
Extension of a multinodular goitre into the parapharyngeal space—a case report of a rare pathology
Introduction
The parapharyngeal space (PPS) is a complex anatomical region in the neck. As an inverted pyramid, the skull base forms the floor and the greater cornu of the hyoid bone forms the apex (1,2). Masses of the PPS are rare, accounting for only 0.5% of all head and neck neoplasms (3,4). Most are benign and salivary in origin (1,2). Thyroid tissue extending into the PPS is even less frequent, making this subtype exceptionally rare. Herein we describe the clinical presentation, management, and histological features of a multinodular goitre (MNG) within the PPS. We present the following article in accordance with the CARE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-18/rc).
Case presentation
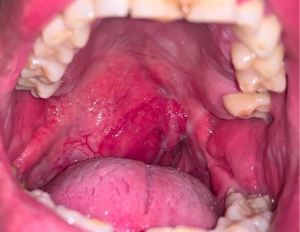
A 35-year-old male presented with a three-year history of a painless, slowly enlarging, right-sided oropharyngeal mass, and a “hot potato” voice. No dysphagia, odynophagia or B-type symptoms were present. His past-medical history included worsening obstructive sleep apnoea (OSA), for which he had a tonsillectomy in 2014. There was no personal or family history of thyroid disease or malignancy. He was a current smoker (12 pack-years). On examination, a large mass was visible in the oropharynx, extending from the right tonsillar fossa towards the midline, with an audible stertor. Palpation revealed a non-tender, smooth, firm mass with palpable level IIA/B lymph nodes on the ipsilateral side. Flexible endoscopy revealed intact vocal fold movement and no further abnormalities.
The patient was clinically and biochemically euthyroid (Thyroid-Stimulating Hormone 0.44 mIU/L). All other blood investigations were unremarkable. Computed tomography (CT) and magnetic resonance imaging (MRI) identified a 6 cm × 4 cm × 7.5 cm heterogeneous mass in the right PPS, causing lateral deviation of the pterygoid muscles and posterior deviation of the prevertebral muscles (Figure 1). The left PPS was unremarkable. The mass was anterior to the right styloid and carotid sheath and abutted the right internal carotid artery at the level of the maxilla. It also extended inferiorly from C1 to C3/4. Radiology review did not suggest this mass could be thyroid in origin.

Ultrasound-guided fine-needle aspiration cytology was non-diagnostic. A transoral incisional biopsy was performed in theatre which confirmed thyroid tissue and a working diagnosis of ectopic thyroid tissue was made (Figure 2). A right hemithyroidectomy, parapharyngeal mass, submandibular gland, and Level IIA super selective neck dissection was performed using a transcervical approach. An awake fibreoptic nasotracheal intubation was undertaken to secure the airway. Adequate exposure revealed superior extension of the right hemi-thyroid and continuity with the parapharyngeal mass (Figure 3).

Macroscopically, the hemi-thyroid measured 11 cm × 3.5 cm × 2.2 cm, had a nodular outer surface and weighed 32 g. Incision revealed visible colloid and grey-brown nodules. In contrast, the parapharyngeal mass measured 6.0 cm × 4.0 cm × 3.0 cm and weighed 34 g. The cut surface demonstrated grey oedematous and haemorrhagic nodules, with areas of fibrosis. Histopathological assessment of both specimens identified benign thyroid tissue with nodular hyperplasia and no evidence of malignancy. Histopathological analysis of the excised submandibular gland and lymph nodes were unremarkable. A final diagnosis of MNG in the PPS was made. The post-operative recovery period was uneventful. The patient was discharged shortly thereafter and remained biochemically euthyroid on follow-up. The patient no longer has OSA. All procedures performed in this study were in accordance with the ethical standards of the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication in accordance with Health and Disability Ethics Committee (HDEC) regulations. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
To our knowledge, this is the first reported case in the literature of a MNG with extension into the PPS. This case demonstrates the diagnostic difficulty of assessing a mass in the PPS and our management in a euthymic patient.
The tensor-vascular-styloid fascia forms a thick fascial plane that divides the PPS into the prestyloid and poststyloid space (1,3-5). Prestyloid lesions are almost always salivary in origin, while poststyloid lesions are most commonly neurogenic. Primary tumours (benign or malignant) are the most common pathology found in the PPS, followed by metastatic disease, tumours extending from adjacent sites and lymphoproliferative disease (1,2,4).
PPS lesions have highly variable presentations depending on their location within the PPS. The surrounding muscles, mandible and salivary glands make it increasingly difficult to identify and characterise tumours through physical examination (1,5-7). As a result, PPS lesions commonly present orally as smooth submucosal masses causing displacement of the tonsils, soft palate and/or lateral pharyngeal wall, as seen in our patient (6,8). Symptom onset is typically associated with progressive enlargement of the mass or associated complications such as dyspnoea, dysphagia, OSA, hoarseness, or cranial-nerve defects (5,7-9). The anatomical complexity of the PSS often makes confirmation of pre-operative diagnosis difficult, thus, radiological imaging is essential (6).
It is well known that enlarged thyroid glands may extend outside of the usual boundaries of the thyroid bed (6). Caudal extension is most common, expanding inferiorly into either the anterior or posterior mediastinum. In contrast, cranial extension, or lateral extension into either side of the pharynx is less common (5). To our knowledge, this is only the 6th recorded case in the literature identifying parapharyngeal extension of an enlarged thyroid, and the first of a MNG (4,6,8,9).
Although rare, extension of an enlarged thyroid gland into the PPS is possible due to the fascial anatomy of the neck (5,6). The PPS is continuous with the retrovisceral space, which starts at the skull base and ends at the level of T2–T6. The retrovisceral space is divided into the retropharyngeal space and retroesophageal space at the level of the pharynx and cervical oesophagus, respectively. The retrovisceral space has a ventral projection at the level of the thyroid cartilage, called the visceral compartment. The visceral compartment spans either side of the cervical oesophagus and is divided inferiorly by a fold of fascia into anterior (pretracheal) and posterior (retroesophageal) spaces (6). This fascial fold creates a complex yet continuous shared space containing the thyroid gland, parathyroid glands, trachea, and larynx, and explains the anatomical basis for retropharyngeal and parapharyngeal extension of an enlarged thyroid into the PPS (5,6). Therefore, despite their rarity, surgeons and radiologists should be aware of this important differential when assessing a PPS mass.
Conclusions
Herein we describe the rare occurrence of an MNG extending into the PPS. This case study explains the anatomical basis of a goitrous extension into the PPS and emphasises the importance of including MNG in the differential diagnosis of a parapharyngeal mass.
Acknowledgments
We would like to thank Counties Manukau District Health Board for their assistance in collecting the data required to write this manuscript.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-18/rc
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-18/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Malipatil SR, George CK, Vidisha I, et al. Aberrant Thyroid in the Parapharyngeal Space. Bengal Journal of Otolaryngology and Head Neck Surgery 2018;26:60-3. [Crossref]
- Soscia A, Guerra G, Cinelli MP, et al. Parapharyngeal ectopic thyroid: the possible persistence of the lateral thyroid anlage. Clinical case report. Surg Radiol Anat 2004;26:338-43. [Crossref] [PubMed]
- Foma W, Pegbessou E, Amana B, et al. Left parapharyngeal ectopic goitre associated with eutopic thyroid and postoperative Horner's syndrome. Eur Ann Otorhinolaryngol Head Neck Dis 2017;134:207-8. [Crossref] [PubMed]
- Cetik F, Yazici D, Uguz A. A thyroid tumor extending to the parapharyngeal space. BMC Ear Nose Throat Disord 2006;6:3. [Crossref] [PubMed]
- Chin SC, Rice H, Som PM. Spread of goiters outside the thyroid bed: a review of 190 cases and an analysis of the incidence of the various extensions. Arch Otolaryngol Head Neck Surg 2003;129:1198-202. [Crossref] [PubMed]
- Lakhani R, Nijjar R, Fishman JM, et al. A retropharyngeal multinodular goitre. Ann R Coll Surg Engl 2010;92:W35-7. [Crossref] [PubMed]
- Bozza F, Vigili MG, Ruscito P, et al. Surgical management of parapharyngeal space tumours: results of 10-year follow-up. Acta Otorhinolaryngol Ital 2009;29:10-5. [PubMed]
- Baik FM, Zhu V, Patel A, et al. Airway management for symptomatic benign thyroid goiters with retropharyngeal involvement: Need for a surgical airway with report of 2 cases. Otolaryngol Case Rep 2018;7:10-2. [Crossref]
- Testini M, Logoluso F, Lissidini G, et al. Emergency total thyroidectomy due to non traumatic disease. Experience of a surgical unit and literature review. World J Emerg Surg 2012;7:9. [Crossref] [PubMed]
Cite this article as: Clark ST, Yeom BW, Cho A, Johnston JJ. Extension of a multinodular goitre into the parapharyngeal space—a case report of a rare pathology. Aust J Otolaryngol 2022;5:23.


