control arm, were included.
Studies were excluded if insufficient data were available, patients underwent operations other than ESS for CRS, or the paper was a review article.
Data extraction
Study data included year of publication, type of study, number of patients, rate of synechiae formation, subjective and objective outcome measures of sino-nasal disease, complications, and last follow-up duration.
Study selection
Search strategies were implemented by author HK; results were imported into Endnote (version X9, Clarivate Analytics, 2020), a reference management software. Duplicate references were removed by HK via manual search. Remaining titles were independently screened by HK and EW for eligibility against inclusion and exclusion criteria. Reference lists of available full-text articles were manually screened for further studies eligible for inclusion. Any discrepancies were referred to NS, senior author and fellowship-trained specialist rhinologist, for final decision.
Quality/risk of bias
A QUADAS-2 model was used for risk of bias assessment of the included literature. This approach evaluated the domains of “patient selection”, “index test”, “reference standard” and “flow and timing” in ascertaining areas of concern within the studies, and why they were subject to bias.
Statistical analysis
Due to significant variation in study designs within each technique, as well as heterogeneity in designs between each technique, meta-analysis of data was not possible.
Results
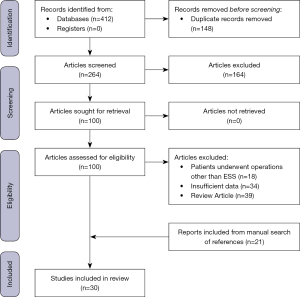
Four hundred and twelve papers were identified using search strategies outlined in Appendix 1-3. One hundred and forty-eight duplicate studies were removed, and titles and abstracts were screened. Two hundred and seventy-five articles were excluded due to insufficient data published, patients undergoing procedures other than ESS, and review articles. Twenty-one articles were included from a manual search of references. In completion, 30 full-text articles were included in this review. A PRISMA diagram is demonstrated in Figure 1.
Quality/risk of bias assessment
Patient selection
Patient selection in studies included was relatively uniform. Study candidates were recruited from within ENT outpatient departments, with known CRS requiring operative intervention. There is a risk of selection bias in non-randomized trials outlined in Table 1, where it is unclear why certain patients underwent the interventions investigated. Overall, patients included met the search criteria for this review article, however, there is concern for selection bias in some studies, as outlined. Patients were randomised in the majority of studies, however, there were a number of studies in which patients were not enrolled in a consecutive manner.
Table 1
| Authors | Patient selection | Index test | Reference standard | Flow and timing |
|---|---|---|---|---|
| Friedman, Landsberg (15) | Low risk: consecutive enrolment of patients | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Hegazy, Shawky (16) | Low risk: consecutive enrolment, RCT | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Hewitt and Orlandi (19) | Unclear: unclear how patients were chosen from cohort of patients undergoing conchopexy | High risk: not blinded. No indication of what degree of synechiae formation was “significant” | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Dutton and Hinton (18) | Low risk: consecutive enrolment of patients | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Chen, Wang (17) | Low risk: consecutive enrolment of patients | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Wong and Singh (20) | Low risk: consecutive enrolment of patients | High risk: not blinded. No indication of what degree of synechiae formation was “significant” | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Shikani (25) | Low risk: consecutive enrolment of patients | High risk: not blinded. No indication of what degree of synechiae formation was “significant” | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Lee and Lee (24) | High risk: patients enrolled all had floppy MTs intraoperatively | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Baguley, Stow (21) | Low risk: consecutive enrolment. Patients blinded | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. All results included |
| Chan, Elmiyeh (22) | Low risk: consecutive enrolment. Patients blinded | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Gall and Witterick (23) | Unclear: unclear how patients were recruited | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Bugten, Nordgard (27) | Low risk: consecutive enrolment of patients | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Kastl, Betz (28) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Valentine, Athanasiadis (33) | Low risk: consecutive enrolment of patients | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Wormald, Boustred (34) | Low risk: consecutive enrolment of patients | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Miller, Steward (30) | Low risk: consecutive enrolment of patients | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Berlucchi, Castelnuovo (26) | Low risk: consecutive enrolment of patients | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Szczygielski, Rapiejko (32) | Low risk: consecutive enrolment of patients | Unclear: unclear whether authors were blinded | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Marple, Smith (29) | Low risk: consecutive enrolment. Patients blinded | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Murr, Smith (31) | Low risk: consecutive enrolment. Patients blinded | Low risk: surgeons blinded to clinical information of patient | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Woodworth, Chandra (38) | Low risk: consecutive enrolment. Patients blinded | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Shi, Zhou (37) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Kim, Lee (35) | Unclear: unclear how patients were enrolled | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Beidlingmaier (39) | Unclear: unclear how patients were enrolled | High risk: surgeon not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Gulati, Wadhera (41) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Havas and Lowinger (42) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Toffel (45) | Low risk: consecutive enrolment of patients | High risk: surgeon not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Hudon, Wright (43) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Shih, Chin (44) | Low risk: consecutive enrolment of patients | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
| Brescia, Pavin (40) | High risk: patients enrolled with phenotypically more severe disease | High risk: surgeons not blinded in post-operative endoscopic evaluations | Low risk: objective evidence of synechiae formation documented | Low risk: appropriate follow-up period. No loss to follow-up. All results included |
RCT, randomized controlled trial.
Index test(s)
Investigative techniques were described adequately in each of the studies, and reproducible in clinical practice. There were clear objective measures in a large proportion of studies. However, observer bias is of concern in the non-blinded studies and trials included in this review. There were varied investigative techniques within each MiTLAF prevention technique. Varied suture material for conchopexy, varied preparations for hyaluronic acid packing, and varied absorbable middle-meatal spacer choices lead to concerns for intervention bias.
Reference standard
The reference standard for most of the studies was the practice of normal ESS without employing any MiTLAF prevention techniques. However, there was a small subset of studies which compared two separate MiTLAF prevention techniques without comparison against a reference standard (no prevention technique). Given this, the true effect of MiTLAF prevention in comparison with the reference standard is unable to be effectively determined, and in this small number of studies, there remains low level of concern for outcome reporting bias.
Flow and timing
Across all interventions, there appears to have been an appropriate length of follow-up of at least 2 months for patients post-intervention which would accurately represent the time frame in which post-operative synechiae formation and resultant symptoms could be expected. The exception to this being a select few studies which investigated different middle meatal spacers where the spacers were potentially removed prematurely; this is discussed later in this review. With regard to potential selection bias, it is reassuring that in all studies, unless patients were lost-to-follow-up, all study candidates were included in the published results to more accurately reflect the accuracy of the proposed interventions. As such, the risk of bias from this perspective appears relatively low.
In the studies reviewed, authors described several methods to prevent MiTLAF, including forced medialisation techniques (“Bolgerisation” and conchopexy), splint placement, middle meatal spacers (absorbable and non-absorbable), and middle turbinectomy. Table 2 lists the results for the studies identified, grouped according to technique. We review the literature for each technique in detail below.
Table 2
| Authors | Type of study | MiTLAF prevention method | Study size (number of patients) | Significant synechiae incidence (%) at time of last follow-up | Potential adverse outcomes quoted (%) |
|---|---|---|---|---|---|
| Friedman, Landsberg (15) | NRCT | Bolgerisation | 500 | 7 | Nil reported |
| Hegazy, Shawky (16) | RCT | Conchopexy | 36 | 0 | Nil reported |
| Bolgerisation | 15 | Nil reported | |||
| Hewitt and Orlandi (19) | Retrospective review | Conchopexy | 85 | 10.8 | Nil reported |
| Dutton and Hinton (18) | Prospective cohort study | Conchopexy | 153 | 8 | Nil reported |
| Chen, Wang (17) | Prospective RCT | Conchopexy | 60 | 3.3 | Nil reported |
| Wong and Singh (20) | Case series | Conchopexy | 25 | 8 | Nil reported |
| Shikani (25) | Case series | Silastic Splint | 50 | 4 | Nil reported |
| Lee and Lee (24) | Prospective cohort study | Silastic Splint | 30 | 6 | Nil reported |
| Baguley, Stow (21) | RCT | Silastic Splint | 42 | 0 | Nasal obstruction (3) |
| Discomfort (2.9) | |||||
| Chan, Elmiyeh (22) | RCT | Silastic Splint | 35 | 8 | Nil reported |
| Gall and Witterick (23) | Prospective case series | Silastic Splint | 500 | 4.2 | Nil reported |
| Bugten, Nordgard (27) | Partly-blinded RCT | Middle Meatal Spacer (NAS; Merocel) | 61 | 11 | Minor bleeding (9.7) |
| Kastl, Betz (28) | RCT | Middle Meatal Spacer (AS; CMC) | 41 | 3.8 | Nil reported |
| Valentine, Athanasiadis (33) | RCT | Middle Meatal Spacer (AS; Chitosan/Dextran Gel) | 40 | 5.3 | Nil reported |
| Wormald, Boustred (34) | Single-blinded RCT | Middle Meatal Spacer (AS; MeroGel) | 42 | 16.7 | Nil reported |
| Miller, Steward (30) | Blinded RCT | Middle Meatal Spacer (AS; MeroGel) | 37 | 19 | Nil reported |
| Middle Meatal Spacer (NAS; Merocel) | 19 | Nil reported | |||
| Berlucchi, Castelnuovo (26) | Multi-centre RCT | Middle Meatal Spacer (AS; MeroGel) | 66 | 4.5 | Nil reported |
| Szczygielski, Rapiejko (32) | Prospective cohort study | Middle Meatal Spacer (AS; CMC) | 60 | 15.4 | Bleeding (13.3) |
| Middle Meatal Spacer (NAS; Merocel) | 35.7 | Bleeding (6.7) | |||
| Marple, Smith (29) | RCT | Middle Meatal Spacer (PROPEL with steroid) | 105 | 4.8 | Nil reported |
| Murr, Smith (31) | RCT | Middle Meatal Spacer (PROPEL with steroid) | 38 | 5.3 | Nil reported |
| Woodworth, Chandra (38) | RCT | Hyaluronic Acid/CMC | 53 | 17.8 | Nil reported |
| Shi, Zhou (37) | RCT | Absorbable Hyaluronan hydrogel | 54 | 20.3 | Nil reported |
| Kim, Lee (35) | Prospective cohort study | Hyaluronic Acid/CMC | 26 | 4.5 | Nil reported |
| Beidlingmaier (39) | Retrospective review | Partial MTR | 80 | 3.2 | Bleeding (3.8) |
| Acute pain (11.2) | |||||
| Anosmia/Dysgeusia (1.3) | |||||
| Gulati, Wadhera (41) | RCT | Partial MTR | 40 | 5 | Nil reported |
| Havas and Lowinger (42) | NRCT | Partial MTR | 1,106 | 0 | Nil reported |
| Toffel (45) | Cohort study | Partial MTR | 2,954 | 2.5 | Bleeding (0.12) |
| Hudon, Wright (43) | RCT | Partial MTR | 15 | 0 | Nil reported |
| Shih, Chin (44) | Prospective cohort study | Partial MTR | 31 | 16.1 | Nil reported |
| Brescia, Pavin (40) | Retrospective cohort study | Partial MTR | 48 | 0 | Nil reported |
MiTLAF, middle turbinate lateralisation and adhesion formation; NAS, non-absorbable spacer; AS, absorbable spacer; NRCT, non-randomized controlled trial; RCT, randomized controlled trial; CMC, carboxymethylcellulose; MTR, middle turbinate resection.
Bolgerisation
First described and published by Bolger et al. in 1999, “controlled” medial synechiae formation (Bolgerisation) is purposeful creation of mucosal abrasions on the medial surface of the anteroinferior MT and adjacent nasal septum (14). Abrasions are matched to encourage local adhesion formation, securing the middle turbinate medially and preventing lateralisation. Some surgeons reinforce Bolgerisation with insertion of dissolvable or non-dissolvable nasal packing in the middle meatus, thereby bringing the abraded surfaces into closer contact.
Friedman et al. investigated 500 patients whose ESS procedures included Bolgerisation (15). This study yielded a 93% success rate with regard to MT medialisation and prevention of lateralisation. Patients with successful medialisation and without lateral synechiae were less likely to suffer from nasal obstruction postoperatively than those whose medialisation was unsuccessful (94% vs. 58%), however, the statistical significance of this finding was not reported (15).
Synechiae prevention was further investigated by Hegazy et al. in a RCT of 39 patients. Patients were randomised to one of three arms of investigation:conchopexy vs. Bolgerisation vs. no MiTLAF prevention measures (control arm). Pre- and post-operative endoscopic assessment was performed on each patient, assessing for: inflammatory oedema of the OMC; presence of mucopus in the middle meatus; and presence of synechiae, with each endoscopic measure quantified on a 0-2 basis (0 = not present, 1 = present, 2 = marked) and all three scores added together to give a final figure. Mean post-operative scores of patients in whom Bolgerisation or conchopexy (described later in the manuscript) was performed were significantly reduced when compared with their pre-operative scores (1.15±1.28 vs. 3.46±1.45 respectively, P<0.05) (16). Synechiae rates were decreased in the bolgerisation group in comparison with the control arm (15% vs. 38%, P value not reported) and there were no synechiae reported in patients of the conchopexy group, with the statistical significance not reported.
Concerns have been raised regarding Bolgerisation—removal of packing in the post-operative period may cause epistaxis, as well as trigger vasovagal reactions. As with conchopexy, iatrogenic hyposmia is a potential concern raised. Olfactory neuroepithelium is located superiorly in the nasal cavity, found in the mucosa of the superior turbinate, superolateral nasal wall and septum. Medialisation procedures may reduce regional nasal airflow and odorant particulate deposition (46). However, objective evidence for this postulated complication is limited, with only a few cases described (47-52). The two studies described above did not report any cases of hyposmia.
Conchopexy
Conchopexy involves MT medialisation via temporary suture placement, attaching the MT to the septum. While at times technically difficult to perform, it may mitigate the nasal obstruction and discomfort associated with nasal packing (and subsequent removal, if required) experienced by patients in whom Bolgerisation (with packing) has been used. Hewitt et al. demonstrated the efficacy of this technique in 2009 with lateral synechiae found in 10.8% of patients (19).
In addition to the Bolgerisation technique, Hegazy et al., 2015, also investigated conchopexy for MiTLAF prevention. As previously described, this study investigated inflammatory oedema of the OMC, presence of mucopus in the middle meatus, and presence of synechiae pre- and post-operatively in patients undergoing ESS. Mean post-operative endoscopic grading score was significantly reduced (lower = better) in the conchopexy arm when compared with pre-operative endoscopic grading (0.77±0.83 vs. 4±1.53 respectively, P<0.05) (16). The rate of MiTLAF in the conchopexy cohort was reportedly lower than in the control arm which had no MiTLAF prevention method (0% vs. 38%), however, statistical significance was not reported. In addition to mitigation of MiTLAF risk, conchopexy was also associated with complete resolution of OMC mucopus findings 2 months post-operatively. In comparison, 40% of control subjects still had OMC mucopus 2 months post-operatively (statistical significance not reported).
Chen et al. investigated MiTLAF incidence in patients with a study design comparing nasal-packing alone (control) and conchopexy with nasal-packing (intervention) in 120 patients. The packing material chosen was Nasopore (Polyganics; Rozenburglaan, Groningen, the Netherlands), a biodegradable, absorbable material. MT lateralisation was significantly reduced in the intervention arm in comparison control at 3 months post-operatively (5% vs. 15.8%; RR not quoted; P<0.05). Additionally, synechiae formation rates were lower in the intervention arm in comparison with the control (3.3% vs. 10.8%; RR not quoted, X2 test; P<0.05) (17).
Conchopexy technique has recently been described by Wong et al. in 2018 (20). In this cohort of 25 patients, a novel, simplified conchopexy technique was described with 2 (8%) patients developing lateral synechiae, of which 1 underwent simple adhesiolysis in the outpatient setting, and the other patient remained asymptomatic without any further intervention (20). The authors postulated that conchopexy technique and choice of suture material (secondary to time for suture dissolution in-vivo) may influence MiTLAF prevention.
Similar to Bolgerisation, concerns have been raised regarding possible iatrogenic hyposmia. Interestingly, in a study of 85 patients by Dutton and Hinton, patients experienced improved olfactory outcomes, measured with University of Pennsylvania Smell Identification Test (UPSIT) scores, with lateral synechiae formation rate reported as 8% (mean increase in UPSIT score from 35 to 36, P<0.05) (18). It is unclear whether this result is clinically significant with the low number of study participants, and low absolute change in UPSIT scores. Notably, anatomic obstructions such as sinonasal polyps, particularly around olfactory cleft, may result in hyposmia/ anosmia by limiting nasal airflow to olfactory neuroepithelium. In these patients, FESS alone, independent of MT medialisation, can often improve subjective nasal olfactory measures (46).
Middle meatal/nasal splint placement
Another method of MT medialisation is silastic splints/stents placement between the MT and lateral nasal wall. This intervention aims to leave olfaction unaffected, however may temporarily affect nasal aerodynamics in the early postoperative period.
Originally described by Shikani in 1994, middle meatal stent placement was found to be effective in prevention of middle meatal synechiae in 50 patients who underwent middle meatal antrostomies (25). In each patient, one side was left without stent placement (control), and a silicone stent was placed in the contralateral side between the MT and lateral nasal wall (intervention). Following stent removal 10 to 14 days post-operatively, at the time of long-term follow-up (mean 8.2 months), significant middle meatal synechiae were seen in the control nasal passage of 18% (9/50) of patients compared to only minor synechiae found in 4% (2/50) on stented sides (statistical significance not reported) (25). Further follow-up of these patients demonstrated 5 of the 9 patients with significant synechiae developed closure of the middle meatal antrostomy with recurrence of disease. However, it was not mentioned at what stage following initial follow-up this occurred. There was no report of the effect of middle meatal synechiae on other sinus ostia such as the frontal recess or anterior ethmoid (25).
Lee, in 2007, confirmed these findings in a cohort of 30 patients; 15 patients were randomized to receive silastic splint placement, while the remaining 15 patients received no synechiae prevention technique. Lateral synechiae formation was lower in those with splinted patients than in the control population (6% vs. 44%; Relative risk χ2=4.15; P=0.02) (24).
Baguley et al. similarly found reduction in lateral synechiae formation with silastic splint placement in 2012 with a study cohort of 38 patients. At 12-week follow-up, no splinted nasal passages developed lateral synechiae, while 27% of unsplinted nasal passages developed middle meatal synechiae (21). No association was found between Lund-Kennedy endoscopic scores (LKES) and presence of synechiae for patients with unilateral synechiae in this study (LKES, 2.0 vs. 1.2; Z0=1.466; P=n.s.) (21). No statistically significant difference between symptoms or ethmoid cavity scores were seen at 12-week post-operatively (21).
Chan et al. conducted a RCT in 2015 investigating silastic stent placement in MiTLAF prevention in a cohort of 35 patients; secondary outcomes included post-operative facial pain, nasal obstruction and bleeding. Stented sides demonstrated a statistically significant decrease in MiTLAF rate at both 2 weeks (8% vs. 64%; OR =0.01; 95% CI: 0.0002 to 0.10; P<0.05) and 8 weeks (8% vs. 61%; OR =0.02; 95% CI: 0.003 to 0.12; P<0.05) post-operatively. Secondary outcomes of post-operative pain, nasal obstructive symptoms and bleeding were indistinguishable between study sides (P=n.s) (22). This study was modelled after a prospective case series by Gall and Witterick in 2004 which utilised an identical silastic sheet technique performed in a cohort of 500 patients, which reported synechiae formation in 4.2% of its cohort (23).
Middle meatal spacers
Middle meatal spacers are another method of post-operative care utilised for post-ESS MITLAF prevention. Both absorbable spacers (AS) and nonabsorbable spacers (33) are available, however, there is currently no consensus as to which material results in optimal outcomes. Merocel (Medtronic Inc., Xomed, Minneapolis, MN, USA) is a commonly used NAS. AS include MeroGel (Medtronic Inc., Xomed, Minneapolis, MN, USA), Nasopore (Polyganics; Rozenburglaan, Groningen, the Netherlands), Sinu-foam (Smith & Nephew, Hull, UK), Sepragel Sinus (Genzyme Biosurgery, Union City, CA, USA) and FloSeal (Baxter International Inc., Deerfield, IL, USA). Of particular note, while FloSeal is traditionally marketed as a haemostatic agent, some surgeons and studies have advocated its efficacy as a middle meatal spacer to prevent MiTLAF.
Bugten et al. in 2006 performed a randomised, controlled, partly-blinded study consisting of 59 patients assessing the effect of nonabsorbable middle meatal packing, specifically focussed on synechiae rates. Thirty-one patients received middle meatal packing with Merocel for 5 days. Twenty-eight patients received daily saline irrigations alone as a control. Synechiae rates were significantly lower in the treatment arm in comparison with the control (11.3% vs. 53.7%, P<0.05) (27). A comparative study by Miller et al. in 2003 examined synechiae rates in 37 patients whereby participants were randomized to receive nonabsorbable Merocel packing in one operated side, and absorbable MeroGel in the contralateral side. Synechiae rates at time of last follow-up were comparable (19% vs. 19%, P=n.s.); a non-significant short-term trend was seen with MeroGel-packed cavities yielding higher rates of significant synechiae requiring in-office adhesiolysis (RR 1.67; 95% CI: 0.48–5.76; P=n.s.) (30). Szczygielski et al. similarly published a comparative study investigating NAS and AS synechiae rates, using absorbable carboxymethylcellulose (CMC) rather than MeroGel. A non-significant trend was seen with NAS placement demonstrating lower synechiae rates at time of last follow-up (6.7% vs. 35.7%, P=n.s.) (32).
The AS with the most evidence in the literature is Merogel. Wormald et al. in 2006 demonstrated in a blinded RCT consisting of 42 patients there was no statistically significant benefit in Merogel AS placement when compared with the control arm (no spacer) at time of last follow-up (16.7% vs. 19%, P=n.s.) (34). Conversely, a significant reduction in synechiae rates was yielded with Merogel packing in the study published by Berlucchi et al. in 2009. In 66 patients, Merogel packing was found to be superior to control sinus cavities with no packing (4.6% vs. 29.7%, P<0.001) (26).
Other absorbable spacers have been investigated, but the literature available is more limited. CMC spacer placement, investigated by Kastl et al. in 2009, did not yield any significant benefit in synechiae prevention in comparison with standard surgery without spacer placement in 27 patients (4% vs. 0%, P=n.s.) (28). Chitosan/Dextran Gel, however, was effective in a study published by Valentine et al. in 2010. In the 40 patients included in this RCT, there was a statistically significant reduction in synechiae formation (5% vs. 30%, P<0.05); no significant complications from AS placement were reported (33).
Steroid-eluting spacers are also an area of new research. Two recent papers demonstrated their efficacy in post-operative synechiae prevention. Murr et al., in 2011, conducted a double-blinded RCT investigating a novel mometasone-eluting absorbable stent (PROPEL, Intersect ENT, Palo Alto, CA) in comparison with a non-drug-eluting absorbable stent with a cohort of 38 patients. The treatment arm demonstrated a significant reduction seen in synechiae rates (5.3% vs. 21.1%, P<0.05) at time of last follow-up, 60 days post-operatively (31).
These findings were further validated in the ADVANCE II multi-centre RCT conducted by Marple et al. in 2012, utilising the same spacer in a larger cohort of 105 patients. There was a demonstrable reduction in synechiae formation in the treatment arm (4.8% vs. 12.5%, P<0.05), correlating with findings reported by Murr et al. (29,31).
Hyaluronic acid-soaked packing
Hyaluronic acid plays an essential role in physiological homeostasis of the airways, specifically with building and stabilization of extracellular matrices and increased type III collagen (36). Therefore, hyaluronic acid-soaked packing may prevent synechiae formation by expediting wound healing and mucosal re-epithelialisation (37).
Kim et al. were among the first research groups to investigate the role of hyaluronic acid-impregnated packing in synechiae prevention. The authors’ study in 2007 compared hyaluronic acid-impregnated CMC spacers with Merocel spacers in a small cohort of 24 patients—there was a demonstrable reduction in synechiae rates in the hyaluronic acid arm in comparison with patients packed with Merocel at time of last follow-up (3% vs. 18%, P<0.05). Complications were not reported (35). Woodworth et al. similarly investigated synechiae rates with impregnated CMC against a control arm, with no packing/spacer placement, in an RCT of 53 patients. There was no significant benefit seen (82% vs. 71%, P=n.s.) (38). Finally, Shi et al. in 2013 compared synechiae formation rates whereby each patient received Merocel packing on one side (control), and hyaluronic acid gel on the contralateral side (intervention). At 12 weeks’ follow-up there were significantly less obstructive synechiae (0% vs. 7.41%, P<0.05) as well as nonobstructive synechiae (20.4% vs. 46.3%, P<0.05) in the intervention group (37).
Middle turbinate resection (MTR)
MTR is a controversial technique in MiTLAF prevention. Proponents report the technique results in increased space at the OMC (42,45). Other authors favour middle turbinate preservation (MTP) due potential risk of frontal recess stenosis, as well as atrophic rhinitis or “empty nose syndrome” (39,53,54). These authors suggest that MTP maintains the natural anatomy and preserves innate nasal aerodynamics, although there is limited objective evidence assessing this contention (41).
Havas and Lowinger demonstrated in 2000 a significant benefit from MTR in comparison with MTP in a cohort of 1,106 patients (509 patients with MTR and 597 patients without MTR). At 12 months’ post-ESS, synechiae formation was significantly reduced in the MTR cohort (0% vs. 8.5% respectively, P<0.05). Furthermore, the rate of revision surgery was reduced in patients who underwent MTR vs. MTP (7.1% vs. 15.6%, P<0.05). There were no significant complications from MTR reported (42).
Toffel advocated for MTR quoting a synechiae incidence rate of 2.5% in a cohort of 2,954 cases of ESS. All patients with synechiae required revision ESS for recalcitrant sinus disease (45). A commonly raised concern by surgeons is the potential for intraoperative/post-operative bleeding with MTR. Toffel reported minimal adverse outcomes, with 0% intraoperative haemorrhage causing premature termination of the procedure, and 0.12% experiencing post-operative haemorrhage requiring blood-transfusion (45). Unfortunately, the quantity of bleeding required for premature termination of the procedure was not reported, nor were indications for post-operative blood transfusion.
Gulati et al. in 2010 performed a retrospective analysis of 40 patients comparing middle meatal antrostomy (MMA) alone, against MMA with partial MTR in the assessment of post-operative outcomes both subjectively and objectively. MTR and MMA was associated with significantly reduced synechiae formation when compared to MMA alone (5% vs. 25% respectively, P<0.05) (41). Subjectively, patients noted improved nasal obstructive symptoms, rhinorrhoea, headache, post-nasal drip, and sneezing, in comparison with MMA alone. Patients were surveyed with “yes/no” questionnaires indicating whether symptoms had improved post-operatively; the paper did not provide numerical data to quantify the degree of improvement in symptoms (41).
Most recently, Hudon et al. investigated a small cohort of patients (n=15) comparing MTR and MTP using post-operative LKES scores as well as specifically investigating incidence of synechiae formation. While transient differences were seen between each investigation arm, long-term outcomes at 6 months were similar regarding LKES scores (1.7±1.5 vs. 1.7±1.6, P=n.s.). No statistically significant difference in synechiae formation between the two techniques was reported, which may relate to the study’s low power (MTP 20% vs. MTR 0%, P=n.s.) (43).
Discussion
This study reviews the efficacy and safety of various MiTLAF prevention techniques. Due to the lack of appropriately-powered, high-quality studies and significant study design and outcome data heterogeneity, meta-analysis could not be performed.
Efficacy
Based on the reviewed literature, the most effective techniques in preventing MiTLAF were silastic splints (MiTLAF rate range 0–8%) (21-25) and MT conchopexy (0–10.8%) (16-20). Variability in conchopexy efficacy has been postulated to be, at least in part, due to type of suture material-sutures such as Monocryl which have a longer time for dissolution, and higher tensile strength are thought to be ideal (20).
Bolgerisation was reasonably efficacious from the two studies included (10–15%) (15,16). The lower synechiae rate in the study by Friedman et al. was thought to be due to the use of a microdebrider rather than the conventional sickle knife for creating matched abrasions (15). The sparse literature limits further analysis on the efficacy of this technique.
Post-operative topical intranasal corticosteroids appear to improve post-operative endoscopic scores, however the evidence is of low-quality from 7 studies included in a systematic review and meta-analysis by Fandiño et al. in 2013 (55). The use of post-operative systemic corticosteroids however has been shown to improve post-operative healing and reduce early disease recurrence, particularly in those with polypoid disease (56). Steroid-eluting absorbable spacers appear to be very effective (4.8–5.3%), however available literature is limited (29,31). Drug-eluting stents could be of particular utility in patients requiring ESS, with the scope to mitigate the risks of systemic corticosteroid therapy.
Less effective techniques evaluated were NAS (8.1% to 35.7%) (27,30,32) and other AS, including hyaluronic acid (3.8–20.3%). In the study by Szczygielski et al. which reported 35.7% post-operative synechiae, packing was removed after only 24 hours. Conversely, the studies by Miller et al. and Bugten et al. reported considerably lower synechiae rates at 19% and 11% respectively, when packing was removed 5–7 days post-operatively (27,30,32). NAS left in-situ for greater than 24 hours seem to be more effective in synechiae prevention, however, given the limited literature with standardised time left in-situ in patients, further research is required to validate these findings.
Merogel, a hyaluronic-acid based hydrogel appears to have the greatest evidence base amongst AS. Results are variable however, with synechiae rates ranging from 4.5% to 16.7% (26,30,34). Other hyaluronic acid preparations have been trialled as well, with rates ranging from 4.5% to 20.3% (30,35,37,38). The authors of these papers postulated differences in preparations as contributing factors to success rates; given this heterogeneity in study designs, it is difficult to ascertain the reproducible efficacy.
From the 7 studies reviewed, there is significant evidence that MTR results in reduced synechiae rates ranging from 0–16.1% (39-45). The highest rate was reported by Shih et al. in a prospective study with 16.1% of the 31 patients developing post-operative synechiae. The authors’ description of methodology and outcome measures was limited, and did not mention whether patients performed post-operative sinus douching as part of their post-operative care (44).
Safety
Reporting of complications was inconsistent between studies and difficult to compare. Where documented, complication rates were generally reported to be low, but, particularly with the retrospective studies, may have been underreported. Minor complications included post-operative nasal obstruction; this was only reported in one study investigating silastic splints, and was relatively uncommon (3%) (21). Major complications reported in studies pertained to post-operative bleeding. Post-operative bleeding was reported in one AS study (13.3%) (32), two NAS studies (6.7% and 9.7%) (27,32), and two MTR studies (0.12% and 3.8%) (39,45). In general, reporting on post-operative complication rates was sparse in articles included in this review. The true incidence of complications for each technique is likely underepresented in the data available, either due to poor study design or the retrospective nature of many of the studies. Prospective studies, with careful documentation of complications is recommended.
Concerns have been raised that Bolgerisation and conchopexy may lead to aberrant nasal airflow and hyposmia (15,18,57). This has not been observed in the studies reviewed but requires further investigation.
Ease of use
Ease-of-use was not reported and is difficult to compare across techniques. In general, it is assumed the simplest techniques include AS and NAS placement. Silastic splints need to be sutured in place, which increases difficulty. Bolgerisation requires using a debrider or knife with precisely matched abrasions to be successful. Conchopexy has been reported to be technically challenging. Wong and Singh described a novel technique reportedly reducing some of these challenges with the suture knot tied at the caudal septum rather than endonasally at the MT (20). MTR is technically not challenging to incorporate intraoperatively, however it would impact any revision procedures a patient may need as it is an important anatomical landmark during ESS (58).
Patient discomfort
Patient discomfort was not consistently reported in the literature, however appears to be greatest with MTR, with 11.2% of patients reporting acute post-operative pain in one study (39). These findings were not reported, or corroborated, in other MTR papers reviewed.
Post-operative discomfort was reported in 2.9% of patients in only one study investigating silastic splints (21).
Summary
The findings of this review are summarized in Table 3. It appears that the techniques that are most efficacious, safe, easy for surgeons to utilise, and create the least discomfort for patients include MT conchopexy and silastic splints. Steroid-eluting absorbable spacers appear efficacious and safe but have limited supporting evidence. MTR also yields low synechiae rates, however, the majority of supporting literature for MTR employed non-consecutive patient enrolment and is subject to selection bias (43). MTR may potentially have negative effects on sinonasal physiology, particularly sinus ventilation patterns and olfaction, effects which have not yet been objectively assessed. As mentioned previously, MTR also renders revision procedures to be more difficult. Further research to objectively investigate these outcomes are indicated if it is to achieve wider acceptance amongst surgeons.
Table 3
| MiTLAF prevention method | Number of studies (n) | Synechiae rates at time of last follow-up (%) | Potential adverse outcomes quoted (%) | Other considerations |
|---|---|---|---|---|
| Bolgerisation | 2 | 10–15 | Nil | |
| Conchopexy | 5 | 0–10.8 | Nil | Technically challenging |
| Silastic splints | 5 | 0–8 | Nasal obstruction (3) | |
| Discomfort (2.9) | ||||
| MM spacers | 9 | AS: 3.8–20.3 | Bleeding (6.7–13.3) | |
| NAS: 8.1–35.7 | ||||
| Hyaluronic acid | 5 | 4.5–20.3 | Nil | |
| MT resection | 7 | 0–16.1 | Bleeding (0.12–3.8) | Increase difficulty for revision surgery |
| Acute pain (11.2) | ||||
| Anosmia/Dysgeusia (1.3) |
MiTLAF, middle turbinate lateralisation and adhesion formation; MM, middle meatal; MT, middle turbinate.
Limitations
This paper aimed to systematically review the literature regarding operative techniques in MiTLAF prevention. Unfortunately, there are limited high-quality, large-cohort, randomised, controlled studies. Multiple papers included are non-blinded and thus subject to observation bias. Final included studies included a large proportion of studies from bibliographic search and further studies may have been discovered with a broader search strategy. It is difficult to draw meaningful conclusions from the data, however, they do provide some insight as to area(s) of research to further validate the findings.
There is significant heterogeneity in study designs between each technique, however there is also significant variability in quality of studies of the same technique, particularly with middle meatal spacers; this limits comparison between techniques and products. Nevertheless, the evidence does indicate that some spacer materials are effective in MiTLAF prevention; these include steroid-eluting splints, MeroGel, CMC gel, and chitosan gel.
Future studies
Further research with comparative RCT studies in the investigation of MiTLAF prevention techniques is required to facilitate meta-analysis and identify the ideal technique. This is particularly important given the abundance of middle meatal spacers available. Uniform reporting of outcomes would facilitate meta-analysis. The authors postulated varied conchopexy outcomes are at least partially secondary to suture material used, and further studies in this area could be of value. The role of middle meatal synechiae in recalcitrant sinus disease requires further investigation.
A novel tool recently used in rhinology to analyse nasal airflow and topical medication distribution is computational fluids dynamics (CFD). Computer modelling of sinonasal passages, and analysis of flows is providing greater understanding the complexity of sinonasal physiology. CFD analysis could help objectively model sequelae of altered nasal aerodynamics in patients with CRS, cast light on repercussion(s) of synechiae formation post-ESS, and their role in patients requiring revision surgery.
Conclusions
Systematic review of the literature indicates that silastic splints (0–8%) and middle turbinate conchopexy (0–10.8%), are the techniques that are most efficacious (lowest synechiae rates), safe, easy to use and well-tolerated by patients. Steroid-eluting absorbable spacers show significant promise (4.8–5.3%) but require more evidence. Bolgerisation is an effective method (10–15%), however, available literature is limited, and results may be subject to operative technique. Middle meatal spacers appear effective but less so than other techniques. Heterogenous study design and inconsistent reporting complicates analysis. Middle turbinate resection is effective (0–16.1%), however there are concerns regarding potential sequelae of altered sinonasal physiology with this practice. The strength of the study findings was limited by low-quality evidence and inconsistent reporting. Further research, including well-constructed RCTs directly comparing techniques using validated measures, is recommended.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-6/rc
Funding: The authors thank
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-6/coif). KI and NS received the Rodney Williams and Garnett Pass Memorial Foundation Conjoint grant 2019-2022 for financial support. RS is an unpaid member of the Federal Council of Royal Australasian College of Surgeons and he received payment from Avant Mutual for a medico-legal opinion unrelated to this manuscript. NS is a consultant for ResMed, Optinose, Nasus, GSK, and ENT Technologies, and receives grant funding from Microsoft. The other authors have no conflicts of interests to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe--an underestimated disease. A GA2LEN study. Allergy 2011;66:1216-23. [Crossref] [PubMed]
- Gross C, Schlosser R. Prevalence of economic impact of rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg 2001;9:8-10. [Crossref]
- Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology 2020;58:1-464. [Crossref] [PubMed]
- Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012;50:1-12. [Crossref] [PubMed]
- Noon E, Hopkins C. Review article: outcomes in endoscopic sinus surgery. BMC Ear Nose Throat Disord 2016;16:9. [Crossref] [PubMed]
- Nair S, Dutta A, Rajagopalan R, et al. Endoscopic sinus surgery in chronic rhinosinusitis and nasal polyposis: a comparative study. Indian J Otolaryngol Head Neck Surg 2011;63:50-5. [Crossref] [PubMed]
- Bhattacharyya N. Clinical outcomes after revision endoscopic sinus surgery. Arch Otolaryngol Head Neck Surg 2004;130:975-8. [Crossref] [PubMed]
- Shrime MG, Tabaee A, Hsu AK, et al. Synechia formation after endoscopic sinus surgery and middle turbinate medialization with and without FloSeal. Am J Rhinol 2007;21:174-9. [Crossref] [PubMed]
- Ramadan HH. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope 1999;109:27-9. [Crossref] [PubMed]
- Musy PY, Kountakis SE. Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol 2004;25:418-22. [Crossref] [PubMed]
- Otto KJ, DelGaudio JM. Operative findings in the frontal recess at time of revision surgery. Am J Otolaryngol 2010;31:175-80. [Crossref] [PubMed]
- Bassiouni A, Naidoo Y, Wormald PJ. Does mucosal remodeling in chronic rhinosinusitis result in irreversible mucosal disease?. Laryngoscope 2012;122:225-9. [Crossref] [PubMed]
- Henriquez OA, Schlosser RJ, Mace JC, et al. Impact of synechiae after endoscopic sinus surgery on long-term outcomes in chronic rhinosinusitis. Laryngoscope 2013;123:2615-9. [Crossref] [PubMed]
- Bolger WE, Kuhn FA, Kennedy DW. Middle turbinate stabilization after functional endoscopic sinus surgery: the controlled synechiae technique. Laryngoscope 1999;109:1852-3. [Crossref] [PubMed]
- Friedman M, Landsberg R, Tanyeri H. Middle turbinate medialization and preservation in endoscopic sinus surgery. Otolaryngol Head Neck Surg 2000;123:76-80. [Crossref] [PubMed]
- Hegazy MA, Shawky A, El Fouly MS, et al. Conchopexy of middle turbinate versus bolgarization in endoscopic sinus surgery. Egypt J Otolaryngol 2015;31:219-23. [Crossref]
- Chen W, Wang Y, Bi Y, et al. Turbinate-septal suture for middle turbinate medialization: a prospective randomized trial. Laryngoscope 2015;125:33-5. [Crossref] [PubMed]
- Dutton JM, Hinton MJ. Middle turbinate suture conchopexy during endoscopic sinus surgery does not impair olfaction. Am J Rhinol Allergy 2011;25:125-7. [Crossref] [PubMed]
- Hewitt KM, Orlandi RR. Suture medialization of the middle turbinates during endoscopic sinus surgery. Ear Nose Throat J 2008;87:E11. [PubMed]
- Wong E, Singh N. An Improved Method for Temporary Suture Medialisation of the Middle Turbinates following Endoscopic Sinus Surgery. Int J Otolaryngol 2018;2018:9093545. [Crossref] [PubMed]
- Baguley CJ, Stow NW, Weitzel EK, et al. Silastic splints reduce middle meatal adhesions after endoscopic sinus surgery. Am J Rhinol Allergy 2012;26:414-7. [Crossref] [PubMed]
- Chan CL, Elmiyeh B, Woods C, et al. A randomized controlled trial of a middle meatal silastic stent for reducing adhesions and middle turbinate lateralization following endoscopic sinus surgery. Int Forum Allergy Rhinol 2015;5:517-23. [Crossref] [PubMed]
- Gall RM, Witterick IJ. The use of middle meatal stents post-endoscopic sinus surgery. J Otolaryngol 2004;33:47-9. [Crossref] [PubMed]
- Lee JY, Lee SW. Preventing lateral synechiae formation after endoscopic sinus surgery with a silastic sheet. Arch Otolaryngol Head Neck Surg 2007;133:776-9. [Crossref] [PubMed]
- Shikani AH. A new middle meatal antrostomy stent for functional endoscopic sinus surgery. Laryngoscope 1994;104:638-41. [Crossref] [PubMed]
- Berlucchi M, Castelnuovo P, Vincenzi A, et al. Endoscopic outcomes of resorbable nasal packing after functional endoscopic sinus surgery: a multicenter prospective randomized controlled study. Eur Arch Otorhinolaryngol 2009;266:839-45. [Crossref] [PubMed]
- Bugten V, Nordgård S, Skogvoll E, et al. Effects of nonabsorbable packing in middle meatus after sinus surgery. Laryngoscope 2006;116:83-8. [Crossref] [PubMed]
- Kastl KG, Betz CS, Siedek V, et al. Effect of carboxymethylcellulose nasal packing on wound healing after functional endoscopic sinus surgery. Am J Rhinol Allergy 2009;23:80-4. [Crossref] [PubMed]
- Marple BF, Smith TL, Han JK, et al. Advance II: a prospective, randomized study assessing safety and efficacy of bioabsorbable steroid-releasing sinus implants. Otolaryngol Head Neck Surg 2012;146:1004-11. [Crossref] [PubMed]
- Miller RS, Steward DL, Tami TA, et al. The clinical effects of hyaluronic acid ester nasal dressing (Merogel) on intranasal wound healing after functional endoscopic sinus surgery. Otolaryngol Head Neck Surg 2003;128:862-9. [Crossref] [PubMed]
- Murr AH, Smith TL, Hwang PH, et al. Safety and efficacy of a novel bioabsorbable, steroid-eluting sinus stent. Int Forum Allergy Rhinol 2011;1:23-32. [Crossref] [PubMed]
- Szczygielski K, Rapiejko P, Wojdas A, et al. Use of CMC foam sinus dressing in FESS. Eur Arch Otorhinolaryngol 2010;267:537-40. [Crossref] [PubMed]
- Valentine R, Athanasiadis T, Moratti S, et al. The efficacy of a novel chitosan gel on hemostasis and wound healing after endoscopic sinus surgery. Am J Rhinol Allergy 2010;24:70-5. [Crossref] [PubMed]
- Wormald PJ, Boustred RN, Le T, et al. A prospective single-blind randomized controlled study of use of hyaluronic acid nasal packs in patients after endoscopic sinus surgery. Am J Rhinol 2006;20:7-10. [Crossref] [PubMed]
- Kim JH, Lee JH, Yoon JH, et al. Antiadhesive effect of the mixed solution of sodium hyaluronate and sodium carboxymethylcellulose after endoscopic sinus surgery. Am J Rhinol 2007;21:95-9. [Crossref] [PubMed]
- Macchi A, Terranova P, Digilio E, et al. Hyaluronan plus saline nasal washes in the treatment of rhino-sinusal symptoms in patients undergoing functional endoscopic sinus surgery for rhino-sinusal remodeling. Int J Immunopathol Pharmacol 2013;26:137-45. [Crossref] [PubMed]
- Shi R, Zhou J, Wang B, et al. The clinical outcomes of new hyaluronan nasal dressing: a prospective, randomized, controlled study. Am J Rhinol Allergy 2013;27:71-6. [Crossref] [PubMed]
- Woodworth BA, Chandra RK, Hoy MJ, et al. Randomized controlled trial of hyaluronic acid/carboxymethylcellulose dressing after endoscopic sinus surgery. ORL J Otorhinolaryngol Relat Spec 2010;72:101-5. [Crossref] [PubMed]
- Biedlingmaier JF. Endoscopic sinus surgery with middle turbinate resection: results and complications. Ear Nose Throat J 1993;72:351-5. [Crossref] [PubMed]
- Brescia G, Pavin A, Giacomelli L, et al. Partial middle turbinectomy during endoscopic sinus surgery for extended sinonasal polyposis: short- and mid-term outcomes. Acta Otolaryngol 2008;128:73-7. [Crossref] [PubMed]
- Gulati SP, Wadhera R, Kumar A, et al. Comparative evaluation of middle meatus antrostomy with or without partial middle turbinectomy. Indian J Otolaryngol Head Neck Surg 2010;62:400-2. [Crossref] [PubMed]
- Havas TE, Lowinger DS. Comparison of functional endonasal sinus surgery with and without partial middle turbinate resection. Ann Otol Rhinol Laryngol 2000;109:634-40. [Crossref] [PubMed]
- Hudon MA, Wright ED, Fortin-Pellerin E, et al. Resection versus preservation of the middle turbinate in surgery for chronic rhinosinusitis with nasal polyposis: a randomized controlled trial. J Otolaryngol Head Neck Surg 2018;47:67. [Crossref] [PubMed]
- Shih C, Chin G, Rice DH. Middle turbinate resection: impact on outcomes in endoscopic sinus surgery. Ear Nose Throat J 2003;82:796-7. [Crossref] [PubMed]
- Toffel PH. Secure endoscopic sinus surgery with partial middle turbinate modification: a 16-year long-term outcome report and literature review. Curr Opin Otolaryngol Head Neck Surg 2003;11:13-8. [Crossref] [PubMed]
- Wong EH, Do TQ, Harvey RJ, et al. Patient-reported olfaction improves following outside-in Draf III frontal sinus surgery for chronic rhinosinusitis. Laryngoscope 2019;129:25-30. [Crossref] [PubMed]
- Zhang Y, Zhou X, Lou M, et al. Computational Fluid Dynamics (CFD) Investigation of Aerodynamic Characters inside Nasal Cavity towards Surgical Treatments for Secondary Atrophic Rhinitis. Mathematical Problems in Engineering 2019;2019:6240320. [Crossref]
- Alam S, Li C, Bradburn KH, et al. Impact of Middle Turbinectomy on Airflow to the Olfactory Cleft: A Computational Fluid Dynamics Study. Am J Rhinol Allergy 2019;33:263-8. [Crossref] [PubMed]
- Zhao K, Jiang J, Pribitkin EA, et al. Conductive olfactory losses in chronic rhinosinusitis? A computational fluid dynamics study of 29 patients. Int Forum Allergy Rhinol 2014;4:298-308. [Crossref] [PubMed]
- Zhao K, Malhotra P, Rosen D, et al. Computational fluid dynamics as surgical planning tool: a pilot study on middle turbinate resection. Anat Rec (Hoboken) 2014;297:2187-95. [Crossref] [PubMed]
- Li C, Jiang J, Kim K, et al. Nasal Structural and Aerodynamic Features That May Benefit Normal Olfactory Sensitivity. Chem Senses 2018;43:229-37. [Crossref] [PubMed]
- Schroeter JD, Kimbell JS, Asgharian B. Analysis of particle deposition in the turbinate and olfactory regions using a human nasal computational fluid dynamics model. J Aerosol Med 2006;19:301-13. [Crossref] [PubMed]
- Morgenstein KM, Krieger MK. Experiences in middle turbinectomy. Laryngoscope 1980;90:1596-603. [Crossref] [PubMed]
- Thornton RS. Middle turbinate stabilization technique in endoscopic sinus surgery. Arch Otolaryngol Head Neck Surg 1996;122:869-72. [Crossref] [PubMed]
- Fandiño M, Macdonald KI, Lee J, et al. The use of postoperative topical corticosteroids in chronic rhinosinusitis with nasal polyps: a systematic review and meta-analysis. Am J Rhinol Allergy 2013;27:e146-57. [Crossref] [PubMed]
- Pundir V, Pundir J, Lancaster G, et al. Role of corticosteroids in Functional Endoscopic Sinus Surgery--a systematic review and meta-analysis. Rhinology 2016;54:3-19. [PubMed]
- Kim SW, Kim RB, Kang H, et al. Influence of a medialized middle turbinate on olfactory function: a prospective randomized double-blind study. Int Forum Allergy Rhinol 2019;9:473-8. [Crossref] [PubMed]
- Kennedy DW. Middle turbinate resection: evaluating the issues--should we resect normal middle turbinates? Arch Otolaryngol Head Neck Surg 1998;124:107. [Crossref] [PubMed]
Cite this article as: Khatri H, Wong E, Inthavong K, Sacks R, Singh N. Peri-operative measures to prevent middle turbinate lateralisation and adhesion formation in endoscopic sinus surgery—a systematic review of the literature. Aust J Otolaryngol 2022;5:20.