Hospital-avoidance with Outpatient Management of Epistaxis (HOME): which epistaxis patients packed with a Rapid RhinoTM are potentially appropriate for outpatient management?
Introduction
Uncontrolled epistaxis is a common reason for presentation to the emergency department in Australia. Vasoconstrictive topical measures in conjunction with silver nitrate cautery are often successful in arresting the bleeding, allowing the patient to be discharged home (1,2). In our health service if these initial measures fail, insertion of a non-dissolving carboxymethylcellulose balloon pack (Rapid RhinoTM) to tamponade the bleeding, additionally acting as a platelet aggregator and lubricator, is frequently performed (1). The literature advocates for the removal of the pack 24–72 hours after insertion (2-5), therefore once it has been inserted patients are routinely admitted to hospital for observation and pack removal (6).
A number of recent British studies have identified that the majority of patients admitted with non-dissolving balloon packing do not require other inpatient intervention and could potentially be managed at home (4,7-9). This has not been studied in Australia and it is possible there is a cohort of the Australian patient population who are also amenable to ambulatory management. Hospital admission avoidance can potentially preserve beds for more unwell patients and reduce unnecessary inpatient cost to the healthcare system (2), whilst minimising risks of inpatient nosocomial complications (10).
There is a small but significant group of patients presenting with epistaxis who have a high level of comorbidity, highlighted by a 3.4% all-cause mortality rate of inpatients with epistaxis in a British study, although epistaxis was rarely identified as the cause of death (11). The difficulty arises in predicting those patients requiring non-dissolving packing who will require active inpatient management and therefore would not be suitable for outpatient management. The aim of this study was to evaluate which patient groups may be suitable for outpatient management and to develop a risk stratification tool that can be used by ear nose and throat (ENT) departments to identify patients with epistaxis and non-dissolving packing with balloon tamponade in situ who may be suitable for outpatient management with follow-up in a Rapid Access Clinic within 48 hours. We present this article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-22-27/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved as a Quality Improvement Project by Southern Adelaide Clinical Human Research Ethics Committee (SAC HREC) and the study met criteria for exemption from such review. Individual consent for this retrospective analysis was waived.
Design
A single centre, observational, retrospective case series carried out at a tertiary hospital (Flinders Medical Centre), Adelaide, Australia.
Inclusion criteria
Adult (>18 years) patients with an emergency admission admitted under ENT with ICD-10 code of ‘epistaxis’ between 1st January 2019 and 31st December 2020. Only those requiring packing with a Rapid RhinoTM were included in analysis.
Exclusion criteria
Paediatric patients and patients undergoing elective surgery to manage recurrent epistaxis were excluded from this study.
Data collection
Data was extracted from the hospital database and patient case-notes. Patient factors included age at presentation (years), living situation (alone or with another adult), hospital catchment area [Southern Adelaide, Central Adelaide, Northern Adelaide, or regional; see Figure S1], presence of comorbidities (ischaemic heart disease or valve replacement, diabetes, stroke/transient ischaemic attack (TIA), atrial fibrillation, heart failure, significant liver disease, renal failure, cognitive impairment, bleeding disorder). Epistaxis history including number of previous admissions for epistaxis, number of presentations to medical professionals in last 30 days, previous surgical management or interventional radiology/embolisation of epistaxis was collected. Presentation systolic blood pressure (SBP) (mmHg), haemoglobin (g/L), use of antiplatelets or anticoagulants, nasal trauma, recent endonasal surgery (within last 30 days) and if blood transfusion required. Type of packing (single or bilateral Rapid RhinoTM, posterior packing) was recorded, along with the reasons for medical review, and if surgical management or interventional radiology/embolisation was required to arrest bleeding.
The primary outcome was whether unplanned medical review was required while an inpatient. This was used as a proxy to predict those who may re-present to hospital if they were not admitted for inpatient care of their epistaxis. The secondary outcome was whether a surgical procedure or radiologic embolisation was required. This represents a need for inpatient management for the patient to undergo these procedures. If significant data was not recorded, the case was excluded from analysis.
Statistics
Data was primarily categorical and is presented with descriptive statistics. Data was collated was analysed using SPSS IBM version 27 (Armonk, NY, USA). Chi-square statistical analysis was used to identify variables that were associated with the outcomes of unplanned medical review, surgical procedure/radiologic embolisation (Tables S1,S2). Univariate logistic regression was conducted to identify variables predicting unplanned medical management, or the requirement of surgical intervention or interventional radiology/embolisation. Those variables with P<0.2 on univariate logistic regression, as well as variables deemed clinically relevant, were subsequently included in multiple logistic regression to identify predictive factors. Factors identified as predictive and those deemed clinically important were compiled into a risk stratification tool to guide clinical decision making.
Results
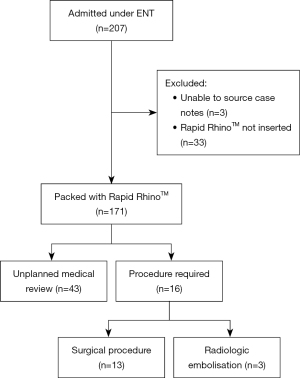
A total of 207 adult patients with epistaxis were admitted under the ENT team with 171 (82.6%) managed using a Rapid RhinoTM who were analysed further (Figure 1). Of the patients with a Rapid RhinoTM, 43 patients (25.1%) required at least one unplanned medical review with 7 patients (4%) requiring multiple medical reviews; 13 patients (7.6%) with Rapid RhinoTM required a procedure in theatre, and 3 patients (1.8%) received interventional radiology/embolisation to control epistaxis (Figure 1); 21 (12.3%) of patients had bilateral Rapid RhinoTM inserted and of these 7 (33.3%) required medical review and 1 (4.8%) required surgery and 1 (4.8%) embolisation; 3 (1.8%) required additional posterior packing and of these, 1 (33.3%) required review and 0 went on to have surgery or embolisation. The average length of stay was 32 hours (range, 3–153 hours).
Demographic data (Table 1) identified that most patients were ≥70 years (60.2%) and living in the Southern Adelaide area (80.1%). One hundred and nineteen (69.6%) of patients were taking an anticoagulant/antiplatelet medication with 51.3% of those having the medication withheld during their inpatient admission. Reasons for unplanned medical review are presented in Table 2. A total of 21 (12.3%) patients required an unplanned medical review due to concern for ongoing bleeding despite packing, with 19 (11.1%) of those patients having evidence of ongoing bleeding. Other common reasons for review were; 9 (5.3%) asymptomatic hypertension, 8 (4.7%) self-removal of nasal pack, 5 (2.9%) hypotension and 4 (9.3%) pain or discomfort.
Table 1
| Variable | N (%) |
|---|---|
| Age | |
| <50 years | 19 (11.1) |
| ≥50, <70 years | 49 (28.7) |
| ≥70 years | 103 (60.2) |
| Locality | |
| Flinders Medical Centre Catchment (SALHN) | 137 (80.1) |
| Royal Adelaide Hospital Catchment (CALHN) | 9 (5.3) |
| Adelaide Hills/Barossa/Fleurieu | 20 (11.7) |
| Regional/remote | 5 (2.9) |
| Living arrangement | |
| Alone | 47 (27.5) |
| With another adult | 102 (59.6) |
| Residential care facility | 22 (12.9) |
SALHN, Southern Adelaide Local Health Network; CALHN, Central Adelaide Local Health Network.
Table 2
| Reason for unplanned medical review | Number of reviews |
|---|---|
| Concern for bleeding—found to be bleeding | 13 |
| Concern for bleeding—no bleeding evident | 2 |
| Hypertension—asymptomatic | 7 |
| Discomfort | 4 |
| Self-removal of Rapid RhinoTM | 8 |
| Hypotension | 4 |
| Nausea and vomiting | 1 |
| Tachycardia | 4 |
| Desaturation | 2 |
| Other* | 5 |
| Total | 50 |
*, other reasons for unplanned medical review: groin haematoma, urinary retention, per rectal bleeding, agitation, hypoglycaemia.
Analysis with multivariate logistic regression revealed abnormal SBP (<90 or >170 mmHg) (P=0.002) and cognitive impairment (P=0.04) were predictive of requiring an unplanned medical review (Table 3). Recent endonasal surgery (P=0.03) and ≥1 recent previous presentation with epistaxis (P=0.009) were predictive for requiring a procedure in theatre (Table 3). Chi-square analysis indicated that severe bleeding indicated by a change in haemoglobin (≥20 g/L; P=0.001), previous surgical management or interventional radiology/embolisation of epistaxis (P<0.001) and previous admissions for epistaxis (P<0.001) were associated with requirement for interventional radiology/embolisation (Table S3). The number of patients requiring interventional radiology/embolisation was small hence logistic regression was not appropriate.
Table 3
| Variables | Medical review | Surgical procedure | |||
|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | ||
| Age group | |||||
| <50 years | 1 | 0.42 | 1 | 0.44 | |
| ≥50, <70 years | 2.56 (0.56–11.72) | 0.23 | 0.41 (0.083–1.99) | 0.27 | |
| ≥70 years | 1.92 (0.38–8.84) | 0.43 | 0.28 (0.032–2.61) | 0.25 | |
| SBP outside clinically acceptable range (<90 or >170 mmHg) | 1.56 (1.17–2.04) | 0.002 | N/A | N/A | |
| Heart disease | 1.47 (0.68–3.18) | 0.32 | 2.39 (0.35–16.33) | 0.37 | |
| Cognitive impairment | 3.08 (1.04–9.17) | 0.04 | N/A | N/A | |
| Posterior packing | 4.50 (0.61–33.37) | 0.14 | N/A | N/A | |
| Anticoagulation or antiplatelet medication | 0.72 (0.27–1.88) | 0.50 | 0.25 (0.033–1.82) | 0.17 | |
| Recent endonasal surgery | 1.35 (0.41–4.50) | 0.62 | 8.32 (1.21–57.09) | 0.03 | |
| Haemoglobin drop ≥20 g/dL | 1.61 (0.73–3.55) | 0.24 | 2.29 (0.62–8.53) | 0.22 | |
| ≥1 recent presentation with epistaxis (last 30 days) | 1.21 (0.59–2.49) | 0.60 | 7.96 (1.67–37.84) | 0.009 | |
N/A, no cases requiring surgical procedure with this factor. OR, odds ratio; CI, confidence interval.
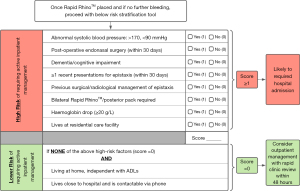
From these results, a risk stratification tool was developed (Figure 2). Factors predictive of at least one of the outcomes (unplanned medical review, surgical procedure or interventional radiology/embolisation) or deemed clinically important (i.e., posterior pack) were identified as ‘high risk’ of requiring inpatient management. Applying this stratification tool to the investigated cohort, 31% of patients had no ‘high risk’ factors and were deemed appropriate for ambulatory management with nasal pack, with subsequent follow-up in a rapid access ENT clinic within 48 hours.
Discussion
Current practice in this health system is for emergency department staff to insert a non-dissolving balloon packing (e.g., Rapid RhinoTM) for epistaxis failing to respond to topical lignocaine and phenylephrine or cautery, followed by referral to ENT and hospital admission. Product information for the Rapid RhinoTM by Smith and NephewTM indicate that the patient can be discharged following balloon inflation with follow-up in 24–72 hours (3). This study sought to identify factors that predict requirement of inpatient management of epistaxis. A risk stratification tool was designed, based on the factors identified, to categorise those patients with a nasal pack who are likely to be safe for discharge home and follow-up in a Rapid Access outpatient clinic for removal of the nasal pack (Rapid RhinoTM) within 48 hours.
Outcomes of this study are comparable with the available literature (4,12). By applying this risk stratification tool to the retrospective cohort in this study, we identified that approximately 26 patients (31%) could potentially be discharged home with a non-dissolving nasal pack in situ. The range of patients discharged in UK studies during the COVID pandemic with a non-dissolving pack in situ ranged broadly based on health service from 29.5–90% (4,8,9,12). Unplanned medical review is usually triggered by nursing staff escalating their concerns regarding their patient. In this cohort of patients an unplanned medical review was required in 25% of cases, with 9% due to concern for further bleeding. UK studies of outpatient management of patients with Rapid RhinoTM report re-presentation rates to hospital of 5.1–20.0%, with approximately 10% presenting for further bleeding (4,5,12).
This study found that 7.6% had uncontrolled bleeding despite Rapid RhinoTM who subsequently required surgical intervention, primarily those patients who had undergone recent endonasal sinus surgery, slightly higher than the literature estimated rates of 3.2–6.8% (11,13). In other cases, radiologic embolisation was required, usually in patients with recurrent epistaxis who are medically unfit for a general anaesthetic. The current study found 1.8% of patients required embolisation, similar the rate in a study by Goddard and Reiter (1.4%) (13).
Hypertension is a potential issue in the management of epistaxis as the literature suggests both pre-existing chronic hypertension and high SBP at time of presentation are associated with persistent epistaxis (14). In this study, abnormal SBP (<90, >170 mmHg) was significantly associated with increased likelihood of an unplanned medical review. Many of the reviews for asymptomatic hypertension identifies likely chronic asymptomatic hypertension may go undetected in the outpatient setting, overestimating number of patients that would likely represent to hospital for this issue (15).
Use of intranasal packing poses difficulty in patients with cognitive impairment as behavioural manifestations may lead to pulling on the pack (16). In this study, patients with cognitive impairment frequently required unplanned medical review following self-removal of the nasal pack.
Epistaxis post endonasal sinus surgery is a well-recognised complication with approximately 2.2% of patients having significant bleeding requiring readmission and/or packing (17). In this study 39% of patients who presented with epistaxis post sinus surgery required surgical intervention to control the bleeding, higher than published by Bhattacharyya [2014] who calculated a procedure was required in 1.0% and 17.9% of post endoscopic sinus surgery bleeding, at first and second presentations respectively (18).
A systematic review suggested that anticoagulants result in adverse outcomes in epistaxis, causing recurrent and heavier bleeding with increased frequencies of blood transfusion (19). This was not observed in the current study as antiplatelet/anticoagulant medication was not predictive of an unplanned medical review, surgical procedure or radiologic embolisation. There is no current protocol within our health service to withhold anticoagulation or antiplatelets. A discussion regarding the risks and benefits with the patient and the relevant teams occurs. In this retrospective dataset it was recorded as to whether antiplatelets/anticoagulation was given or held.
Risk stratification tool and implementation
As a response to the COVID pandemic, the UK-ENT network aimed to safely reduce number of patients admitted with epistaxis. This resulted in a number of publications supporting safe ambulatory management of many epistaxis patients with non-dissolving balloon packs in the absence of bilateral +/− posterior packs, significant medical comorbidities, or likely surgical intervention (8,9,12,20). Based on the results of this study, it is recommended that patients requiring Rapid RhinoTM who present with one or more of the following factors are admitted to hospital for inpatient care: abnormal blood pressure (<90, >170 mmHg), bilateral Rapid RhinoTM or posterior pack, recent endoscopic sinus surgery (within 30 days), cognitive impairment, haemoglobin drop >20 g/L, ≥1 previous presentation for epistaxis within last 30 days. If in the absence of all of these factors, discharge can be considered if the patient is independent, contactable by telephone and lives within 60 minutes of the hospital. An ENT clinic appointment within 48 hours is to be arranged prior to discharge. Given the results of this study, patients taking antiplatelet or anticoagulant medication are potentially safe for outpatient management however clinical judgement should be applied to individual cases.
While it was not assessed in this study, it may be preferable for patients to be managed at home, as demonstrated in other medical conditions (21,22). Nasal balloon packing can be uncomfortable as evidenced by 8% of medical reviews required for patient discomfort. Regular simple analgesia should be advised to patients on discharge with nasal packing with instructions if further analgesia is required. There is a movement toward use of dissolvable local haemostatic agents (such as NasoporeTM and SurgifloTM) at time of first presentation to avoid hospital admission and allow virtual follow-up (6,8). This is not currently common practice at this hospital however practice change should be considered in future.
Discharging patients safely with a Rapid RhinoTM in situ represents an area of potential cost saving for the public healthcare budget. The Independent Hospital Pricing Authority (2014-15) estimates the national cost of one bed day in Australia is AUD $1,901 (23). Based on the rounded average length of stay (2 days), if 26 (31%) of patients were discharged annually, an estimated annual saving of $98,852 would be realized for the healthcare budget. This hospital avoidance strategy for treating patients with epistaxis would improve inpatient bed flow and help reduce strain on the hospital system—an essential consideration for management of hospital resources during COVID-19 pandemic.
The rate of medical reviews in this study is expected to overestimate the rate of unplanned representation for the following reasons: (I) abnormal vital signs may necessitate a review while the patient may be asymptomatic; (II) a medical review is more accessible as an inpatient therefore patients are more likely to request review for other/unrelated symptoms. Another limitation is that the population features two clinically contrasting patient groups; those older, more comorbid patient on blood thinning medication, and those younger, post endonasal sinus surgery which makes statistical analysis more difficult. Further limitations include the use of a dataset from a single-centre, the inherent constraints of retrospective data and a small sample size which limit the external validity of this study.
Conclusions
Epistaxis represents an area where appropriately selected patients with non-dissolving balloon packing such as Rapid RhinoTM can be safely and effectively managed as outpatients thus potentially reducing bed pressures in Australian hospitals. This retrospective study has identified patient groups that are associated with increased risk of requiring inpatient management. Using these results, a risk stratification tool was created to assess suitability of patients, presenting with epistaxis in the emergency setting, for outpatient management. The next step is implementation of this proposed stratification tool for prospective evaluation.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-22-27/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-22-27/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-22-27/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-22-27/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved as a Quality Improvement Project by Southern Adelaide Clinical Human Research Ethics Committee (SAC HREC) and the study met criteria for exemption from such review. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pope LE, Hobbs CG. Epistaxis: an update on current management. Postgrad Med J 2005;81:309-14. [Crossref] [PubMed]
- Heining CJ, Amlani A, Doshi J. Ambulatory management of common ENT emergencies - what's the evidence?. J Laryngol Otol 2021;135:191-5. [Crossref] [PubMed]
- Smith and Nephew. RAPID RHINO, Product Usage Instructions 2016. Available online: https://rapidrhino.com/rapid-rhino-product-usage-instructions/
- Van Wyk FC, Massey S, Worley G, et al. Do all epistaxis patients with a nasal pack need admission? A retrospective study of 116 patients managed in accident and emergency according to a peer reviewed protocol. J Laryngol Otol 2007;121:222-7. [Crossref] [PubMed]
- Singer AJ, Blanda M, Cronin K, et al. Comparison of nasal tampons for the treatment of epistaxis in the emergency department: a randomized controlled trial. Ann Emerg Med 2005;45:134-9. [Crossref] [PubMed]
- Toppi J, Chan SW, Pratap U, et al. Cost effectiveness of posterior epistaxis management using a gelatin-thrombin matrix or Rapid Rhino. Aust J Otolaryngol 2020;3:14. [Crossref]
- Upile T, Jerjes W, Sipaul F, et al. A change in UK epistaxis management. Eur Arch Otorhinolaryngol 2008;265:1349-54. [Crossref] [PubMed]
- Devabalan Y, Cereceda-Monteoliva N, Lorenz H, et al. Coronavirus disease 2019: changing the future of emergency epistaxis management. J Laryngol Otol 2021;135:675-9. [Crossref] [PubMed]
- Stansfield J, Dobbs S, Harrison R, et al. Management of ENT emergencies during the coronavirus disease 2019 pandemic. J Laryngol Otol 2021;135:117-24. [Crossref] [PubMed]
- Fernando-Canavan L, Gust A, Hsueh A, et al. Measuring the economic impact of hospital-acquired complications on an acute health service. Aust Health Rev 2021;45:135-42. [Crossref] [PubMed]
- Epistaxis 2016: national audit of management. J Laryngol Otol 2017;131:1131-41. [Crossref] [PubMed]
- Admission avoidance in acute epistaxis: A prospective national audit during the initial peak of the COVID-19 pandemic. Clin Otolaryngol 2021;46:577-86. [Crossref] [PubMed]
- Goddard JC, Reiter ER. Inpatient management of epistaxis: outcomes and cost. Otolaryngol Head Neck Surg 2005;132:707-12. [Crossref] [PubMed]
- Terakura M, Fujisaki R, Suda T, et al. Relationship between blood pressure and persistent epistaxis at the emergency department: a retrospective study. J Am Soc Hypertens 2012;6:291-5. [Crossref] [PubMed]
- Australian Bureau of Statistics. National Health Survey: First Results, Australia 2017–18, Canberra, Australia; 2018.
- Hessler JB, Schäufele M, Hendlmeier I, et al. Behavioural and psychological symptoms in general hospital patients with dementia, distress for nursing staff and complications in care: results of the General Hospital Study. Epidemiol Psychiatr Sci 2018;27:278-87. [Crossref] [PubMed]
- Dalziel K, Stein K, Round A, et al. Endoscopic sinus surgery for the excision of nasal polyps: A systematic review of safety and effectiveness. Am J Rhinol 2006;20:506-19. [Crossref] [PubMed]
- Bhattacharyya N. Unplanned revisits and readmissions after ambulatory sinonasal surgery. Laryngoscope 2014;124:1983-7. [Crossref] [PubMed]
- Khan M, Conroy K, Ubayasiri K, et al. Initial assessment in the management of adult epistaxis: systematic review. J Laryngol Otol 2017;131:1035-55. [Crossref] [PubMed]
- ENT-UK, Covid-19 Epistaxis Management, accessed through. 19th February 2023. Available online: https://asohns.org.au/Portals/6/COVID-19%20Resources/ENTUK_COVID%2019%20Epistaxis%20Management.pdf?ver=2021-01-11-115458-123
- Rosinsky PJ, Chen SL, Yelton MJ, et al. Outpatient vs. inpatient hip arthroplasty: a matched case-control study on a 90-day complication rate and 2-year patient-reported outcomes. J Orthop Surg Res 2020;15:367. [Crossref] [PubMed]
- Joo EH, Rha SY, Ahn JB, et al. Economic and patient-reported outcomes of outpatient home-based versus inpatient hospital-based chemotherapy for patients with colorectal cancer. Support Care Cancer 2011;19:971-8. [Crossref] [PubMed]
- Independent Hospital Pricing Authority. National Hospital Cost Data Collection Cost Report: Round 19 Financial Year 2014-15. IHPA; 2016.
Cite this article as: Footner L, Woods CM, Huang L, Ooi EH. Hospital-avoidance with Outpatient Management of Epistaxis (HOME): which epistaxis patients packed with a Rapid RhinoTM are potentially appropriate for outpatient management? Aust J Otolaryngol 2023;6:15.