Burnout in Australian Otorhinolaryngology Head and Neck Surgery consultants during the coronavirus disease 2019 (COVID-19) pandemic
Introduction
The stressful nature of the medical profession leads to increased risks of burnout among physicians. Burnout was described by Dr. Christina Maslach as ‘a syndrome of emotional exhaustion and cynicism’ (1). It is becoming increasingly prevalent, especially within the medical profession with rates ranging from 20% to 85% in the literature (2). The current gold standard for identifying burnout in medical professionals is the Maslach Burnout Inventory (3). The Maslach Burnout Inventory (MBI) tool is a validated 22 question survey that assesses burnout over 3 dimensions; emotional exhaustion, depersonalization and reduced personal accomplishment (1). A study by Beyondblue has identified a high prevalence of mental health issues in Australian doctors and medical students (4). Occupational burnout has impacts that extend beyond the way in which we carry out our jobs and can affect multiple aspects of our lives. In terms of our patients, burnout has been associated with deterioration in the quality of care and service provided which can result in increased errors, poorer patient outcomes and patient dissatisfaction (3). In terms of personal lives, burnout has been correlated with family and marital problems, as well as increased use of drugs and alcohol, effects on mental health, depression and suicide (2,5).
A recent study from 2019 identified high rates of burnout among Otolaryngology Registrars in Australia of around 73% (6). This study highlighted the high demands of the surgical training program and levels of stress experienced by trainees. Geelan-Hansen [2018] reported on the occurrence of burnout in not only otolaryngology residents but also consultants across a variety of specialties, with a particularly high vulnerability to mid-career surgeons (7). Compounding this is the significant impact of the coronavirus disease 2019 (COVID-19)-pandemic on the mental health of the population as a whole but more specifically on healthcare professionals. Australia experienced four waves of COVID-19 since the beginning of the pandemic (8). The first wave affected all states and territories across Australia between March and April of 2020. The second wave occurred in the Winter of 2020 with most cases documented in Victoria. It was not until the following Winter of 2021 that there was another wave primarily affecting New South Wales and Victoria. The fourth wave begun in December 2021 with cases across all states and territories (8).
A study is, therefore, needed to explore if the high rate of burnout in Australian Otolaryngology Head and Neck Surgery (OHNS) trainees translates to burnout in OHNS consultants. Our study aims to assess burnout using a standardized instrument and explore the effect of various demographic, clinical practice, and lifestyle covariates on burnout levels in a nation-wide cohort of practicing Australian Society of Otolaryngology Head and Neck Surgery (ASOHNS) surgeons during COVID-19. Our survey was performed at a time between the second and third COVID-19 waves where there was not a significant burden of disease (8). We present this article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-21/rc).
Methods
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Central Adelaide Local Health Network Human Research Ethics Committee (reference number: 12322). Informed consent was taken from all individual participants. An anonymous cross-sectional survey was created using the online platform, SurveyMonkey (https://www.surveymonkey.com). The survey was initially distributed through the Royal Australasian College of Surgery (RACS) newsletter however due to limited responses it was sent to the ASOHNS for consideration. The survey link and consent form were subsequently distributed via email to all practicing consultant ASOHNS members using a database held by ASOHNS. The survey was initially distributed to ASOHNS members on the 15th of March 2021 with subsequent re-distribution on the 16th of April to maximize response numbers. Completion of the survey in its entirety was not required for available data to be included. Missing data from incomplete questionnaires was excluded from further analysis.
Respondents initially completed a series of demographic questions relating to lifestyle, family and work (Appendix 1). A series of questions related to the impact COVID-19 was having on their personal and work lives were assessed with a five-point Likert scale (Appendix 2). Finally, respondents’ level of burnout was assessed using the Maslach Burnout Inventory—Human Services Survey for Medical Personnel. The Maslach Burnout Inventory is a series of 22 statements regarding job-related feelings, three examples are provided in Appendix 3. Burnout was defined when a high threshold was met in one or more of the three MBI domains, as guided by previously established cut-off scores (6). High levels of emotional exhaustion, depersonalization and reduced personal accomplishment were ≥27, ≥14 and ≤30 respectively.
Statistical analysis
Analysis of categorical data was performed using Chi-square and Fisher’s exact tests as appropriate. Covariates predictive of burnout were tested in univariable logistic regression models with (absence versus presence of) burnout as the binary outcome, P values were always two-sided. All analyses were performed using the Scientific Python library (“scipy”; version 1.5.4) and R (version 4.0.2) through the Jupyter notebook interface.
Results
Demographic data
A total of 117 out of the 490 members responded to our survey, giving a completion rate of 24%. Demographic information is outlined in Table 1. The majority of respondents were from New South Wales (30%), Queensland (29%) or Victoria (22%), married (85%) and aged between 40–59 years (67%). In regards to gender, 80% of our responses were from males and 20% from females. Of the 490 ASOHNS members, there was a higher response rate from females (31%) compared to males (23%). A significant proportion of respondents did not have a regular general practitioner (GP) (44%). Of those who did have a GP, the majority only saw them once per year. The Centers for Disease Control and Prevention (CDC) currently recommends up to one standard drink of alcohol per day for women and two standard drinks per day for men. 18% of respondents consumed more alcohol compared to these CDC recommendations. In regards to workload, the majority of consultants worked in major city hospitals, more than 40 hours per week with a mix of public and private workload and averaging none to two nights on call per week.
Table 1
| Demographics | Participants, % [n] |
|---|---|
| Gender | |
| Male | 80 [94] |
| Female | 20 [23] |
| Relationship | |
| Married | 85 [100] |
| De facto | 5 [6] |
| Widowed | 1 [1] |
| Single | 3 [4] |
| Divorced | 5 [6] |
| Practice location | |
| Capital/major city | 78 [91] |
| Large regional | 17 [20] |
| Small regional | 5 [6] |
| Age, years | |
| 30–39 | 8 [9] |
| 40–49 | 36 [42] |
| 50–59 | 31 [36] |
| 60–69 | 15 [17] |
| 70+ | 11 [13] |
| Children | |
| None | 22 [26] |
| 1 or more | 78 [91] |
| State | |
| SA | 10 [12] |
| NT | 0 |
| Queensland | 29 [34] |
| ACT | 0 |
| Victoria | 22 [26] |
| NSW | 30 [35] |
| WA | 8 [9] |
| Tasmania | 1 [1] |
| Reviews with GP | |
| Every year | 42 [49] |
| Every 6 months | 10 [12] |
| Every 3 months | 3 [4] |
| Monthly | 1 [1] |
| I don’t have a regular GP | 44 [51] |
ASOHNS, Australian Society of Otolaryngology Head and Neck Surgery; SA, South Australia; NT, Northern Territory; ACT, Australian Capital Territory; NSW, New South Wales; WA, Western Australia; GP, general practitioner.
Burnout
Of the 117 respondents, 42 (36%) met a high level of burnout in at least one of the MBI domains. Breaking this down, 27 (23%) were burnt out in a single domain, 10 (9%) in 2 domains and 5 (4%) in all three. The most common domain in which participants met burnt out criteria was emotional exhaustion, identified in 33 (28%) participants. High depersonalization and reduced sense of personal accomplishment were found in 14 (12%) and 15 (13%) participants respectively. The demographic factors that correlated with burnout, although not reaching statistical significance included marital status (P=0.92), age (P=0.19), gender (P=0.23), area of practice (P=0.25) and alcohol consumption (P=0.09), see Table 2.
Table 2
| Personal/work characteristic | Participants, n | Percentage of category burnt out, % | Odds ratio (95% CI) | P value | |
|---|---|---|---|---|---|
| Burnt out | Not burnt out | ||||
| Marital status | 0.92 | ||||
| Divorced | 2 | 4 | 33 | ||
| De facto | 2 | 4 | 33 | ||
| Married | 36 | 64 | 36 | ||
| Single | 2 | 2 | 50 | ||
| Widowed | 0 | 1 | 0 | ||
| Age, years | 0.19 | ||||
| 30–39 | 5 | 4 | 56 | ||
| 40–49 | 19 | 23 | 45 | 0.66 (0.15–2.84) | 0.58 |
| 50–59 | 9 | 27 | 25 | 0.27 (0.05–1.21) | 0.09 |
| 60–69 | 4 | 13 | 24 | 0.25 (0.04–1.34) | 0.11 |
| 70+ | 5 | 8 | 38 | 0.50 (0.08–2.78) | 0.43 |
| Gender | 0.23 | ||||
| Female | 11 | 12 | 48 | ||
| Male | 31 | 63 | 33 | 0.54 (0.21–1.37) | 0.19 |
| State of practice | 0.25 | ||||
| ACT | 0 | 0 | 0 | ||
| NSW | 17 | 18 | 49 | ||
| NT | 0 | 0 | 0 | ||
| Queensland | 9 | 25 | 26 | 0.38 (0.13–1.03) | 0.06 |
| SA | 5 | 7 | 42 | 0.76 (0.19–2.83) | 0.68 |
| Tasmania | 1 | 0 | 100 | ||
| Victoria | 7 | 19 | 27 | 0.39 (0.13–1.13) | 0.09 |
| WA | 3 | 6 | 33 | 0.53 (0.10–2.35) | 0.42 |
| Alcohol consumption as guided by the CDC | |||||
| Not applicable | 1 | 4 | 20 | ||
| Less than recommended | 18 | 37 | 33 | ||
| As recommended | 11 | 25 | 31 | 0.90 (0.36–2.22) | 0.83 |
| More than recommended | 12 | 9 | 57 | 2.74 (0.99–7.90) | 0.06 |
| Frequency of working weekends | 0.06 | ||||
| Always | 3 | 2 | 60 | ||
| Often | 8 | 13 | 38 | 0.38 | |
| Sometimes | 16 | 27 | 37 | 0.33 | |
| Rarely | 4 | 23 | 15 | 0.12 (0.01–0.93) | 0.04 |
| Never | 11 | 10 | 52 | 0.76 | |
| Reviews with GP | |||||
| Every year | 17 | 32 | 49 | 1.59 (0.19–33.59) | 0.39 |
| Every 6 months | 6 | 6 | 50 | 3.00 (0.29–70.88) | 0.85 |
| Every 3 months | 1 | 3 | 25 | ||
| Monthly | 1 | 0 | 100 | ||
| No regular GP | 17 | 34 | 33 | 1.50 (0.18–31.58) | 0.01 |
CI, confidence interval; ACT, Australian Capital Territory; NSW, New South Wales; NT, Northern Territory; SA, South Australia; WA, Western Australia; CDC, Centers for Disease Control and Prevention; GP, general practitioner.
Personal burnout
Looking at burnout by marital status we found that those who were single had the highest rate of burnout. This is limited though by singles making up only 3% of all respondents with 85% of respondents married, 6% de facto and 6% divorced. There was also a trend towards younger consultants experiencing higher rates of burnout with 56% of those aged 30–39 years being burnt out. In terms of the gender disparity, for female and male consultants there was a burnout rate of 48% and 33% respectively.
Occupational burnout
When we considered regions of work, we found that those who worked in New South Wales and South Australia had the highest rates of burnout with 49% and 42% respectively. A higher proportion of respondents working in small regional centers (n=4, 67%) experienced burnout compared to those in large regional centers (n=9, 45%) or major cities (n=29, 32%). There was also a correlation between burnout and consuming more than the recommended amounts of alcohol. 57% of respondents who consumed more than CDC recommendations were found to be burnt out compared to 31% of those who consumed recommended amounts or less.
Frequency of working weekends was a statistically significant factor when considering levels of burnout in our cohort. We found that ASOHNS consultants that rarely worked on weekends had one-tenth the risk of being burnt out compared to those who always worked weekends [odds ratio (OR) =0.12; P=0.04]. There may be a suggestion that working fewer weekends is protective of burnout.
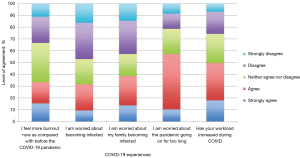
COVID-19 experiences
COVID-19 experiences were assessed by asking respondents how much they agreed or disagreed with five COVID-related statements, see Appendix 2. Overall there was a trend towards respondents’ workload having increased during COVID-19 as well as a concern that the pandemic will go on for too long. Respondents neither significantly agreed nor disagreed when asked about concerns for themselves or their families becoming infected and feelings of more burnout compared to before the pandemic (Figure 1).
Discussion
This study has shown a rate of burnout in ASOHNS consultants that has been similarly identified in previous reports (3,9,10,11). The risk factors we identified as correlating with burnout in the Australian population, although not statistically significant, included being young, single, female, working in rural practice and higher alcohol consumption. Rarely working weekends did, however, show a statistically significant negative correlation with burnout compared to those who always worked weekends.
Our study not only contributes to the existing literature on burnout in surgical specialties but also has provided a comparison to the cohort of Australian ENT trainees that were surveyed in 2017 (6). We found that of the ASOHNS consultants in our study, 36% met a high level of burnout. This is similar to rates from overseas, which report burnout occurring in 41% of consultant surgeons across the UK and Ireland (11). In comparison, ASOHNS trainees experienced burnout at more than twice the rate (73%) (6). A systematic review of burnout in surgeons by Galaiya et al. in 2020 also demonstrated both young age and level of training to have an inverse relationship with burnout as measured with the MBI (2). The reduced levels of burnout identified in consultants may be a secondary effect of other protective factors that are more commonly reflected in this population compared to trainees. These factors include the presence of a partner, being married and having children. 78% of our cohort compared to only 48% of the Australian OHNS trainee cohort analyzed by Raftopulos [2019] had children. We can also speculate that in comparison to trainees, consultants are more likely to have children who are both older and also more independent. In addition to this, 90% of our cohort was either married or in a de facto relationship. These demographic factors have been reflected in the literature with the presence of a partner, being married and having children all correlating with a reduced risk of burnout (2,5,11). These findings are likely a reflection of the support family and friends provide especially given the differences in emotional exhaustion noted between Australian OHNS consultants and trainees (28% vs. 70%).
Interestingly, our findings with respect to geographical correlation with burnout are also consistent with previous studies (6). Raftopulos [2019] found that South Australia and New South Wales reported the highest rates of burnout for OHNS trainees. Similar findings were noted in this study with these two regions also reporting the highest rates of burnout. This finding may be a reflection of the possible long-term effects and existence of burnout. Alternatively, these findings may reflect statewide issues regarding the health, wellbeing and support available to OHNS trainees and consultants.
Looking at geographical differences it is also important to consider the impacts COVID-19 had on individual states within Australia. The Australian Institute of Health and Welfare reported on the number and rate of COVID-19 related deaths across the Australian states and territories (8). This report identified that New South Wales and Victoria accounted for more than 80% of COVID-19 related deaths in Australia (38% and 46% respectively) (8). Victoria and New South Wales also recorded the highest mortality rates (364 and 248 deaths per million respectively) with the lowest rates in Western Australia and the Northern Territory (15 and 41 deaths per million respectively) (8). These rates were also reflected in the local measures implemented by each state to control the spread of COVID-19. During 2021, Victoria enforced the most stringent policies including multiple stay at home orders and over 170 days of school closures within its capital city, Melbourne (12). These policies likely contributed to the differences seen in burnout rates across the Australian states and territories. Our finding of higher burnout rates in respondents from small regional centers must be analyzed with caution given the small numbers in both the small and large regional center subgroups.
Our results have also displayed a correlation between higher than recommended alcohol consumption and burnout. This finding may reflect an important negative response to burnout. Alcohol misuse has been associated with both short- and long-term adverse effects including injuries, heart disease, liver disease and cancer (13). Further to this, alcohol misuse can have implications on practitioners’ ability to perform at work and delivery of safe and effective patient care (3).
Frequency of working weekends was one of the main findings from our study. We found that ASOHNS consultants that rarely worked weekends were significantly less likely to be burnt out compared to those who always worked weekends. However, this data must be analyzed with caution given no significant difference was seen between those who never worked weekends compared to those who always worked weekends. This finding was also noted in a cross-sectional study of burnout among United States otolaryngologists where number of weekends worked was also one of the predictors of burnout (10). The correlation between weekends worked and burnout may be a secondary effect of hours worked as well as the impact working weekends has on an individual’s ability to spend time with family and perform recreational activities.
The effect of COVID-19 was the final aspect that was assessed in our study. We reflected on a recent survey conducted in Wuhan, China of burnout in frontline and Oncology workers (14). In both studies most respondents agreed with concerns about the pandemic going on for too long. There was, however, a difference noted in regard to respondents’ concerns for themselves and their family members becoming infected. Most respondents from Wuhan agreed with these concerns whereas most Australian respondents disagreed with these statements. A notable difference between these groups though is that the survey in Wuhan was conducted in March 2020 when COVID-19 was considered under control. In comparison, we conducted our survey in March 2021 when most states in Australia were in strict lockdowns with the focus on COVID-19 elimination prior to widespread community transmission. Given these different timelines, we can speculate that the experiences of those who worked through COVID-19 in Wuhan may have made them more cautious and vigilant in regards to contracting COVID-19.
This prospective cross-sectional study has reported on a large subset of practicing ASOHNS consultants to identify factors correlating with burnout during COVID-19. This study, however, is also associated with some inherent limitations based on our study design. The cross-sectional nature of the study only allows for correlation and does not allow us to identify causation. Having only received responses from 24% of the ASOHNS members, there also exists the potential for selection bias. Despite these limitations, the data collected through this study provides valuable insight into burnout in Australian doctors and contributes to the current body of literature available on burnout.
Conclusions
Ideally, being able to re-survey a group of surgical trainees during and after they have completed their training will provide a more accurate longitudinal comparison of burnout. Based on the current available data though, we may speculate that burnout exists in higher levels in our surgical trainees and that more support is required across the board, but more specifically for our junior doctors.
Currently the Royal Australian College of Surgery offers multiple supports in the form of hotlines, wellbeing documents as well as online modules. A potential area for improvement is that these services all require self-recognition of physicians’ own burnout for them to seek out this information. Developing more proactive strategies to reach out to those who may be unaware of their own burnout should be something to consider.
Further information and support is available through the Royal Australasian College of Surgeons and ASOHNS websites as well as beyond blue and lifeline.
Acknowledgments
The authors acknowledge the Australian Society of Head and Neck Surgery for help with distribution of the survey.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-23-21/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-23-21/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-21/prf
Funding:
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-21/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Central Adelaide Local Health Network Human Research Ethics Committee (reference number: 12322). Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav 1981;2:99-113. [Crossref]
- Galaiya R, Kinross J, Arulampalam T. Factors associated with burnout syndrome in surgeons: a systematic review. Ann R Coll Surg Engl 2020;102:401-7. [Crossref] [PubMed]
- Bartholomew AJ, Houk AK, Pulcrano M, et al. Meta-Analysis of Surgeon Burnout Syndrome and Specialty Differences. J Surg Educ 2018;75:1256-63. [Crossref] [PubMed]
- National Mental Health Survey of Doctors and Medical Students. beyondblue 2013 – [cited 2020 May]. Available from: https://medicine.uq.edu.au/files/42088/Beyondblue%20Doctors%20Mental%20health.pdf
- Amanullah S, Ramesh Shankar R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthcare (Basel) 2020;8:421. [Crossref] [PubMed]
- Raftopulos M, Wong EH, Stewart TE, et al. Occupational Burnout among Otolaryngology-Head and Neck Surgery Trainees in Australia. Otolaryngol Head Neck Surg 2019;160:472-9. [Crossref] [PubMed]
- Geelan-Hansen K, Anne S, Benninger MS. Burnout in Otolaryngology-Head and Neck Surgery: A Single Academic Center Experience. Otolaryngol Head Neck Surg 2018;159:254-7. [Crossref] [PubMed]
- The impact of a new disease: COVID-19 from 2020, 2021 and into 2022. Australian Institute of Health and Welfare 2022 – [cited 2023 July 10]. Available online: https://www.aihw.gov.au/getmedia/c017fa79-be4b-4ad5-bbf3-2878ed0995e5/aihw-aus-240_Chapter_1.pdf.aspx
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012;172:1377-85. [Crossref] [PubMed]
- Golub JS, Johns MM 3rd, Weiss PS, et al. Burnout in academic faculty of otolaryngology-head and neck surgery. Laryngoscope 2008;118:1951-6. [Crossref] [PubMed]
- Balendran B, Bath MF, Awopetu AI, et al. Burnout within UK surgical specialties: a systematic review. Ann R Coll Surg Engl 2021;103:464-70. [Crossref] [PubMed]
- Variation in policy response to COVID-19 across Australian states and territories. Blavatnik School of Government 2022 – [cited 2023 July 11]. Available online: https://www.bsg.ox.ac.uk/sites/default/files/2022-06/BSG-WP-2022-046_1.pdf
- Alcohol Use and Your Health. Centers for Disease Control and Prevention 2022 – [cited 2022 January 14]. Available online: https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm
- Wu Y, Wang J, Luo C, et al. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J Pain Symptom Manage 2020;60:e60-5. [Crossref] [PubMed]
Cite this article as: Lee TJ, Bassiouni A, Wilkie MD, Foreman A, Krishnan S, Hodge JC. Burnout in Australian Otorhinolaryngology Head and Neck Surgery consultants during the coronavirus disease 2019 (COVID-19) pandemic. Aust J Otolaryngol 2024;7:16.