The prevalence of middle ear effusion at the time of grommet insertion—a retrospective cohort study
Introduction
Grommets or ventilation tube insertion are common surgical procedures completed in paediatric otolaryngology. Most cases are completed in children due to recurrent acute otitis media (AOM) or otitis media with effusion (OME). Children aged one to three are at particular risk of developing OME with a prevalence of 10–30% and generally reducing after the age of seven. By the age of four, up to 80% of children have had OME (1). Patients with Trisomy 21 or cleft palate are at particular risk and generally receive multidisciplinary team input (2).
While painless, OME is the most common cause of acquired hearing loss in children with direct impacts on hearing and speech development. The impact of effusion on hearing is variable but can reach up to 50 dB conductive loss (1). In New Zealand, children with OME are either referred by general practitioners (GP) or through the B4 School Checks. The B4 School Checks are part of the Well Child Tamariki Ora programme established in 2008. The check aims to identify any health, developmental or behavioural problems in four-year-old children nationwide (3,4). Part of the check includes an audiometry and tympanometry with children demonstrating persisting OME or type B tympanograms being referred.
OME in itself typically does not cause any harm. Despite the high incidence, many children experience OME transiently and do not have any noticeable symptoms. Most cases of OME persist for 6 to 10 weeks with 56% of cases spontaneous resolve within 3 months (5). The optimal time for treatment has been debated and internationally guidelines vary (5-7).
There is general consensus that patients who have bilateral OME, persisting greater than 3 months and have associated hearing loss are suitable candidates for surgery (2). The challenge with the current health system is the significant interval between being wait-listed and the surgery. The Ministry of Health (MoH) targets a 4 months wait-list duration in New Zealand. There is evidence that between three and six months, 56–72% of children with OME demonstrate spontaneous resolution. Taking into account the wait list criteria which require children to demonstrate OME present for greater than 3 months, the actual wait time may be up to nine months. At 9 months, 81% of patients show spontaneous resolution of OME (8).
Data released from the New Zealand Health Quality and Safety Commission suggest that nationally in the decade from 2009 to 2018, grommet insertion rates in children (age 0–14 years) have steadily reduced by 26.4%. In contrast, Waikato District Health Board have seen a gradual 33% increase of grommet insertion from 2010 to 2018 and has one of the highest insertion rates in the country. The national rate of grommet insertion at 2018 is 5.3 per 1,000 while Waikato is at 8.0 per 1,000 (9).
Patients who receive a myringotomy for OME and are not found to have fluid are designated as having “dry taps”. The reported rate in literature varies significantly from 0% to 34% (10-12). This is likely to be a reflection of different health models and guidelines between otolaryngology departments.
The aim of this study is to review the incidence of “dry taps” at Waikato Hospital. Our study also aims to both compare and contribute to existing literature to allow determination of optimal timing and best practice for the surgical management of OME (13,14).
Methods
Data collection for this retrospective study was completed at Waikato Hospital, Hamilton, New Zealand. All patients who receive any surgical procedure at Waikato Hospital will have associated procedure coding inserted into the theatre database.
The inclusion criteria are all patients who received a grommet or ventilation tube insertion, aged under 15 on the day of surgery and over a 12-month period from September 2019 to September 2020.
The internal hospital Concerto network was used for review of the patients’ clinic letters and operation notes. Patients who were wait-listed only for OME were included for further analysis. Excluded cases include AOM, cleft palate and Trisomy 21 patients. Patients who received a subannular T-tube for retraction of tympanic membrane and those without clinical documentation were also excluded.
Demographics including the patients age, gender and ethnicity were recorded. The date of the outpatient appointment on which the patient was placed onto the waiting list and date of surgery were both recorded. The operation note and discharge summary were reviewed for intra-operative findings.
Patients were considered to have a dry tap only when no fluid is found in both ears following myringotomy. Analysis was completed for variables including ethnicity, season, waiting list duration and age. Data analysis was completed through SPSS Software (Version 26.0; IBM). Descriptive frequency analysis was performed for patient demographics. Crosstabs and Chi-squared tests were used to compare categorical variables. Mean differences were compared through independent sample t-tests and one way analysis of variance (ANOVA) with post hoc Tukey’s. Statistical significance was taken at P<0.05.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was deemed outside the scope for ethical review and registered with the Clinical Audit Support Unit (#4157). Individual consent for this retrospective analysis was waived.
Results
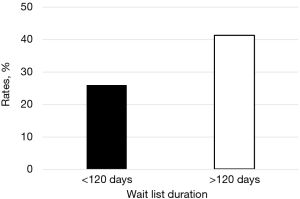
A total of 460 cases were identified in the initial search completed by the Department of Otolaryngology. Two hundred and ninety-two children fulfilled inclusion criteria and were included in the study (Figure 1); 56.8% were male and 43.2% female. New Zealand European (NZ European) were the most frequent ethnic group making up 53.4% with 33.6% Māori. The mean age of the cohort was 5 years (Table 1).
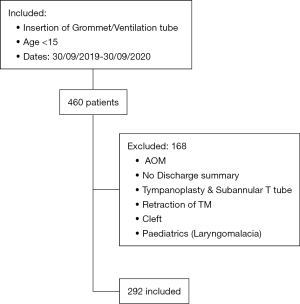
Table 1
| Demographics | Values |
|---|---|
| Gender, n (%) | |
| Male | 166 (56.8) |
| Female | 126 (43.2) |
| Ethnicity, n (%) | |
| NZ European | 156 (53.4) |
| Māori | 98 (33.6) |
| Other | 38 (13.0) |
| Age (range, 1–14 years), n | |
| 4 and under | 136 |
| 5 and over | 156 |
NZ European, New Zealand European.
One hundred and ten patients (37.7%) had bilateral dry taps following during surgery following myringotomies. Fifty-five patients (18.8%) were found to have unilateral effusion at the time of surgery. There were no statistical significance identified between ethnic groups for rate of dry taps; 32.7% and 39.7% dry tap rates were identified for Māori and NZ European respectively (P=0.25) (Table 2). No significant difference in dry tap rate was found between summer and winter months.
Table 2
| Ethnicity | NZ European | Māori | Overall | P value |
|---|---|---|---|---|
| Wait list duration (mean) | 149.7 days | 158.7 days | 153.7 days (range, 7–327 days) | 0.22 |
| Dry tap | 39.7% | 32.7% | 37.7% | 0.25 |
NZ European, New Zealand European.
The average duration patients spent on the waiting list was 153.1 days. No significant difference was found between Māori and NZ European. Patients who had intra-operative dry taps spent a significantly longer period on the waiting list than those found to have persisting OME (163.4 vs. 146.8 days, P=0.02) (Figure 2). Patients who received their surgery within 4 months had a dry tap rate of 26.0% compared to 41.6% for those on the waiting list greater than 4 months (P=0.02) (Figure 3).

Patients aged 5 and over demonstrated a higher occurrence of dry tap compared to children 4 and under, although this did not reach statistical significance (41.7% vs. 33.1%, P=0.13).
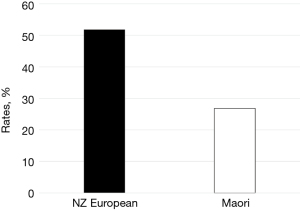
One hundred and seventeen (40.1%) of the 292 children were age 5 or over and were on the waiting list over 4 months. The dry tap rate for this cohort was 44.4%. NZ European were far more likely to receive a dry tap in this cohort 51.8% than Māori 26.8% (P=0.05) (Figure 4).
Discussion
The finding of intra-operative dry taps simply imply resolution of the child’s OME. Given most cases of OME are known to spontaneously resolve over time, dry taps are unavoidable in most centres. Our study found a dry tap rate of 37.7% with an average of 153.1 days on the wait list. The dry tap rates are at the top end of reported figures in literature and there were no significant ethnic disparities in the wait list duration. A higher proportion of dry taps raises a number of potential issues. Firstly, patients with resolved OME may no longer require surgery and would therefore be exposed to unnecessary surgical and anaesthetic risk. Second, the child would also take up valuable operating theatre resource.
The reported rate of dry taps in literature vary significantly from 0–34% (10-12). With the exception of Dempster’s study where the surgery took place 10 days following clinical confirmation of effusion, reporting no occurrence of dry taps, most studies reported findings of dry taps in mid-teen percentage rates (13).
Jardine had a large cohort of 1,688 children and found a bilateral dry tap rate of 16% (10). The true rate for OME may be lower as 15% of the children were listed for AOM. The study had a mean waiting list duration of 20 weeks. Significant correlation was found between dry tap rate and age, from around 10–15% at age three to five to around 30% at age 10 (10).
Delay in surgery has been identified as a key factor contributing to higher dry tap rates. Lee’s study which had a 16.9% dry tap rate supports this and suggested anaesthesia is unlikely to be a contributing factor. Henny found the optimal time to proceed with surgery is 1 to 2 months after wait-listing with a dry tap rate of around 10%. Further delays however correlate with sharp increases in dry tap rates, 20% at 4 months and 35% at 6 months. The study reported an 18% rate overall with only 7% being bilateral (11,14).
A possible reason for the high dry tap rates is the health system performing under significant strain with most departments operating at capacity volumes. While the MoH aims for a four-month wait for first specialist appointments (FSA), in reality, patients are not infrequently waiting much longer (15). Patients then on average wait another 4 to 6 months for their grommet procedure after being placed onto the waiting list. Consequently, consistent with Lee and Henny’s findings, delay in surgery means many patients no longer have OME at time of surgery (11,14). Our findings support this with those receiving surgery within the four months MoH target having a far lower proportion of dry taps. Furthermore, surgical intervention for OME is aimed at improving the child’s hearing to assist with speech and development. The delay in surgery also means a prolonged period of hearing and social challenges.
Significant health inequities exist for Māori in New Zealand. Māori have less health access, receive poorer health care and are more likely to suffer from racial discrimination (16). Low socioeconomic status and overcrowded homes are particular risk factors for ear pathology. Māori children are reported to have greater complications with OME compared to NZ European children. Despite Māori children having higher tympanometry failure rates than NZ European children, some studies have previously shown a lower proportion of Māori patients receiving elective surgery (3).
Thirty-three-point-six percent of our patients are Māori and exceeds the national average of 16.5% (17). The over representation of Māori in this case is a positive outcome. It likely reflects the greater Māori population in the Waikato and more importantly, Māori children with OME are accessing tertiary care to be wait-listed and receive appropriate surgical intervention. A similar finding was reflected in Auckland with 20% Māori children representation. Also found in the study was that Māori have equitable outcomes following surgery (18).
Older children and delay in surgery have consistently been associated with higher dry tap rates (10,14). Within this sub-group, we found Māori to have significantly lower rates of dry tap. Possible explanations for this include older Māori children being more susceptible to OME than older NZ European children or differences in the pathophysiology. This could also represent previous health inequities with fewer proportion of Māori children reported to receive surgery despite higher incidence of OME. Further research on this is required before any conclusion can be drawn.
Limitations
Our study numbers are likely to be lower than usual due to the impacts of coronavirus disease 2019 (COVID-19) pandemic. During the national lockdown of 6 weeks, no non-urgent elective operations were completed. The lockdown would have also increased the waiting list time for children who received surgery in the final 3 months of the study period.
Conclusions
High dry tap rates are strongly associated with delayed surgery, which unfortunately represents a health system operating at capacity. This feeds a negative cycle where neither the patient or hospital benefits. Conversely, identifying methods to reduce dry tap rates will minimise unnecessary use of theatre resource and achieve the goals of surgery, to treat OME and improve hearing deficits. Māori children are over-represented in our study, a likely reflection of the greater incidence of OME. Performing surgery within 2 months and scheduling a brief review for patients waiting more than 3 months would likely optimise the pathway.
Acknowledgments
None.
Footnote
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-25/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-25/prf
Funding: None.
Conflicts of Interest: Both authors have completed the ICMJE’s unified disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-25/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was deemed outside the scope for ethical review and registered with the Clinical Audit Support Unit (#4157). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Browning GG, Rovers MM, Williamson I, et al. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev 2010;CD001801. [Crossref] [PubMed]
- 2018 surveillance of otitis media with effusion in under 12s: surgery (NICE guideline CG60). 2018. Available online: www.nice.org.uk
- McCallum J, Craig L, Whittaker I, et al. Ethnic differences in acute hospitalisations for otitis media and elective hospitalisations for ventilation tubes in New Zealand children aged 0-14 years. N Z Med J 2015;128:10-20.
- Ministry of Health. B4 school check. Available online: Health.govt.nz
- Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngol Head Neck Surg 2016;154:S1-41. [Crossref] [PubMed]
- Venekamp RP, Mick P, Schilder AG, et al. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst Rev 2018;5:CD012017. [Crossref] [PubMed]
- Rosenfeld RM, Tunkel DE, Schwartz SR, et al. Clinical Practice Guideline: Tympanostomy Tubes in Children (Update). Otolaryngol Head Neck Surg 2022;166:S1-55. [Crossref] [PubMed]
- Rosenfeld RM, Kay D. Natural history of untreated otitis media. Laryngoscope 2003;113:1645-57. [Crossref] [PubMed]
- Ventilation tube (grommets) insertion (0-14 years), rate per 1000. Health and quality & safety commission New Zealand. 2020. Available online: www.hqsc.govt.nz
- Jardine AH, Maw AR, Coulton S. Dry tap at myringotomy: a three-year study of 1688 children undergoing myringotomy. Clin Otolaryngol Allied Sci 1999;24:266-9. [Crossref] [PubMed]
- Henney S, Counter P, Mirza S, et al. Pre-operative prediction of 'dry taps'. J Laryngol Otol 2009;123:61-8. [Crossref] [PubMed]
- Black NA, Sanderson CF, Freeland AP, et al. A randomised controlled trial of surgery for glue ear. BMJ 1990;300:1551-6. [Crossref] [PubMed]
- Dempster JH, Browning GG, Gatehouse SG. A randomized study of the surgical management of children with persistent otitis media with effusion associated with a hearing impairment. J Laryngol Otol 1993;107:284-9. [Crossref] [PubMed]
- Lee CH, Yoo CK, Hong JE, et al. Resolved effusion on myringotomy: a study of dry tap without general anesthesia. Int J Pediatr Otorhinolaryngol 2011;75:635-8. [Crossref] [PubMed]
- Ministry of Health. Elective services patient flow indicator web tool. 2022.
- Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health 2019;18:174. [Crossref] [PubMed]
- Statistics New Zealand. New Zealand’s population reflects growing diversity. 2019. Available online: https://www.stats.govt.nz/news/new-zealands-population-reflects-growing-diversity
- Johnston J, McLaren H, Mahadevan M, et al. Surgical treatment of otitis media with effusion in Maori children. ANZ J Surg 2018;88:1141-4. [Crossref] [PubMed]
Cite this article as: Wu J, Currie A. The prevalence of middle ear effusion at the time of grommet insertion—a retrospective cohort study. Aust J Otolaryngol 2023;6:6.