
Cochlear implantation surgery with conscious sedation in the very elderly: a feasibility study comparing cochlear implant outcomes in general anaesthesia (GA) and local anaesthesia (LA) cohorts
Introduction
Age-related hearing loss is an independent risk factor for neurodegenerative diseases such as dementia and Alzheimer’s disease (1,2). Hearing impairment is the third highest cause of years lived with disability and the number of people over the age of 65 is estimated to double from 800 million to 1.6 billion by the year 2050 (3-5). Improving hearing significantly improves the global condition of the elderly patient in addition to significantly impacting communication and social interactions (1). While hearing amplification strategies such as hearing aids provide an effective strategy for patients with mild to moderate hearing loss, it does not sufficiently address hearing in patients with severe-to-profound hearing loss (6).
Cochlear implantation provides an alternative strategy for patients with severe hearing loss as well as addressing associated symptoms such as tinnitus (7). In addition to the audiological benefits, cochlear implantation in the elderly patient has been shown to improve social interactions, language as well as improvements in their quality of life (8-10).
Significant limitations in cochlear implantation in the elderly are risks involved in performing general anaesthesia (GA) due to patient’s multiple comorbidities, as well as post-operative delirium and post-operative cognitive dysfunction (11,12). In addition to the decreased independence and general frailty, anxiety and hesitation exists among patients to accept to undergo elective surgery. Given their multiple comorbidities, other elderly patients may also not be suitable candidates for GA.
Cochlear implantation under local anaesthesia (LA) with sedation is an alternative method that avoids the risks associated with a GA and expands availability of this technology to elderly patients who are otherwise medically unfit. Previous studies have demonstrated CI under LA is comparable to GA with measurable reduction in surgical times, cost of anaesthesia and overall shorter inpatient stays (13,14). However, few studies have analysed the feasibility of CI under LA in the elderly population (15-18).
This study compares CI under LA in the very elderly patient (80+ years) with age-matched patients who received CI under GA.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Westmead Hospital (QA 1903-01). Individual consent for this retrospective analysis was waived.
Between an empirically chosen period of 24 months (2018 and 2020) patients over the age of 80 receiving a CI under LA were recruited. These patients either opted to avoid the risks of GA, were high risk for GA due to their multiple co-morbidities or were medically unfit to have a GA. Patients were thoroughly counselled pre-operatively about intra-operative and post-operative expectations by both surgeon and anaesthetist. These patients were then compared to age-matched patients who received cochlear implantation under GA. All patients received their cochlear implant (CI) and anaesthetic by the same surgeon and anaesthetist in the same hospital to reduce variations in surgical technique, equipment and administration of sedation/anaesthetic. Prior to each case, the surgical team, anaesthetic team and nursing scrub were briefed about the protocol and any possible issues that might arise were discussed. Data was recorded in the patient record at the time of surgery and accessed for this study by retrospective chart review.
Local anaesthetic/sedation and GA protocols
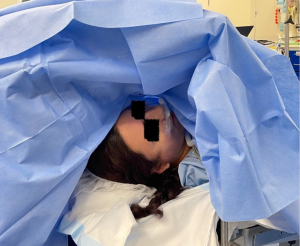
Intravenous access was established prior to entering the operating room. The post auricular incision was marked and infiltrated with Xylocaine 1% with 1:100,000 adrenaline was administered. A four-point auricular ring block was used to anaesthetise the pinna and middle ear structures. Patients were prepped and draped to achieve a sterile field and a combination of dexmedetomidine/midazolam were used as sedation throughout the case. The dosage of sedation agents was varied to maintain the patient in a comfortable and lucid state throughout the procedure (Figure 1). During the case if patients complained of pain or discomfort this was addressed either with additional local anaesthetic or sedation as per dosage of above. The duration of anaesthesia for both groups was included in the analysis. For the LA group the time of anaesthetic commenced with the infusion of dexmedetomidine/midazolam and concluded with the timing of surgery. For the GA group with the timing commenced with the infusion of induction agents, generally propofol and/or remifentanil and concluded with extubation.
Surgical technique
Patients were positioned supine on a head ring with the head turned as allowable. For patients with limited neck mobility or kyphosis, the operating bed was adjusted accordingly to optimise positioning. The anaesthetist at the head of the table was in constant communication with the patient and where applicable the contralateral hearing aid or CI was left in place for communication. All patients were given antibiotics on induction as well as sequential compression devices for thrombosis prophylaxis. Following establishment of a sterile field a standard post auricular incision was made and an anterior Palva flap was raised. The subperiosteal pocket was elevated postero-superiorly and a bony tunnel as well as a bony pocket was drilled.
A cortical mastoidectomy was then performed in a standard fashion with topical anaesthetic applied prior to entering the middle ear space through a facial recess opening. During identification of the lateral semicircular canal and incus, warm fluid was used and suctioned as necessary to reduce the caloric effect causing vertigo. An extended round window opening to the cochlea was used in all cases. Facial nerve monitor was used during the facial recess approach. Additional topical xylocaine was infused into the middle ear to supplement analgesia.
The CI processor is fitted in the bony pocket and the electrode array was slowly inserted through the extended round window opening over a duration of 1 min. Electrode impedances, electrically evoked auditory brainstem response (eABR) and neural response telemetry (NRT) were performed using reduce current levels (CLs) to determine appropriate stimulation of the auditory nerve. Typically, CLs were reduced to CL <80 (usually CL =220) during NRT. It was common for patients to perceive formed sound during this testing further confirming correct electrode placement. The wound was then closed in layers, the procedure terminated, and the patient transferred to the recovery room for further observation. A cone beam computed tomography (CBCT) was performed the next morning to document correct electrode placement in all cases.
Outcome measures
Primary outcomes measured included duration of anaesthesia, operative time, post-operative analgesia requirement, post-operative disequilibrium, time spent in recovery, duration of admission and any adverse events experienced by patients in both groups with a focus on post-operative confusion. Post operative confusion was defined as disorientation in one or more responses to questions assessing time, place or person persisting more than 1 hour. As this was a retrospective observational review, pre-operative cognitive decline was assessed informally by history of memory, executive functions, learning and language. No formal tests of cognition were used.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 26.0 for Windows (IBM Corp., Armonk, NY, USA). Data was summarized using descriptive statistics following evaluation of data distribution for normality. All non-parametric measures are presented as medians and interquartile range (IQR) with differences between groups analyzed using the Mann Whitney U test. Univariate regression modelling and analysis was performed for the risk of post-operative confusion and cognitive impairment. Where relevant odds ratio (OR) and the relevant 95% confidence intervals (95% CIs) are presented. All tests were two tailed a P value of <0.05 was considered statistically significant.
Results
Patient demographics
A total of 16 patients received CI under LA and were compared against 28 age-matched patients who received CI under GA. The median age of patients was 82.2 and 83.5 years in the LA and GA group respectively. There was no significant difference in age by type of anaesthetic (P=0.788). Patients in the LA group had higher rates of pre-operative cognitive impairment compared with the GA group (P=0.013).
There was no difference in comorbidities and functional status between the two groups.
All patients in the GA group were deemed American Society of Anaesthesiologists (ASA) 3 or 4 according to the ASA Physical Status Classification System. In the LA group, 13 patients were deemed ASA 3 or a 4 while 3 patients were deemed ASA 1 or a 2.
Nine patients in the GA group had a contralateral CI inserted and 4 patients in the LA group had a contralateral CI previously performed under GA. During the operation, all patients received a perimodiolar implant except one patient in the LA group who received a lateral wall implant. Table 1 outlines the comparison endpoints between the two groups.
Table 1
| General characteristics | LA group (n=16) | GA group (n=28) | P value |
|---|---|---|---|
| Age (years), median [IQR] | 82.2 [78.5–88.8] | 83.5 [80.0–88.0] | 0.78 |
| Aetiology of hearing loss, n (%) | – | ||
| Otosclerosis | 2 (12.5) | 4 (14.3) | |
| Presbycusis | 3 (18.8) | 5 (17.9) | |
| NIHL | 2 (12.5) | 4 (14.3) | |
| Unknown | 4 (25.0) | 5 (17.9) | |
| Other | 5 (13.3) | 10 (35.7) | |
| ASA score, n (%) | 0.42 | ||
| 1 & 2 | 3 (18.8) | 0 | |
| 3 & 4 | 13 (81.3) | 28 (100.0) | |
| Comorbidities, n (%) | |||
| Hypertension | 8 (50.0) | 14 (50.0) | >0.99 |
| Diabetes | 3 (18.8) | 2 (7.1) | 0.34 |
| Vascular disease | 3 (18.8) | 11 (39.3) | 0.15 |
| Reduced mobility, n (%) | 4 (25.0) | 3 (10.7) | 0.236 |
| Duration of deafness (years), median [IQR] | 44.0 [18.8–55.0] | 30.0 [20.0–45.0] | 0.33 |
| Previous otologic surgery, n (%) | 4 (25.0) | 9 (32.1) | 0.73 |
LA, local anaesthesia; GA, general anaesthesia; IQR, interquartile range; NIHL, noise induced hearing loss; ASA, American Society of Anaesthesiologists.
Anaesthetic and operative time
There was no difference in anaesthetic time between the two groups (median anaesthetic time in the LA group 142.5 vs. 133.5 min for the GA group; P=0.53). The longer LA times most likely reflecting the initial 10–20 min loading dosage period required for dexmedetomidine. Although there was a trend towards shorter duration of surgery in the LA group compared to the GA group, the differences were not significant (median 94.0 for LA vs. 109.0 min for GA; P=0.08) (see Table 2).
Table 2
| Operative parameters | LA group (n=16) | GA group (n=28) | P value |
|---|---|---|---|
| ASA score, n (%) | 0.42 | ||
| 1 & 2 | 3 (18.8) | 0 (0) | |
| 3 & 4 | 13 (81.3) | 28 (100.0) | |
| Anaesthetic time (min), median [IQR] | 142.5 [106.0–186.3] | 133.5 [116.3–148.8] | 0.53 |
| Operative time (min), median [IQR] | 94.0 [77.8–148.3] | 109.0 [96.3–119.8] | 0.08 |
| Electrode type, n (%) | 0.36 | ||
| Perimodiolar | 15 (93.8) | 28 (100.0) | |
| Lateral wall | 1 (6.3) | 0 |
LA, local anaesthesia; GA, general anaesthesia; ASA, American Society of Anaesthesiologists; IQR, interquartile range.
Perioperative recovery and inpatient admission time
There was no significant difference in time spent in recovery room between the two groups (median 78.5 min for LA vs. 88.5 min for GA; P=0.51). All patients were discharged within 24 hours except one patient in the GA group. This patient had a 7 days admission due to prolonged confusion.
Patient experience
There was no significant difference in requirement for post-operative analgesia between LA and GA groups (P=1.000). Patients were asked to provide feedback regarding comfort levels as well as any persistent issues. Adverse pain was defined as requiring more than paracetamol for pain control. There were no significant differences between the LA and GA group (P=0.29). Two patients in the LA group and 8 patients in the GA group experienced post-operative disequilibrium, which resolved within 24 hours.
During the postoperative rehabilitation and training three patients in the GA group experienced post-operative confusion. One patient in the GA group had post op confusion lasting 7 days which eventually resolved but required a prolonged hospital admission. This patient was the eldest in the cohort at 92 years of age with sensory deprivation including enucleation of one eye. No patients in the LA group experienced confusion in the post-operative period.
Using univariant modelling the limited data set demonstrated that for every 1-min increase in duration of anaesthetic, the risk of post-operative confusion increased by 1.042-fold (OR =1.042; 95% CI: 1.1 to 131.2; P=0.042). As the number of comorbidities increases the risk of cognitive impairment increased by almost two and half times (OR =2.4; 95% CI: 0.9 to 6.1; P=0.065). Although not significant, univariate modelling showed that for every unit increase in ASA score the risk of cognitive impairment increases by three-fold (OR =3.041; 95% CI: 0.328 to 28.185; P=0.328). There is a high degree of variability in our study cohort as such, the results need to be interpreted with some caution. Table 3 outlines post-operative observations discussed above.
Table 3
| Post-operative observations | LA group (n=16) | GA group (n=28) | P value |
|---|---|---|---|
| Recovery time (min), median [IQR] | 78.5 [53.8–96.5] | 88.5 [55.5–114.5] | 0.51 |
| Inpatient admission (hours), median [IQR] | 24 [24–24] | 24 [24–24] | 0.76 |
| Adverse experience reported (N&V, rash), n (%) | 3 (18.8) | 9 (32.1) | 0.29 |
| Post op analgesia required, n (%) | 12 (75.0) | 22 (78.6) | >0.99 |
| Post op disequilibrium, n (%) | 2 (12.5) | 8 (28.6) | 0.276 |
| Persistent confusion >24 hours, n (%) | 0 | 3 (10.7) (one case lasting 7 days) | 0.013 |
LA, local anaesthesia; GA, general anaesthesia; IQR, interquartile range; N&V, nausea & vomiting.
Discussion
The results of this study demonstrate cochlear implantations under LA with sedation is a viable option in very elderly patients (80+ years) who would otherwise be limited by having GA. Compared to age-matched patients with similar comorbidity profile and pre-operative cognitive function who received a GA, there were no differences in anaesthetic time, operative time and recovery ward time. This was similar to previously published studies comparing CI under LA versus GA (18,19). Connors and colleagues (16) compared 100 patients receiving CI under LA with conscious sedation with 50 age-matched patients who had CI under GA and found shorter surgery time and overall operative room time in the LA cohort. Recovery room times were similar between both cohorts. Similar studies also found a shorter duration in surgical time as well anaesthetic time (18). In this study, there was a trend towards shorter duration of surgery in the LA group compared to the GA group although the differences were not significant. This is likely reflective of the limited number of patients recruited in this study rather than surgical differences between the two groups. Hamershmidt and colleagues (13) demonstrated shorter time in recovery, inpatient stay and lower cost of anaesthesia in patients receiving cochlear implantation under LA. However, the major of their patients were under 40 years of age, and likely to be fitter than our elderly cohort (13).
Patients in both groups required similar post-operative analgesia and inpatient admission. Patient’s reported similar experiences in terms of comfort level scores between the two groups. In addition to a lengthy discussion with the patient regarding consent and expectations of having LA, a co-ordinated team effort and understanding is critical to optimise patient experience.
In this study 3 patients in the GA group experienced post-operative confusion compared to no patients in the LA group. On univariate modelling, post-operative confusion increased with every 1-min of duration of anaesthesia, number of comorbidities and ASA score. This is consistent with previous literature published on the effects of GA and surgery and post-operative cognitive decline (POCD). POCD was reported as early as 1950s by Bedford and colleagues, who noticed permanent post-operative mental decline in over 1,000 patients over the age of 50 years (20). In a large International Study of Postoperative Cognitive Dysfunction (ISPOCD) study, Moller and colleagues (21) also identified through neuropsychological testing, a 25% risk of post-operative cognitive dysfunction 1 week after surgery in patients 60 years of age and above compared to 3.4% in younger controls. Furthermore, there was an almost 10% risk of post-operative cognitive dysfunction in elderly patients compared to 2.8% younger controls (21). The results of both were statistically significant. On longer follow-up (over 6 years) the same ISPOCD group reported a significantly increased mortality in that subset of patients who had POCD 3 months post operatively (22).
Patients over the age of 60 years are more prone to the neurotoxic effects of anaesthesia especially with isoflurane and sevoflurane (23-25). For elderly patients receiving GA, where possible it is recommended to minimise anaesthetic depth and periods of electroencephalographic suppression, limit duration of continuous anaesthesia and consider regional anaesthesia or light sedation (24).
In this study patients receiving LA, conscious sedation was achieved with dexmedetomidine and occasionally supplemented with midazolam for patients with anxiety. In contrast to the inhaled anaesthetic agents, dexmedetomidine is believed to be neuroprotective with significantly reduced incidence of post-operative cognitive dysfunction based on a meta-analysis of 26 randomized controlled trials (26).
The relationship between GA and development of Alzheimer’s disease or dementia is controversial (23). While there seems to be an increased risk of developing dementia in patients who received a GA and surgery after the age of 60 years based on meta-analysis of cohort and case-control studies, these findings are not corroborated by meta-analysis of population-based studies, where no strong link was demonstrated between GA and surgery and risk of dementia in the elderly (25,27).
This study is limited by the small number of patients undergoing CI under LA. Although previous studies have compared CI under LA with GA in the elderly population, the very elderly (80+ years) is a unique cohort and demonstrates the feasibility of LA in this age group. Further prospective and larger studies are required to further expand on the efficacy of using LA in the elderly population as well as comparing the cognitive outcomes in this age group.
Conclusions
Cochlear implantation under LA with conscious sedation is a safe and feasible option for very elderly patients who are otherwise not suitable or unfit for GA. Given the potential postoperative cognitive effects of GA, LA with conscious sedation should be offered as an alternative anaesthesia to patients undergoing CI surgery.
Acknowledgments
None.
Footnote
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-22/dss
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-22/coif). MdC reports that he is a paid member of Commonwealth Department of Health Committee and paid consultant to Cochlear Ltd. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of this work and ensure that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Westmead Hospital (QA 1903-01). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ralli M, Gilardi A, Stadio AD, et al. Hearing loss and Alzheimer's disease: A Review. Int Tinnitus J 2019;23:79-85. [Crossref] [PubMed]
- Liu CM, Lee CT. Association of Hearing Loss With Dementia. JAMA Netw Open 2019;2:e198112. [Crossref] [PubMed]
- Yang Z, Cosetti M. Safety and outcomes of cochlear implantation in the elderly: A review of recent literature. J Otol 2016;11:1-6. [Crossref] [PubMed]
- Hearing loss prevalence and years lived with disability, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet 2021;397:996-1009. [Crossref] [PubMed]
- He W, Goodkind D, Kowal P. An Aging World: 2015 International Population Reports. Washington, USA: U.S. Census Bureau, 2015.
- Lerner S. Limitations of Conventional Hearing Aids: Examining Common Complaints and Issues that Can and Cannot Be Remedied. Otolaryngol Clin North Am 2019;52:211-20. [Crossref] [PubMed]
- Peter N, Liyanage N, Pfiffner F, et al. The Influence of Cochlear Implantation on Tinnitus in Patients with Single-Sided Deafness: A Systematic Review. Otolaryngol Head Neck Surg 2019;161:576-88. [Crossref] [PubMed]
- Amin N, Wong G, Nunn T, et al. The Outcomes of Cochlear Implantation in Elderly Patients: A Single United Kingdom Center Experience. Ear Nose Throat J 2021;100:842S-7S. [Crossref] [PubMed]
- Lin FR, Chien WW, Li L, et al. Cochlear implantation in older adults. Medicine (Baltimore) 2012;91:229-41. [Crossref] [PubMed]
- Vermeire K, Brokx JP, Wuyts FL, et al. Quality-of-life benefit from cochlear implantation in the elderly. Otol Neurotol 2005;26:188-95. [Crossref] [PubMed]
- Hussain M, Berger M, Eckenhoff RG, et al. General anesthetic and the risk of dementia in elderly patients: current insights. Clin Interv Aging 2014;9:1619-28. [PubMed]
- Mason SE, Noel-Storr A, Ritchie CW. The impact of general and regional anesthesia on the incidence of post-operative cognitive dysfunction and post-operative delirium: a systematic review with meta-analysis. J Alzheimers Dis 2010;22:67-79. [Crossref] [PubMed]
- Hamerschmidt R, Mocellin M, Gasperin A, et al. Local anesthesia for cochlear implant surgery: low risks for the patient and few costs for the hospital, a rational alternative. Rev Laryngol Otol Rhinol (Bord) 2011;132:227-9. [PubMed]
- Hamerschmidt R, Moreira AT, Wiemes GR, et al. Cochlear implant surgery with local anesthesia and sedation: comparison with general anesthesia. Otol Neurotol 2013;34:75-8. [Crossref] [PubMed]
- Kecskeméti N, Szőnyi M, Küstel M, et al. Cochlear implantation under local anesthesia: a possible alternative for elderly patients. Eur Arch Otorhinolaryngol 2019;276:1643-7. [Crossref] [PubMed]
- Connors JR, Deep NL, Huncke TK, et al. Cochlear Implantation Under Local Anesthesia With Conscious Sedation in the Elderly: First 100 Cases. Laryngoscope 2021;131:E946-51. [Crossref] [PubMed]
- Mistry SG, Carr S, Martin J, et al. Cochlear implantation under local anaesthesia - Our experience and a validated patient satisfaction questionnaire. Cochlear Implants Int 2017;18:180-5. [Crossref] [PubMed]
- Shabashev S, Fouad Y, Huncke TK, et al. Cochlear implantation under conscious sedation with local anesthesia; Safety, Efficacy, Costs, and Satisfaction. Cochlear Implants Int 2017;18:297-303. [Crossref] [PubMed]
- Pateron B, Bakhos D, LeLouarn A, et al. Local anaesthesia and conscious sedation for cochlear implantation: experience with 20 patients. J Laryngol Otol 2016;130:151-6. [Crossref] [PubMed]
- Bedford PD. Adverse cerebral effects of anaesthesia on old people. Lancet 1955;269:259-63. [Crossref] [PubMed]
- Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet 1998;351:857-61. Erratum in: Lancet 1998;351:1742. [Crossref] [PubMed]
- Steinmetz J, Christensen KB, Lund T, et al. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology 2009;110:548-55. [Crossref] [PubMed]
- Belrose JC, Noppens RR. Anesthesiology and cognitive impairment: a narrative review of current clinical literature. BMC Anesthesiol 2019;19:241. [Crossref] [PubMed]
- Cottrell JE, Hartung J. Anesthesia and Cognitive Outcome in Elderly Patients: A Narrative Viewpoint. J Neurosurg Anesthesiol 2020;32:9-17. [Crossref] [PubMed]
- Jiang J, Dong Y, Huang W, et al. General anesthesia exposure and risk of dementia: a meta-analysis of epidemiological studies. Oncotarget 2017;8:59628-37. [Crossref] [PubMed]
- Yang W, Kong LS, Zhu XX, et al. Effect of dexmedetomidine on postoperative cognitive dysfunction and inflammation in patients after general anaesthesia: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e15383. [Crossref] [PubMed]
- Lee JJ, Choi GJ, Kang H, et al. Relationship between Surgery under General Anesthesia and the Development of Dementia: A Systematic Review and Meta-Analysis. Biomed Res Int 2020;2020:3234013. [Crossref] [PubMed]
Cite this article as: Shah S, Ahmadzada S, Hitos K, da Cruz M. Cochlear implantation surgery with conscious sedation in the very elderly: a feasibility study comparing cochlear implant outcomes in general anaesthesia (GA) and local anaesthesia (LA) cohorts. Aust J Otolaryngol 2022;5:33.


