
Presentation and management of acute epiglottitis over a 10-year period in a rural setting: a retrospective cohort study
Introduction
Epiglottitis represents a potentially life-threatening illness, particularly with acute airway obstruction. Since the introduction of the Haemophilus influenzae type-b (Hib) vaccination, multiple studies have noted a fall in the incidence of paediatric acute epiglottitis (1-4). A multi-centre study from Melbourne, Australia published in 2018 found no microbiological evidence of Haemophilus influenzae type-b in 93 patients presenting with epiglottitis (5). To our knowledge, there is little data available on management of epiglottitis in rural Australia. Dubbo Base Hospital and Orange Health Service are the two referral hospitals with an Ear, Nose and Throat (ENT) service for the Western New South Wales Health District, which covers an area of 246,676 square kilometres (6). A recent meta-analysis demonstrated declining rates of airway intervention for acute epiglottitis over a forty-year period to 10% (7).
The primary objective was to review the demographics, presentation, investigation and management for rural patients presenting with acute epiglottitis. The secondary objective was to analyse factors implicated in need for airway intervention. Our hypotheses were that the rates of airway intervention would be higher when compared to available literature, due to the need to transfer patients safely from peripheral hospitals and the intermittent availability of otolaryngologists leading to a lower threshold for airway intervention when they were available, and that most microbiological organisms would be due to gram-positive bacteria such as Streptococcus.
Methods
A retrospective analysis of medical records was conducted for patients admitted to Dubbo Base Hospital and Orange Hospital over a ten-year period. Patient presentations from 1st January 2014 to 31St December 2023 were searched using the Cerner Discern Analytics 2.0 program, as part of the Cerner Powerchart electronic medical record. Search terms for admitting diagnoses were “epiglottitis”, “acute epiglottitis” and “acute epiglottitis and supraglottitis”. The study is reported according to the STROBE reporting guidelines (available at https://www.theajo.com/article/view/10.21037/ajo-24-87/rc).
Inclusion criteria were any patient admitted to Dubbo Base Hospital or Orange Hospital over a 10-year period with a confirmed diagnosis of epiglottitis via direct visualiation or radiologically. This study excluded paediatric cases as it is policy that children with epiglottitis are transferred to a tertiary paediatric unit with paediatric intensive care support. Data collected from the medical records included demographic features, distance from home to a base hospital, presenting signs and symptoms, vaccination status if known, past medical history, smoking status, any background of head and neck cancer, fibreoptic or direct laryngoscopy findings, pathology results, imaging results, microbiology results, management including type of airway intervention, intensive care unit (ICU) admission and length of stay (LoS), complications and mortality and availability of an otolaryngologist.
Data were analysed using R studio (8). Comparison for continuous variables that were not normally distributed on Kolmogorov-Smirnov test was performed using Mann-Whitney U-test. Continuous variables with normal distribution were compared using Student’s t-test. Categorical variable associations were analysed using Pearson’s Chi-squared test or Fisher’s exact test for count data less than 10. Univariate analysis presented as odds ratios (ORs) and 95% confidence intervals (CIs) were used when comparing multiple variables. Missing data were highlighted and excluded from statistical analysis. A P value less than 0.05 was considered statistically significant.
The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was reviewed by the Executive Officer of the Greater Western Human Research Ethics Committee (HREC) and advised that no ethical risks requiring submission to an HREC have been identified in accordance with NSW Health Policy (GL2007_020). Patient confidentiality was maintained by anonymising data, and individual consent was waived for this retrospective analysis.
Results
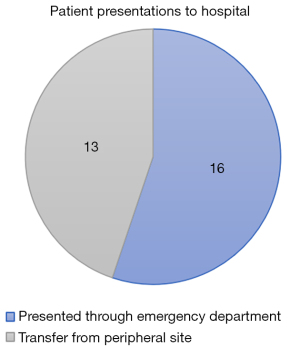
There were 29 adult patients and zero paediatric cases included for analysis over the ten-year period. The median age was 45 years old [interquartile range (IQR) 32–57, mean 47±17 years] with a slight male predominance (n=16, 55.2%). The vaccination status of the cohort was largely unknown with only four patients (13.8%) having known vaccination status against Haemophilus influenza type-b. Thirteen patients (44.8%) were active smokers and seven (24.1%) had a background of diabetes. More than half (n=16, 55.2%) presented via the Emergency Department and the remainder (n=13, 44.8%) were transferred from peripheral hospitals, with six patients (20.7%) requiring a transfer distance of more than 100 kilometres (Figure 1).
Clinical presentation and diagnosis
The median duration of symptoms at original presentation was 2 days (IQR <24 hours to 3 days). The most common symptoms were sore throat (n=28, 96.6%), odynophagia (n=25, 86.2%), dysphagia (n=17, 58.6%), dysphonia (n=17, 58.6%), dyspnoea (n=17, 58.6%) and subjective fevers (n=12, 41.4%). There were eight patients (27.6%) with stridor on examination and seven patients (24.1%) with inability to manage upper airway secretions. Median temperature on arrival was 37 ℃ (IQR 36.6–38.1 ℃), median respiratory rate was 20 breaths per minute (IQR 17–24 breaths per minute), and three (10.3%) patients required supplemental oxygen therapy. Of those patients transferred from peripheral hospitals, eight were diagnosed with epiglottitis radiologically [seven on computed tomography (CT) and one with lateral neck X-ray] and the remaining five were clinically suspicious for epiglottitis and were transferred for further investigation and management. Almost all patients (n=28, 96.6%) underwent fibreoptic nasendoscopy at the base hospital to confirm epiglottitis, with the remaining patient diagnosed based on radiological findings. Four patients (13.8%) had lateral neck X-rays and 17 (58.6%) had CT of the neck. The mean white cell count (WCC) was 14.8 (±6.2) ×109/L and median C-reactive protein (CRP) was 61 mg/L (IQR 18–174 mg/L).
Management and outcomes
There were 12 patients (41.4%) who underwent airway intervention, seven (24.1%) of these via awake fibreoptic nasotracheal intubation, four (13.8%) with direct laryngoscopy and one patient (3.4%) who had three failed attempts at intubation before proceeding to emergency cricothyroidotomy and subsequently semi-elective tracheostomy (Table 1). Of the 12 patients requiring airway intervention, 11 of these were performed in the Operating Theatre and one was performed in the Emergency Department. There were three instances of airway intervention without an otolaryngologist available. Of these patients, one had failed intubation and subsequent cricothyroidotomy with hypoxic arrest with full neurological recovery, one underwent successful awake fibreoptic nasotracheal intubation at a peripheral site prior to transfer, and one underwent successful intubation with video laryngoscopy. Two patients were transported from peripheral sites by the State-Wide Retrieval Service, with the remainder transferred via ambulance. Most patients (n=24, 82.8%) were admitted to ICU for monitoring and the median hospital LoS was 3 days (IQR 2–5 days). No patients required transfer to tertiary centres.
Table 1
| Airway management | N (%) |
|---|---|
| Observation and medical therapy | 17 (58.6) |
| Awake fibreoptic nasotracheal intubation | 7 (24.1) |
| Direct laryngoscopy/video laryngoscopy intubation | 4 (13.8) |
| Failed intubation requiring cricothyroidotomy | 1 (3.4) |
All patients were managed with intravenous antibiotics and corticosteroids. The most common antibiotic choices were ceftriaxone (n=22, 75.9%) and cefotaxime (n=3, 10.3%). There were 12 patients (41.4%) who had samples sent for culture. Of these patients, eight had both throat and blood cultures taken, whilst four had throat cultures only. Eight patients had no growth on cultures, two had Streptococcus pyogenes on throat swabs, one had Streptococcus anginosus on throat swab and one patient had both Streptococcus pneumoniae and Pseudomonas aeruginosa isolated in blood culture bottles.
One patient had a hypoxic cardiac arrest during intubation but made a full neurological recovery and was discharged home from hospital after 12 days. There was one (3.4%) mortality in the cohort caused by hypoxia during awake fibreoptic intubation leading to pulseless electrical activity (PEA) cardiac arrest. The patient underwent cardiopulmonary resuscitation, with 23 minutes of downtime, before return of spontaneous circulation. The patient subsequently developed Multiple Organ Dysfunction Syndrome and passed away 4 days later.
Factors associated with airway intervention
Clinical factors associated with airway intervention (Table 2) included inability to tolerate upper airway secretions (OR 13, 95% CI: 1.7–390, P=0.011), stridor (OR 6.7, 95% CI: 1.1–62, P=0.038), higher temperature (median 37.8 ℃ compared to 36.8 ℃, P=0.041), higher heart rate (median 116 per minute compared to 94 per minute, P=0.049) and higher respiratory rate (median 24 per minute compared to 18 per minute, P=0.034). There was no association between smoking (P=1) and airway intervention. There was a non-significant association between diabetes and need for airway intervention (OR 4.9, 95% CI: 0.8–45.4 P=0.092). There was no significant difference between WCC (P=0.96) and CRP (P=0.51) of the group that required airway intervention and those that did not. There was no significant association (P=0.24) in distance from a base hospital and requirement for airway intervention.
Table 2
| Variable | Airway intervention (n=12) | No airway intervention (n=17) | Odds ratio (95% CI) | P value |
|---|---|---|---|---|
| Inability to tolerate upper airway secretions | 6/12 (50.0) | 1/17 (5.9) | 13 (1.7–390) | – |
| Stridor | 6/12 (50.0) | 2/17 (11.8) | 6.7 (1.1–62) | – |
| Diabetes mellitus | 5/12 (41.7) | 2/17 (11.8) | 4.9 (0.8–45.4) | – |
| Smoker | 5/12 (41.7) | 8/17 (47.1) | 0.8 (0.2–3.7) | – |
| Temperature (℃) | 37.8 [36.9–38.8] | 36.8 [36.5–37.3] | – | 0.041 |
| Heart rate (beats per minute) | 116 [97–126] | 94 [81–112] | – | 0.049 |
| Respiratory rate (breaths per minute) | 24 [20–28] | 18 [16–20] | – | 0.034 |
| White cell count (109/L) | 14.8±7.0 | 14.7±5.8 | – | 0.96 |
| C-reactive protein (mg/L) | 72.5 [20–252] | 60 [18–159] | – | 0.51 |
Data are presented as n/N (%), median [IQR] or mean ± SD. OR and 95% CI were calculated using univariate logistic regression. Continuous variables were compared using the Mann-Whitney U-test or Student’s t-test, as appropriate. Categorical variables were analysed using Pearson’s Chi-squared test or Fisher’s exact test. A P value <0.05 was considered statistically significant. CI, confidence interval; IQR, interquartile range; OR, odds ratio; SD, standard deviation.
Discussion
This cohort had a high rate of airway intervention (41%) compared to a recent meta-analysis demonstrating declining rates of airway intervention to 10% (7). There was one death in the cohort as well as one cardiac arrest with full neurological recovery, highlighting the serious nature of acute epiglottitis and the potential risk for upper airway obstruction and subsequent hypoxia.
There were several limitations for this study. Firstly, the retrospective nature of the study is a potential source of selection bias, particularly as missing documentation could lead to under-reporting of vaccination status, co-morbidities, symptoms, and examination findings in the cohort. Paediatric patients were excluded from our cohort as any paediatric cases of epiglottitis would likely have been managed acutely in the Emergency Department before requiring retrieval to a tertiary centre with paediatric intensive care support, therefore never being admitted to hospital locally. Finally, we were unable to access archived ICU documentation for patients and relied on the discharge summaries copied into the electronic medical records.
Our cohort had a slight male predominance with a median age of 45 years old and most common symptoms being sore throat, odynophagia, dysphagia, dysphonia and dyspnoea, similar to previous literature (5,9-12). Several studies have noted the decreasing rates of epiglottitis amongst the paediatric population since the widespread introduction of the Hib vaccination (3,4,9,13). All bar one patient in the cohort underwent fibreoptic nasendoscopy to confirm a diagnosis of acute epiglottitis, which remains the gold-standard investigation (14). Our cohort had relatively high rates of airway intervention (41%) compared to previous studies (10–29%) (5,9,10,12,13). It is beyond the scope of this study to examine factors driving the higher rates of airway intervention, which are likely complex and multi-factorial. Possible factors include barriers to accessing healthcare in rural locations leading to delayed presentations, a more conservative approach to airway management due to less resources and need to transport patients safely over vast distances (15,16). One quarter of the patients had their airways secured without an otolaryngologist available. In one of these cases, there was failure to intubate and subsequent hypoxic cardiac arrest requiring cricothyroidotomy, highlighting the issue of managing epiglottitis in a resource-limited setting. Many of the peripheral sites within the health district do not have access to medical imaging and five patients were transferred based on clinical history and examination. The decision on whether patients needed their airway secured prior to transfer and the involvement of a retrieval specialist was based on the clinical judgement of those at the peripheral sites.
Less than half of the patients in our cohort had samples sent for microbiology and it is unclear from the medical documentation as to the rationale for some patients not having microbiology collected, particularly those that were febrile. There were no positive microbiological samples for Hib in our cohort, with Streptoccocus being the most common organism. This is reflective of the literature, suggesting a significant reduction in incidence of Hib following widespread vaccination (3,5,17,18). Unfortunately, we were unable to draw any conclusions about vaccination rates in this cohort due to the largely missing data. Our mortality rate (3%) was likely reflective of a small sample size, with mortality rates of 1% reported in a large retrospective study (19).
In our cohort, factors associated with need for airway intervention included inability to tolerate upper airway secretions, stridor, higher temperature, higher heart rate and higher respiratory rate on presentation. This represents similar findings to previous studies (5,18). A 2019 systematic review found that stridor, diabetes mellitus and presence of abscess were the strongest predictors for airway intervention (20). Our cohort demonstrated a trend towards diabetes mellitus being associated with airway intervention but was likely under powered to demonstrate statistical significance (OR 4.9, 95% CI: 0.8–45.4; P=0.092).
Overall, our cohort appears congruent with available literature in terms of clinical presentation, diagnosis and factors associated with airway intervention. However, this rural cohort had significantly higher rates of airway intervention than suggested in the literature, limiting the external validity. It raises the need for further research into management of life-threatening illnesses such as acute epiglottitis in resource-limited settings.
Conclusions
This rural cohort had a high rate of airway intervention when compared to recent literature. Further research could investigate the factors associated with this. Our study identified stridor, inability to tolerate upper airway secretions, increased temperature, increase heart rate, and increased respiratory rate as signs and symptoms that can aid decision making regarding the need for airway intervention.
Acknowledgments
Our abstract has been presented as a poster at the New Zealand Society of Otolaryngology Head & Neck Surgery’s 77th Annual General and Scientific Meeting, Hamilton, New Zealand, taking place between 15th and 18th October, 2024. It has also been accepted for poster presentation at the Australia Society of Otolaryngology Head & Neck Surgery’s 75th Annual Scientific Meeting, Sydney, Australia, taking place between 28th and 30th March, 2025.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-24-87/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-24-87/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-24-87/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-24-87/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was reviewed by The Executive Officer of the Greater Western Human Research Ethics Committee (HREC) and advised that no ethical risks requiring submission to an HREC have been identified in accordance with NSW Health Policy (GL2007_020). Patient confidentiality was maintained by anonymizing data, and individual consent was waived for this retrospective analysis.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McIntyre PB, Leeder SR, Irwig LM. Invasive Haemophilus influenzae type b disease in Sydney children 1985-1987: a population-based study. Med J Aust 1991;154:832-7. [Crossref] [PubMed]
- Wurtele P. Acute epiglottitis in children and adults: A large-scale incidence study. Otolaryngology–Head and Neck Surgery 1990;103:902-8. [Crossref] [PubMed]
- Wood N, Menzies R, McIntyre P. Epiglottitis in Sydney before and after the introduction of vaccination against Haemophilus influenzae type b disease. Intern Med J 2005;35:530-5. [Crossref] [PubMed]
- Shah RK, Roberson DW, Jones DT. Epiglottitis in the Hemophilus influenzae type B vaccine era: changing trends. Laryngoscope 2004;114:557-60. [Crossref] [PubMed]
- Baird SM, Marsh PA, Padiglione A, et al. Review of epiglottitis in the post Haemophilus influenzae type-b vaccine era. ANZ J Surg 2018;88:1135-40. [Crossref] [PubMed]
- About Western NSW Local Health District: NSW Government; 2024. Available online: https://www.nsw.gov.au/departments-and-agencies/wnswlhd/about-us
- Booth AWG, Pungsornruk K, Llewellyn S, et al. Airway management of adult epiglottitis: a systematic review and meta-analysis. BJA Open 2024;9:100250. [Crossref] [PubMed]
- Team R. R Studio. 1.3.1093 ed. Boston, MA: RStudio Team; 2020.
- Guldfred LA, Lyhne D, Becker BC. Acute epiglottitis: epidemiology, clinical presentation, management and outcome. J Laryngol Otol 2008;122:818-23. [Crossref] [PubMed]
- Riffat F. Acute Epiglottitis in Adults: A 10-Year Review. Otolaryngology–Head and Neck Surgery 2010;143:156. [Crossref]
- Chroboczek T, Cour M, Hernu R, et al. Long-term outcome of critically ill adult patients with acute epiglottitis. PLoS One 2015;10:e0125736. [Crossref] [PubMed]
- Bizaki AJ, Numminen J, Vasama JP, et al. Acute supraglottitis in adults in Finland: review and analysis of 308 cases. Laryngoscope 2011;121:2107-13. [Crossref] [PubMed]
- Shah RK, Stocks C. Epiglottitis in the United States: national trends, variances, prognosis, and management. Laryngoscope 2010;120:1256-62. [Crossref] [PubMed]
- Cox GJ, Bates GJ, Drake-Lee AB, et al. The use of flexible nasoendoscopy in adults with acute epiglottitis. Ann R Coll Surg Engl 1988;70:361-2. [PubMed]
- Mullan L, Armstrong K, Job J. Barriers and enablers to structured care delivery in Australian rural primary care. Aust J Rural Health 2023;31:361-84. [Crossref] [PubMed]
- Baker T, Moore K, Lim J, et al. Rural emergency care facilities may be adapting to their context: A population-level study of resources and workforce. Aust J Rural Health 2022;30:393-401. [Crossref] [PubMed]
- Hermansen MN, Schmidt JH, Krug AH, et al. Low incidence of children with acute epiglottis after introduction of vaccination. Dan Med J 2014;61:A4788. [PubMed]
- Guardiani E, Bliss M, Harley E. Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: evolving principles in diagnosis and management. Laryngoscope 2010;120:2183-8. [Crossref] [PubMed]
- Hanna J, Brauer PR, Berson E, et al. Adult epiglottitis: Trends and predictors of mortality in over 30 thousand cases from 2007 to 2014. Laryngoscope 2019;129:1107-12. [Crossref] [PubMed]
- Sideris A, Holmes TR, Cumming B, et al. A systematic review and meta-analysis of predictors of airway intervention in adult epiglottitis. Laryngoscope 2020;130:465-73. [Crossref] [PubMed]
Cite this article as: Schnitzler N, Ridha H, Sirigiri R. Presentation and management of acute epiglottitis over a 10-year period in a rural setting: a retrospective cohort study. Aust J Otolaryngol 2025;8:19.


