Magnetic resonance imaging evaluation of choanal atresia in newborns
Introduction
The diagnosis of choanal atresia (CA), either bilateral or unilateral, is initially made on clinical assessment and flexible nasendoscopy. Computed tomography (CT) is the accepted imaging modality for confirming the diagnosis and surgical planning, as it enables identification of the bony anatomy of the nasal airway and skull base (1). In a recent consensus recommendation from the International Paediatric Otolaryngology Group, all 28 members surveyed agreed pre-operative CT should be performed in all patients with CA and magnetic resonance imaging (MRI) should be performed in selected cases (2). Evidence linking a history of undergoing a CT in childhood, with an increased risk of benign and malignant brain tumours (3-5), has led to strategies to minimise the degree of radiation exposure in children with replacement of CT by MRI where feasible.
Only isolated case reports of the use of MRI in CA have been reported (6,7). We therefore undertook a proof-of-concept retrospective study of newborns and young children with CA who underwent both CT and MRI prior to their surgical repair, to evaluate whether the CT parameters required to plan surgery can also be determined by MRI. We present the following article in accordance with the STARD reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-8/rc).
Methods
A search was performed of all children under 12 months of age with bilateral or unilateral CA who underwent imaging studies at The Royal Children’s Hospital (RCH), Melbourne between 1 January 2010 and 1 May 2021. Potential cases were identified by search of radiology reports for mention of “choanal atresia”. Only patients who underwent both CT and MRI scan prior to surgery were included. While there is no consensus on which are the relevant parameters for CT evaluation in CA, we surveyed our department’s consultant paediatric otolaryngologists to identify descriptive and quantitative parameters that they regarded as surgically relevant. Using this checklist (Table 1), two radiologists separately evaluated either the CT or MRI scans. Scans were loaded onto the RCH picture archiving and communication system using anonymize test overlays prior to reporting to deidentify the patient and blind the radiologist. The scans were be loaded by an independent party employed by the RCH medical imaging department. Physical blocking measures were used to ensure deidentification and blinding was also used where the anonymize option was not adequate. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The project was approved by RCH Human Research Ethics Committee (No. HREC/76784/RCHM-2021) and individual consent for this retrospective analysis was waived.
Table 1
| Descriptive |
| 1. Bilateral or unilateral atresia |
| 2. Type of atresia: bony, membranous, or mixed |
| 3. Is there an intact skull base? |
| 4. Are there any other intranasal or postnasal pathologies? |
| 5. Are there any other congenital craniofacial anomalies? |
| 6. Are there temporal bone features suggestive of CHARGE association? |
| Quantitative |
| 7. Choanal height: narrowest distance between the horizontal plate of the palatine bone and the body of the sphenoid on coronal and sagittal views (mm) |
| 8. Choanal width: distance between the medial pterygoid and horizontal nasal midpoint on an axial view (mm) |
| 9. Skull base slope: angle between the line of the nasal floor and the line of the skull base (from anterior edge of the cribriform plate to ethmoidal spine of the sphenoid bone (degrees) |
mm, millimeters.
Statistical and data analysis
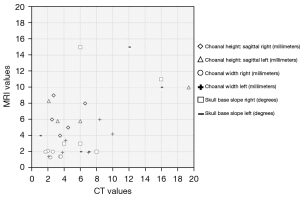
Qualitative data was compiled into a table. Quantitative data was plotted onto a scatter graph where x-axis was CT values and y-axis was the corresponding MRI value for each individual patient. Due to the small sample size, no trend line or correlation analysis was performed.
Results
Over the search period, there were 26 patients identified with CA, of which seven patients (four male, three female) were included in the study. The median age when CT and MRI scan was performed was 36 days (range, 2–410 days) and 56 days (range, 2–290 days), respectively. Two patients had bilateral and five had unilateral CA. Five patients had syndromes that included CHARGE association (two), Burn-McKeown (one), Treacher-Collins (one) and Jeune (one). Of the others, one had cleft palate and one had cleft lip.
Siemens Somatom definition flash 2×128 slice CT scanner was used for CT image acquisition. Non-contrast CT scans were performed to include a field of view from mid orbits to below the nasopharynx. Slice thickness of 0.75 mm was used with multi-planar bone and soft tissue reconstructions. Siemens Magnetom Prisma 3T MRI scanner was used for MRI image acquisition. Dedicated internal acoustic meatus (IAM) sequences performed only in one study. Studies were MRI brain studies with no dedicated imaging performed for the region of the nose and nasopharynx. General anaesthetic and intubation were required for CT in one patient and for MRI in two patients.
Table 2 shows the degree of agreement between CT and MRI findings for each descriptive assessment point. Figures 1,2 shows measurements of quantitative assessment points on axial and sagittal planes in MRI and CT for the same patient. Figure 3 depicts CT values of the quantitative dimensions plotted against the corresponding MRI value, where each symbol represents one patient.
Table 2
| Assessment point | Number of patients with agreement between imaging modalities (N=7) | Difference in findings across all patients |
|---|---|---|
| 1. Unilateral or bilateral | 7 | – |
| 2. Type of atresia | 0 | CT: mixed atresia in all studies |
| MRI: either bony or membranous in all studies | ||
| 3. Intact skull base | 7 | – |
| 4. Other intranasal or postnasal space pathology | 5 | CT reported: thick vomer, turbinate abnormalities, piriform aperture stenosis |
| 5. Other congenital craniofacial anomalies | 4 | CT reported: mid face hypoplasia, hypertelorism, coloboma, central incisor, shallow TMJ |
| MRI reported: absent septum pellucidum, thinned corpus callosum, dilated ventricles | ||
| 6. Temporal bone features suggestive of CHARGE association | 1 | MRI reported: generally unable to assess as no dedicated IAM views available |
CT, computed tomography; MRI, magnetic resonance imaging; TMJ, temporomandibular joint; IAM, internal acoustic meatus.
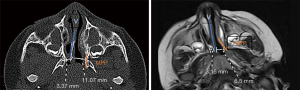
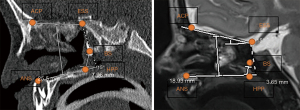
MRI did not enable choanal height to be assessed in the coronal view in any patients, and in one case, MRI was unable to determine skull base slope due to difficulty in assessing margins of the sphenoid bone. Movement artefact was noted on MRI in two cases. In one case, choanal height in sagittal view and choanal width could not be assessed by CT due to poorly defined pterygoids and slope of skull base due to cleft palate.
Discussion
The major surgical concern with CA surgery is the status of the skull base (8), which has been reported to be dehiscent in 3 of 53 CA patients (9). While MRI was able to assess for presence of intact skull base in agreement with CT, there were no cases with skull base defects due to the small sample size. Therefore, whether skull base defects can be identified on MRI has not been determined in our patient cohort. The use of high resolution, three-dimensional MRI has been described to evaluate the skull base (10) and this technique may further improve the capacity of MRI to assess the skull base in CA in future studies.
There is no consensus on which features on pre-operative imaging are surgically important. Messineo et al. (11) described several parameters on CT in patients with CA compared with a control group to identify helpful parameters for surgical planning. In children aged ≤1 year, choanal height, rostrum height, anterior interorbital distance, bone septum thickness, maximum septum length, posterior right bone width, posterior left bone width, bone width of choana and vertical distance of nasopharynx dimensions were all found to be significantly less in the study group compared with controls. Skull base slope was not assessed. There was no assessment of the utility of these parameters in a surgical setting. Fitzpatrick et al. (8) reported the choanal width, choanal height, mid-nasal skull base height and skull base slope in patients with isolated bilateral CA compared with CHARGE associated bilateral CA from CT, emphasising the importance of identifying steeply angulated bony trajectory which informs the surgeon of a lower skull base level posteriorly. In our study, we attempted to evaluate the minimum acceptable parameters to safely perform surgery in accordance with the discussion amongst our otolaryngology consultants. Choanal height, width and skull base slope were able to be assessed in most MRI scans. However, correlation between CT and MRI values could not be established.
There was some degree of agreement for presence of intranasal or post-nasal space pathology and other craniofacial anomalies. However, any deficiencies in this information could be supplemented by information derived by clinical assessment and flexible nasendoscopy. While MRI failed to agree with CT for CA type, given the knowledge that CA generally involves a major bony component, this inability is likely to have little clinical significance.
The inability of MRI in our study group to demonstrate CHARGE associated temporal bone abnormalities was due to absence of dedicated IAM images, which can be addressed by modifying the study algorithm.
The small sample size precluded statistical analysis of the relationship between CT and MRI to be made and no assessment of rater reliability was made. Furthermore, no established consensus exists regarding the imaging information required to ensure safety of endoscopic CA atresia repair. Nonetheless, this limited study has identified some of the issues that require further investigation, particularly by a prospective study combining CT with a targeted MRI study protocol in newborns with CA, to determine whether MRI could be used to replace CT.
Conclusions
Our study has demonstrated that MRI is able to assess some relevant surgical points in young children with CA. However, agreement and correlation between the gold-standard of CT is yet to be established and further prospective studies are required.
Acknowledgments
Data search: Ms Mita Pedersen, Chief Medical Imaging Technician, Medical Imaging Department, Royal Children’s Hospital Melbourne, Parkville, Victoria, Australia; Statistics advice: Associate Professor Susan Donath, Biostatistician, Clinical Epidemiology & Biostatistics, Murdoch Children’s Research Institute, University of Melbourne, Victoria, Australia.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-8/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-8/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-8/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-8/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The project was approved by RCH Human Research Ethics Committee (HREC/76784/RCHM-2021) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Petkovska L, Petkovska I, Ramadan S, et al. CT evaluation of congenital choanal atresia: our experience and review of the literature. Australas Radiol 2007;51:236-9. [Crossref] [PubMed]
- Moreddu E, Rizzi M, Adil E, et al. International Pediatric Otolaryngology Group (IPOG) consensus recommendations: Diagnosis, pre-operative, operative and post-operative pediatric choanal atresia care. Int J Pediatr Otorhinolaryngol 2019;123:151-5. [Crossref] [PubMed]
- Chen JX, Kachniarz B, Gilani S, et al. Risk of malignancy associated with head and neck CT in children: a systematic review. Otolaryngol Head Neck Surg 2014;151:554-66. [Crossref] [PubMed]
- Huang WY, Muo CH, Lin CY, et al. Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer 2014;110:2354-60. [Crossref] [PubMed]
- Li IG, Yang YH, Li YT, et al. Paediatric computed tomography and subsequent risk of leukaemia, intracranial malignancy and lymphoma: a nationwide population-based cohort study. Sci Rep 2020;10:7759. [Crossref] [PubMed]
- Black CM, Dungan D, Fram E, et al. Potential pitfalls in the work-up and diagnosis of choanal atresia. AJNR Am J Neuroradiol 1998;19:326-9. [PubMed]
- Keunen J, Chitayat D, Windrim R, et al. P30.05: Fetal MRI and 2D ultrasound imaging of unilateral choanal atresia in case of progressive unilateral ventriculomegaly, hypertelorism and nasal hypoplasia. Ultrasound Obstet Gynecol 2007;30:565. [Crossref]
- Fitzpatrick NS, Bartley AC, Bekhit E, et al. Skull base anatomy and surgical safety in isolated and CHARGE-associated bilateral choanal atresia. Int J Pediatr Otorhinolaryngol 2018;115:61-4. [Crossref] [PubMed]
- Leclerc JE, Fearon B. Choanal atresia and associated anomalies. Int J Pediatr Otorhinolaryngol 1987;13:265-72. [Crossref] [PubMed]
- Blitz AM, Aygun N, Herzka DA, et al. High Resolution Three-Dimensional MR Imaging of the Skull Base: Compartments, Boundaries, and Critical Structures. Radiol Clin North Am 2017;55:17-30. [Crossref] [PubMed]
- Messineo D, Chernikava M, Pasquali V, et al. Radiological Parameters Review for Choanal Atresia. Pediatr Rep 2021;13:302-11. [Crossref] [PubMed]
Cite this article as: Tan HB, Rathnayake C, Selvam S, Berkowitz RG. Magnetic resonance imaging evaluation of choanal atresia in newborns. Aust J Otolaryngol 2022;5:19.