Virtual multidisciplinary meetings in a new COVID-19 world: how well are we doing it?
Highlight box
Key findings
• Most of our participants have felt it is more challenging to pay attention during online meetings;
• Adequate hearing was reported as an issue requiring further exploration.
What is known and what is new?
• Difficulties with technology uptake and use have been reported as a potential issue in the literature.
• Most of our participants found moving to a virtual platform helpful (70%).
• A high number of participants (91.6%) knew how to use the video function and felt they could engage whilst multi-tasking with screen sharing (62.5%).
What is the implication, and what should change now?
• Adequate hearing was reported as an issue requiring further exploration. The use better headphones and access to microphones may overcome this.
Introduction
In 2019, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a global pandemic (1). As of January 16, 2022, COVID-19 has caused over 323 million confirmed cases and over 5.5 million deaths worldwide (2). The pandemic necessitated a fast and contemporary transition within healthcare services around the globe. Consequently, online services to deliver patient care and facilitate clinician safety became the norm.
The Head and Neck cancer multidisciplinary team meeting (MDT) at the University Hospital Geelong is a meeting involving diverse health professionals that meet to deliver best practice management to cancer patients. This team includes otolaryngologists, plastic surgeons, maxillofacial surgeons, radiologists, oncologists, and allied health. Prior to the pandemic, meetings were exclusively held face-to-face and included the examination of patients. During the pandemic, they were swiftly transitioned online using the Zoom platform to adhere to social distancing rules and ensure clinician compliance and safety.
Before the pandemic, virtual MDTs (vMDT) were considered a ‘niche concept’ unlikely to replace conventional face-face meetings (3). Potential barriers to implementing a vMDT include issues with technology, difficulty reviewing slides and imaging, and loss of interpersonal relationships (3-5). In the heat of the pandemic, there was a rush to move our multidisciplinary meeting (MDM) online without the opportunity to consider such barriers.
The primary outcome of this article is to explore the current perception of the vMDT following the vital shift. In particular, the views on preparation, login, attendance, quality, patient outcomes, safety, and interpersonal relationships were considered. The aim is to understand the current perceptions to guide the changes required to improve the quality of our vMDT. The findings of this study will benefit other Head and Neck MDTs around Australia by the key issues highlighted. We present this article in accordance with the SURGE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-30/rc).
Methods
An online questionnaire, including Likert Scale and free text-type questions, was created using Redcap. The questions evaluated thoughts on preparation, login, attendance, quality, clinician safety and interpersonal relationships on the current vMDT compared to face-to-face meetings. An initial anonymous survey link was emailed to 59 Head and Neck Unit members by the principal investigator. A further reminder email was sent to participants 4 weeks following the initial email. There were no financial incentives provided to participants.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of the Barwon Health Research, Ethics, Governance, and Integrity Unit (No. HREC 73016) and informed consent was taken from all individual participants. The Barwon Health Research, Ethics, Governance, and Integrity Unit granted site-specific ethics for the project.
Statistical analysis
The responses were exported to Microsoft Excel for categorisation of data. Simple descriptive statistical analysis was performed.
Results
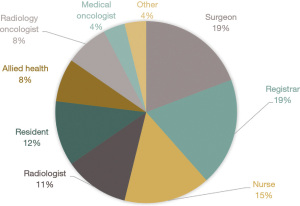
Members were permitted a 12-week period to answer the survey. We received 26 responses, corresponding to a response rate of 44.1%. Figure 1 summarises the different response rates by role within our unit. Note that incomplete responses were also considered. Responders included surgeons (19%), medical oncologists (4%), radiology oncologists (8%), junior medical staff (31%), allied health (8%), nursing staff (15%) and other (4%).
Attendance, log in and referral
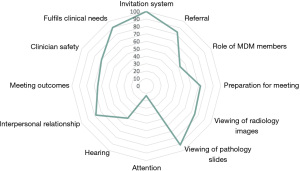
Since moving online, many participants (62.3%) find it easier to attend the meeting. Concerning login, 95.9% of participants know where to find the login details for the meeting, and 100% of survey participants find the weekly invitation link adequate (Figure 2). For patient referral, 62.5% feel it has not impacted their ability to refer patients.
Preparation, quality and meeting outcomes
Many participants felt that presentation preparation was not disrupted by moving to an online platform (72.7%). A proportion of 91.6% of participants know how to use the video function. Almost half of the participants (45.9%) find it difficult to hear during meetings. Most respondents were satisfied with the quality of radiology imaging (75.0%) and pathology sides (91.2%), and 70% of participants found the patient outcomes just as clear.
Clinician safety, relationships and future meetings
In addition, 65.2% of attendees feel less of an interpersonal relationship with colleagues since moving online. Regarding participant contribution, 47.8% feel it has not impacted their ability to contribute to the meeting, and 34.8% feel there has not been a change. In the future, most respondents (78.2%) would like the MDM to continue running in both a physical room and an online platform.
Discussion
This is the first Australian Head and Neck qualitative study exploring the use of a virtual MDT during the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. Our results demonstrate that overall, participants perceive virtual MDTs as similarly effective to face-to-face MDTs.
Before the pandemic, videoconferencing was established within larger healthcare centres to improve access for smaller centres within Australia. Delaney et al. compared virtual MDTs to face-to-face meetings to improve geographical attendance between clinicians. Interestingly, Delaney et al. demonstrated that virtual MDTs improve attendance; however, clinicians prefer face-to-face MDTs (6). Our results reflected this also, as most participants find it easier to attend online meetings. However, most respondents within our unit would like the MDT to continue running in both a physical room and an online platform in future.
To have a fully functioning online virtual MDT, Munro et al. recommended that a critical component is ensuring technical support services are available onsite (3). Difficulties with technology and connectivity were reported whilst using virtual MDTs during COVID (7). Whilst the viewing pathology slides and imaging were well received online, adequate hearing was reported as an issue within our unit requiring further exploration; examples such as using better headphones and access to microphones may overcome this. Unlike Bonanno et al., difficulties with technology uptake were not so much an issue within our unit. Most members knew how to use the video function and felt they could engage whilst multi-tasking with screen sharing. Perhaps the uncertainty of the pandemic fuelled a proactive approach to technology use.
Interestingly, most participants felt it is more challenging to pay attention during online meetings, possibly attributable to distractions in a home environment that would otherwise not be present in a structured environment. Other factors may be distractions from not hearing correctly or late dial-ins from mobile phones.
We acknowledge that this study is not without its limitation. The survey represents a small cohort’s viewpoint and is a single site-centred study. However, the respondents were from various specialties and seniority, which can be applied to the generalised Head and Neck MDT cohort. Another consideration is that these are clinicians’ opinions early in the use of vMDTs in the pandemic. As a result, their responses might be influenced by this. This study highlights the strengths and weaknesses of the vMDTs perceived within our unit. Knowing that difficulties exist with maintaining attention and hearing allows us to seek solutions to help improve the MDT’s effectiveness.
Conclusions
The ongoing resurgence of COVID-19 will mean that virtual meetings will stay. This study demonstrates that our participants find the vMDM a positive move. We hope other units benefit from being cognisant of the identified issues and allow for the development of their meetings during this pandemic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-30/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-30/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-30/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-30/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of the Barwon Health Research, Ethics, Governance, and Integrity Unit (No. HREC 73016) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organisation. Coronavirus disease 2019 (COVID-19): Situation Report, 75. WHO; 2020.
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed 2020;91:157-60. [PubMed]
- Munro AJ, Swartzman S. What is a virtual multidisciplinary team (vMDT)? Br J Cancer 2013;108:2433-41. [Crossref] [PubMed]
- Sidpra J, Chhabda S, Gaier C, et al. Virtual multidisciplinary team meetings in the age of COVID-19: an effective and pragmatic alternative. Quant Imaging Med Surg 2020;10:1204-7. [Crossref] [PubMed]
- Dharmarajan H, Anderson JL, Kim S, et al. Transition to a virtual multidisciplinary tumor board during the COVID-19 pandemic: University of Pittsburgh experience. Head Neck 2020;42:1310-6. [Crossref] [PubMed]
- Delaney G, Jacob S, Iedema R, et al. Comparison of face-to-face and videoconferenced multidisciplinary clinical meetings. Australas Radiol 2004;48:487-92. [Crossref] [PubMed]
- Bonanno N, Cioni D, Caruso D, et al. Attitudes and perceptions of radiologists towards online (virtual) oncologic multidisciplinary team meetings during the COVID-19 pandemic-a survey of the European Society of Oncologic Imaging (ESOI). Eur Radiol 2023;33:1194-204. [Crossref] [PubMed]
Cite this article as: Eqbal H, Borschmann M. Virtual multidisciplinary meetings in a new COVID-19 world: how well are we doing it? Aust J Otolaryngol 2023;6:9.