
Administration of corticosteroids into the middle ear does not limit steroid-induced side effects
Practicing as a Renal Physician for 30+ years, my medical history includes 45 years of type 1 diabetes mellitus and development of sudden onset sensorineural deafness.
Last year, a left sensory neural deafness developed (no aetiology found) and both high dose oral prednisone and subsequently intratympanic methylprednisolone injections, followed by intratympanic dexamethasone [different Ear, Nose and Throat (ENT) surgical opinions, as to the benefit of one over the other], were administered, resulting in some improvement, but still not a full recovery.
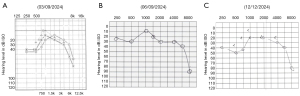
This year, the right ear developed the same issue (Figure 1). Oral prednisolone 50 mg/day was prescribed, reducing to zero, over three weeks. Follow up audiogram, four weeks later, showed improvement in the low frequencies, but subsequent audiogram, a month later, demonstrated a deterioration again, prompting the insertion of a grommet to administer intratympanic dexamethasone (24 mg/mL), 0.5 mL alternate daily for 2 weeks. A subsequent audiogram demonstrated some improvement so another course of intratympanic dexamethasone was prescribed.
The issue with intratympanic steroid administration is that its absorption is 100% from swallowing the eustachian tube drainage, and whatever is absorbed from the middle ear. 12 mg dexamethasone equals 75 mg prednisone (1).
The steroid side effects included insomnia, tremor, anger management issues and having to increase the insulin dose by 250%. This occurred with both episodes of hearing disorder in 2023 and 2024. Oral prednisone side effects were identical. The proof of absorption came with a morning cortisol, taken 48 hours after the last injection, being highly suppressed at 44 nmol/L (normal range, 130–650 nmol/L). This resulted in a mild Addisonian crisis several days later, blood pressure 90/72 mmHg, which responded to low dose prednisone.
This raises the need to consider weaning intratympanic steroids in a similar way to weaning oral prednisone.
Back in 1980, Wilson et al. first demonstrated in a double blind controlled trial the efficacy of steroids in the treatment of idiopathic sudden hearing loss (2). Patients who received systemic corticosteroids recovered their hearing significantly more often than patients receiving placebo (61% vs. 32%). Intratympanic injection of corticosteroids in humans for sensorineural hearing loss was pioneered by Silverstein in 1996 (3).
Treatment options for sensorineural deafness have been covered in both a Cochrane review (4) and a clinical practice guideline (5). The Cochrane review suggested most of the evidence was low- or very low-certainty, therefore it is hoped that further studies may change the conclusions. This review does suggest checking blood sugar levels when treating with steroids, but it is rarely done in clinical trials. Rohrmeier studied the risk of corticosteroid-induced hyperglycaemia and concluded that the prevalence during systemic therapy is high and rises as the dose increases (6).
Although the rate of occurrence of side effects with systemic corticosteroid therapy appears low, systematic data recording and publication of the proposed side effects are still insufficient and adverse effects from a short course of high-dose systemic corticosteroids have not been documented with good evidence (7).
Intratympanic steroids are prescribed in sensorineural deafness as they are considered to have minimal systemic effects but may have local reactions of pain, tympanic membrane perforation, transient dizziness, greater cost and multiple visits if not administered via a grommet. Patients with certain medical conditions, such as insulin-dependent or poorly controlled diabetes, unstable hypertension, tuberculosis, gastric ulcer disease, glaucoma, or prior psychiatric reactions to corticosteroids, may not be able to receive oral corticosteroids. Treatment efficacy will not be reduced using intratympanic steroid injections (8).
With the existence of potential adverse treatment effects, this case reflects the shared decision making between the attending otolaryngologist and the patient (albeit a nephrologist) negotiating both the dosages and duration of both oral and intratympanic steroid use (5).
To conclude, could some practice points be highlighted? The dose of corticosteroids prescribed intratympanically is very high and can result in significant systemic absorption, with subsequent substantial steroid-induced side effect issues. Consider weaning the dose of intratympanic steroids over time, similar to systemic steroids, so as not to precipitate a hypocortisol state.
Acknowledgments
None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Funding: None.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-24-84/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ClinCalc LLC. Corticosteroid Conversion Calculator. [15 Dec 2024]. Available online: https://clincalc.com/corticosteroids/
- Wilson WR, Byl FM, Laird N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol 1980;106:772-6. [Crossref] [PubMed]
- Silverstein H, Choo D, Rosenberg SI, et al. Intratympanic steroid treatment of inner ear disease and tinnitus (preliminary report). Ear Nose Throat J 1996;75:468-71, 474, 476 passim. [Crossref] [PubMed]
- Plontke SK, Meisner C, Agrawal S, et al. Intratympanic corticosteroids for sudden sensorineural hearing loss. Cochrane Database Syst Rev 2022;7:CD008080. [PubMed]
- Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg 2019;161:S1-S45. [Crossref] [PubMed]
- Rohrmeier C, Koemm N, Babilas P, et al. Sudden sensorineural hearing loss: systemic steroid therapy and the risk of glucocorticoid-induced hyperglycemia. Eur Arch Otorhinolaryngol 2013;270:1255-61. [Crossref] [PubMed]
- García-Berrocal JR, Ramírez-Camacho R, Lobo D, et al. Adverse effects of glucocorticoid therapy for inner ear disorders. ORL J Otorhinolaryngol Relat Spec 2008;70:271-4. [Crossref] [PubMed]
- Mirian C, Ovesen T. Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg 2020;146:421-8. [Crossref] [PubMed]
Cite this article as: Roger SD, Kertesz T. Administration of corticosteroids into the middle ear does not limit steroid-induced side effects. Aust J Otolaryngol 2025;8:21.


