
Drug-induced sleep endoscopy (DISE): a retrospective review in Western Australian children
Introduction
Sleep disordered breathing (SDB) is an umbrella term that describes a spectrum of abnormal respiratory patterns and functions during sleep (1). Obstructive sleep apnoea (OSA) falls within this entity and is characterised by upper airway collapse or narrowing during sleep (2). The long-term sequelae of OSA are significant if left untreated and can result in neurocognitive and behavioural disturbances, cardiovascular complications, poor growth, and decreased quality of life (2). Up to 5% of children worldwide are affected by OSA (3), but it is even more prevalent in children with predisposing conditions and comorbidities. For example, in children with trisomy 21 (Down syndrome) OSA is estimated at 30–70% (4,5).
Among the various modalities used to diagnose SDB in children, polysomnography (PSG) is considered the gold standard (1). Although PSG findings help confirm the existence and severity of OSA, they do not provide information on the anatomical site causing upper airway obstruction (6). Drug-induced sleep endoscopy (DISE) can characterise the site and pattern of obstruction contributing to OSA and is a valuable diagnostic tool for assessing the paediatric upper airway (7). A flexible fibreoptic endoscope is passed via the nasal passage whilst the patient is in a drug-induced sleep-like state (8). DISE is often performed when there is persistent obstruction after adenotonsillectomy (AT), but it may also assist in surgical planning to evaluate the candidacy of children before AT (9,10).
Available data on DISE in Australian paediatric OSA patients is limited. This study aims to review our experience within the population of Western Australian children with OSA and how this compares with the literature, specifically by determining the demographics of the children that are having the procedure and the indications, levels of airway collapse during DISE, and identifying the most common DISE-directed surgeries performed.
Methods
Study design
This study is a retrospective chart review of paediatric patients who underwent a DISE at a single tertiary hospital [Perth Children’s Hospital (PCH)] in Western Australia between 2018 and 2021. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the ethics board of the Children’s and Adolescent Health Service (CAHS) Clinical Governance Unit [Governance Evidence Knowledge Outcomes (GEKO) Quality Activity #46967] and individual consent for this retrospective analysis was waived. The data collection process adhered to ethical guidelines, ensuring confidentiality and anonymity of all individuals involved.
The STROBE reporting guideline, accessed online through Enhancing the QUAlity and Transparency Of health Research (EQUATOR), was used in manuscript preparation (available at https://www.theajo.com/article/view/10.21037/10.21037/ajo-24-55/rc).
Patient population
Patients were limited to the paediatric population (≤16 years old). Patients were identified using the Theatre Management System (TMS) software to assess cases listed as ‘nasoendoscopy’ or ’sleep endoscopy’. Patients who underwent DISE, either as a primary procedure or in combination with another procedure, were included. Whereas those who underwent a simple nasoendoscopy were excluded. Demographic data, procedural findings and operative details were collected. A de-identified database was created using patients’ records and documentation.
DISE
DISE was performed by multiple surgeons within the unit, ranging from supervised otolaryngology trainee or fellow to Consultant paediatric ear, nose, and throat (ENT) surgeon. Patients were positioned supine with head in a neutral position. There is no standardised anaesthetic protocol in the unit (also reflecting the lack of universal consensus on the optimal sedation protocol for DISE in children). However, the general practice is to maintain spontaneous respiration (‘drug-induced sleep state’) following induction of anaesthesia, and ensuring adequate sedation to tolerate endoscopy. No single scoring system is consistently used within the unit, but the VOTE (velum, oropharynx, tongue base, epiglottis) classification is the most commonly utilised. Obstruction is assessed at each anatomical sub-site as either no obstruction, partial obstruction, or complete obstruction.
Objectives
The objectives were to describe the demographics of children with OSA who required DISE in the only tertiary paediatric institution serving Western Australia, and to identify the most common sites of obstruction diagnosed at the time of DISE as well as the most common DISE-directed surgical interventions in this population.
Statistical methods
In this study, descriptive statistics were used to assess and summarise the characteristics, findings, and surgical interventions performed in paediatric patients undergoing DISE. The central tendency of the data was represented by the mean, while the standard deviation was used to assess the variability around the mean, providing insights into the consistency of results across the sample.
Bias
Given that this study was conducted at a single centre, the participant sample may be at risk of potential selection bias. However, all paediatric patients referred for DISE were included in this study, applying the aforementioned inclusion/exclusion criteria. This was to ensure a diverse range of patients across varying degrees of severity and comorbidities were included, and reflects the typical clinical practice within the centre. Inter-operator variability is an additional source of potential bias, particularly in a paediatric cohort where anatomical and physiological differences can be more pronounced. To minimize variability, all DISE procedures followed a similar, albeit not identical, protocol for sedation and operator-training for endoscopic examination. Missing data, resulting from incomplete records or loss to follow-up, was addressed by excluding cases with insufficient clinical information and using available alternative data sources to supplement missing values, where possible.
Results
Forty-one paediatric patients who underwent DISE during the 4 years of this retrospective review were studied. Patient demographics and characteristics are shown in Table 1. There were 17 female (41.5%) and 24 male (58.5%) patients, with ages ranging from six months to 15 years (mean 6.2±4.1 years).
Table 1
| Patient characteristics | Value |
|---|---|
| Age at DISE (years) | 6.2±4.1 |
| Gender | |
| Female | 17 (41.5) |
| Male | 24 (58.5) |
| BMI (kg/m2) | 18.2±4.8 |
| BMI percentile† | |
| Underweight (<5%) | 4 (9.8) |
| Normal range (5–85%) | 22 (53.7) |
| Overweight (>85–95%) | 4 (9.8) |
| Obese (>95%) | 11 (26.8) |
| Comorbidities | |
| Yes | 34 (82.9) |
| No | 7 (17.1) |
| Surgical history | |
| Surgically-naïve | 13 (31.7) |
| Previous adenotonsillectomy | 28 (68.3) |
| Anatomical obstruction site | |
| Multiple sites | 34 (82.9) |
| Single site | 7 (17.1) |
| Adenoid | 1 (14.3) |
| Supraglottitis | 1 (14.3) |
| Tongue base | 5 (71.4) |
| Adenoid/tonsillar hypertrophy‡ | |
| Adenoid | |
| 0 | 12 (29.3) |
| 1 | 10 (24.4) |
| 2 | 12 (29.3) |
| 3 | 5 (12.2) |
| 4 | 2 (4.9) |
| Tonsil | |
| 0 | 21 (51.2) |
| 1 | 4 (9.8) |
| 2 | 7 (17.1) |
| 3 | 9 (22.0) |
| 4 | 0 |
| Surgical intervention following DISE | |
| Yes | 33 (80.5) |
| No | 8 (19.5) |
| Polysomnography | |
| Pre-operative | 37 (90.2) |
| OAHI (events/hour)§ | 11.0±17.6 |
| SpO2 nadir (%) | 81.9±11.4 |
Data were presented as mean ± standard deviation or n (%). †, based on Centres for Disease and Prevention (CDC) guidelines; ‡, using Brodsky grading scale 1–4 where 0 = no tissue present; §, OAHI is a measure of the number of apnoeas and hypopneas per hour recorded during a PSG. Obstructive sleep apnoea (OSA) is classified as mild (OAHI between 1 and <5), moderate (OAHI 5–9), or severe (OAHI ≥10). BMI, body mass index; DISE, drug-induced sleep endoscopy; OAHI, Obstructive Apnoea Hypopnoea Index; PSG, polysomnography; SpO2, peripheral oxygen saturation.
Comorbidities
The vast majority (n=34, 83%) of patients in this cohort had comorbidities, most of which were considered congenital or syndromic (n=27), and a small number had a history of prematurity or global developmental delay (n=7). Trisomy 21 was the most commonly occurring syndrome overall, with 14 patients having this diagnosis (52%, n=14/27). There were as many as 12 different congenital diagnoses, as outlined in Figure 1.
BMI
Approximately half of the study population were of normal weight with a BMI between 5–84% (n=22, 53.7%), in accordance with Centres for Disease and Prevention (CDC) age-adjusted BMI percentile charts. A third of patients had a BMI greater than the 85th percentile, with four patients qualifying as overweight (9.8%) and 11 patients as obese (26.8%). Four patients (9.8%) were considered underweight (BMI <5%).
Indications for DISE
Among the 41 patients in this study, 28 patients (68%) had previously undergone an AT and were undergoing investigation for residual or recurrent OSA (rOSA). The remaining 13 (31.7%) were surgically naïve, of which the most common indication for DISE was a craniofacial abnormality present in 5 (38.5%) of these cases—including Robin sequence in two patients, Goldenhar syndrome in one patient, Oculoauriculovertebral Spectrum Disorder in one patient, and micrognathia in one patient. Laryngomalacia was documented in three patients (23%). Additionally, there were individual cases of vocal cord paralysis, obesity, trisomy 21, Di George syndrome with tracheoesophageal fistula, and trisomy 13. A significant proportion of patients (82.9%) had pre-operative PSG testing, with an average Obstructive Apnoea Hypopnoea Index (OAHI) of 11.0±17.6 and SpO2 nadir of 81.9%±11.4%.
Obstruction
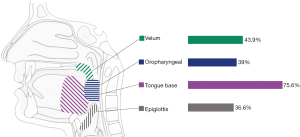
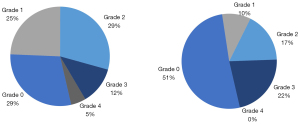
Multilevel obstruction was the most common finding in 83% of patients (n=34/41). Each obstruction site was assessed for frequency as a positive finding, as illustrated in Figure 2. The tongue base emerged as the most frequently obstructed site among all patients (75.6%). Moreover, it exhibited the highest severity of obstruction, with complete obstruction at the base of the tongue noted in 20 patients. Obstruction at the velopalatal, pharyngeal and epiglottic levels was observed in 43.9%, 39%, and 36.6% of cases, respectively. Additionally, the grading of tonsil and adenoid size and obstruction across all patients was also collated and illustrated in Figure 3.
Surgical intervention
Surgical interventions were performed at the time of DISE in 80% of patients (n=33/41), guided by their examination findings. Table 2 lists all procedures performed, alone or in combination, based on DISE findings. The population was further categorised into two groups: surgically naïve patients and those who had undergone a prior AT. In surgically-naïve patients, the most common procedure was AT (n=7/13, 53.8%). In patients with previous AT, revision adenoidectomy (n=13/28, 46%) was the most frequent DISE-directed surgery. Although eight patients did not proceed to surgical intervention, half of them had plans created from the information obtained from DISE for future surgery. These second-stage procedures included midline posterior glossectomy, turbinoplasty, lingual tonsillectomy and vocal fold lateralisation with arytenoidectomy.
Table 2
| Intervention | Total (n=41) | Surgically-naïve (n=13) | Prior AT (n=28) |
|---|---|---|---|
| No intervention | 8 | 2 | 6 |
| Adenotonsillectomy (+/− ICTA) | 7 | 7 | 0 |
| ICT | 4 | 1 | 3 |
| Completion tonsillectomy | 1 | 0 | 1 |
| Revision adenoidectomy | 13 | 0 | 13 |
| Adenoidectomy | 2 | 1 | 1 |
| Cautery of turbinates +/− turbinoplasty | 7 | 0 | 7 |
| Tongue base reduction | 5 | 1 | 4 |
| Lingual tonsillectomy | 1 | 0 | 1 |
| Supraglottoplasty | 2 | 1 | 1 |
AT, adenotonsillectomy; DISE, drug-induced sleep endoscopy; ICT, intracapsular tonsillectomy; ICTA, intracapsular tonsillectomy and adenoidectomy.
Discussion
Over the past decade, the utilisation of DISE for managing paediatric OSA has become widespread among sleep surgeons. Despite this, there are no publications from Australasia regarding the role of DISE in children from this region. The aim of this study was to assess the role of DISE in an Australian tertiary paediatric institution and report on the demographics, obstruction characteristics, and the types of DISE-directed surgery in comparison to the existing international literature.
Although there was no significant difference in this study, there was noted to be a higher percentage of male to female children requiring DISE (roughly 60:40), in accordance with existing literature which often indicates a higher prevalence of males undergoing such evaluations (12). The average age of patients, 6.2±4.1 years, is similar in comparison to other studies analysed in the review by Arganbright et al., ranging from 1.5 to 10.2 years (6).
Comorbidities play a substantial role in paediatric OSA, influencing both its development and management (7). Consistent with findings reported by Durr et al. (13), this study highlighted a high prevalence of comorbidities among children undergoing DISE. This reinforced the bidirectional relationship between OSA and associated conditions identified by Gleeson et al.—OSA may predispose children to certain conditions, and certain conditions may predispose children to OSA (14). The fact that trisomy 21 was the most common syndromic diagnosis among patients is unsurprising, considering its known tendency to cause upper airway problems and its association with a variety of specific birth defects and medical conditions (15,16). It is also the most common syndrome referenced in the literature on OSA (13,15,17-23). This is echoed in a series of paediatric patients undergoing DISE by Adler et al. in which 66.6% of patients had trisomy 21 (23). In contrast, it is still a higher incidence when compared to other studies, such as Raposo et al. (30% and 24% in their surgically naïve and rOSA cohort, respectively) (22), as well as Durr et al. (only 38% of their study population) (13). This may be explained by selective use of DISE in complex cases or those who have failed conventional treatment.
Obesity also featured prominently, with 26.8% of patients affected; a figure similar to that reported by Raposo et al. for surgically naïve children (22). Li et al. stated that for every unit (kg/m2) increase in BMI above the 50th percentile, there is a 12% increase in the risk for OSA (24). Interestingly, the slightly elevated obesity rate (36%) among patients who had already undergone AT prior to DISE may reflect the well-known risk factor for rOSA that is obesity (25). A couple studies’ lower obesity prevalence in their study underscores potential variations due to the small sample size and patient selection (20,21).
The primary indication for DISE in patients within the study population was rOSA post-AT (68.3%, n=28), which supports the findings by Arganbright et al. that this is the most common indication for children undergoing DISE (6). Among the 13 surgically-naïve patients, craniofacial abnormalities and syndromic diagnoses were frequent indications, reflecting the complexities that often necessitate DISE in these cases. Complex paediatric patients with SDB are discussed at fortnightly multidisciplinary team (MDT) meetings. These involve paediatric sleep physicians, paediatric ENT surgeons, oral and maxillofacial surgeons (OMFS), and plastic and reconstructive surgeons (PRS), among other specialists and allied health professionals. Based on the patient’s history and clinical findings, including PSG, an individualised plan for intervention—whether that be CPAP therapy, medical treatment, or surgery—is developed during the MDT discussion. This collaborative approach ensures that the management plan is tailored to the specific needs of each patient. Given the scarcity of data in the Australasian literature, this detailed, multidisciplinary approach is important to highlight, particularly when considering the management of such complex cases.
As in much of the literature, multilevel obstruction was pervasive in the study population (83% of patients), suggesting it is a common finding among patients referred for DISE. The tongue base was the most frequent site of obstruction in 75.6% of the patient cohort, a finding corroborated by several studies including Yeung et al., Durr et al., and Manickam et al. (13,26,27). In fact, akin to results illustrated in Figure 2, a systematic review by Manickam et al. (which included assessment with cine-magnetic resonance imaging as well as DISE) found that the tongue base was the most commonly described site, followed by adenoids (secondary to regrowth), inferior turbinates, velum, and the lateral oropharyngeal walls (27). This, however, contrasts the obstruction patterns demonstrated in the aforementioned studies by Raposo et al. and Amos et al., where tonsillar and adenoidal obstruction predominated (22,28). The difference is likely due to a predominance of surgically naïve patients, but again highlights AT as an important part of surgical planning.
In this study, 80% of children who underwent DISE had a therapeutic surgical intervention in the same session, emphasising its role in guiding immediate treatment decisions. AT was the most frequent DISE-directed intervention in surgically naïve patients (53.8%), reinforcing its status as the first-line management for paediatric OSA (25,29). Conversely, revision adenoidectomy was the most common procedure (46%) in patients who had previously undergone AT prior to DISE. This would suggest that adenoid regrowth is a common factor in children with rOSA and should be considered in the AT consent process, as well as emphasised in children with risk factors for rOSA.
This information can assist with targeted surgical approaches for specific patient populations, based on prior surgery or lack thereof. These findings are mirrored by Esteller et al., who reported AT to be the most frequent DISE-directed surgery in healthy children with OSA, and adenoidectomy to be the next most common (30). He et al. similarly found the most often performed DISE-directed procedure to be revision adenoidectomy (48%); however, tonsillectomy (27%) was third in line, superseded by supraglottoplasty (38%) (31).
Additional procedures, such as tongue base reduction surgery (midline posterior glossectomy), turbinoplasty, lingual tonsillectomy and vocal fold lateralisation with arytenoidectomy, were performed. However, pharyngoplasty was not part of the surgical repertoire compared to other studies (30,31). This reflects the comprehensive approach necessary for addressing multilevel obstructions identified in DISE. Collu et al. validated the shared understanding that children with rOSA (after AT) often require additional procedures to address other sites of obstruction. They also demonstrated that children with conventional OSA and no risk factors are unlikely to have rOSA after AT, reinforcing the unit’s practice of AT as the primary management approach for these patients. Nonetheless, their results also recommend a role for DISE in children who are surgically naïve with severe OSA or small tonsils, as 17.5% in this subgroup required additional surgical interventions (32).
Several limitations should be considered when interpreting this study’s findings. One limitation, which is evident in many other studies, is the lack of a standardised scoring system for DISE assessment. This introduces variability in reporting and comparability across studies. The series generally described DISE findings in the operative notes rather than given a numerical score according to a specific system. Still, even if a scoring system was used routinely, the choice of which single one to adopt could be a subject of debate. Wilcox et al. described at least six different scoring systems being used in the literature to report paediatric DISE outcomes [VOTE, sleep endoscopy-rating scale (SERS), Chan, Bachar, Fishman, Boudewyns] (33). Most centres described by Adler et al. use the VOTE scoring system (velum, oropharynx, tongue base, epiglottis) (23). Interestingly, despite being a common cause of OSA in children (34), nasal obstruction is not a level that is addressed within the VOTE framework. The recent International Paediatric Otolaryngology Group (IPOG) consensus on DISE scoring recommends a three-point scale to score anatomical sub-site of obstruction, which should include the nasal passages, adenoids, velum, lateral pharyngeal walls, tonsils, tongue base, epiglottis and arytenoids (35). Another limitation of DISE, in general, is the potential for varying depths of anaesthesia, which may affect the pattern of upper airway obstruction. Currently, there is no accepted standardised bispectral index (BIS) score or consensus for anaesthetic protocol (23). Other limitations specific to this study include the retrospective design and small study size. While this is typical of other publications on DISE, it does stress the need for larger multi-centred studies to validate these observations. The retrospective nature of this study introduces potential bias, particularly with documentation being variable and incomplete. As all study data comes from a single tertiary centre, the authors also acknowledge the effect of selection bias.
Conclusions
This study offers valuable insights into the utilisation and outcomes of DISE in paediatric patients with OSA in Western Australia. The findings highlight the predominance of multilevel obstruction, with the tongue base emerging as the most frequently obstructed site. A significant proportion of patients undergoing DISE were comorbid, with congenital or syndromic conditions being prevalent, notably trisomy 21. Surgical intervention guided by DISE findings was common, with AT and revision adenoidectomy being the most frequently performed procedures. These findings are consistent with other international series. The recognition that AT and revision adenoidectomy are the most common interventions is an essential guide for pre-operative counselling. These results contribute to our understanding of the demographic and clinical characteristics of paediatric OSA patients undergoing DISE and emphasise the importance of tailored surgical management in this population. Further research and multidisciplinary collaborative efforts are warranted to enhance our understanding of the role of DISE in optimising therapeutic strategies for paediatric OSA.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-24-55/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-24-55/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-24-55/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-24-55/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the ethics board of the Children’s and Adolescent Health Service (CAHS) Clinical Governance Unit [Governance Evidence Knowledge Outcomes (GEKO) Quality Activity #46967] and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Garde AJB, Gibson NA, Samuels MP, et al. Recent advances in paediatric sleep disordered breathing. Breathe (Sheff) 2022;18:220151. [Crossref] [PubMed]
- Kaditis AG, Alonso Alvarez ML, Boudewyns A, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 2016;47:69-94. [Crossref] [PubMed]
- Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012;130:e714-55. [Crossref] [PubMed]
- DelRosso LM. Epidemiology and Diagnosis of Pediatric Obstructive Sleep Apnea. Curr Probl Pediatr Adolesc Health Care 2016;46:2-6. [Crossref] [PubMed]
- Hill CM, Evans HJ, Elphick H, et al. Prevalence and predictors of obstructive sleep apnoea in young children with Down syndrome. Sleep Med 2016;27-28:99-106. [Crossref] [PubMed]
- Arganbright JM, Lee JC, Weatherly RA. Pediatric drug-induced sleep endoscopy: An updated review of the literature. World J Otorhinolaryngol Head Neck Surg 2021;7:221-7. [Crossref] [PubMed]
- Akkina SR, Ma CC, Kirkham EM, et al. Does drug induced sleep endoscopy-directed surgery improve polysomnography measures in children with Down Syndrome and obstructive sleep apnea? Acta Otolaryngol 2018;138:1009-13. [Crossref] [PubMed]
- Chen J, He S. Drug-induced sleep endoscopy-directed adenotonsillectomy in pediatric obstructive sleep apnea with small tonsils. PLoS One 2019;14:e0212317. [Crossref] [PubMed]
- Friedman NR, Parikh SR, Ishman SL, et al. The current state of pediatric drug-induced sleep endoscopy. Laryngoscope 2017;127:266-72. [Crossref] [PubMed]
- Boudewyns A, Verhulst S, Maris M, et al. Drug-induced sedation endoscopy in pediatric obstructive sleep apnea syndrome. Sleep Med 2014;15:1526-31. [Crossref] [PubMed]
- Lumeng JC, Chervin RD. Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc 2008;5:242-52. [Crossref] [PubMed]
- Durr ML, Meyer AK, Kezirian EJ, et al. Drug-induced sleep endoscopy in persistent pediatric sleep-disordered breathing after adenotonsillectomy. Arch Otolaryngol Head Neck Surg 2012;138:638-43. [Crossref] [PubMed]
- Gleeson M, McNicholas WT. Bidirectional relationships of comorbidity with obstructive sleep apnoea. Eur Respir Rev 2022;31:210256. [Crossref] [PubMed]
- Santos RA, Costa LH, Linhares RC, et al. Sleep disorders in Down syndrome: a systematic review. Arq Neuropsiquiatr 2022;80:424-43. [Crossref] [PubMed]
- Sherman SL, Allen EG, Bean LH, et al. Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev 2007;13:221-7. [Crossref] [PubMed]
- Maris M, Verhulst S, Saldien V, et al. Drug-induced sedation endoscopy in surgically naive children with Down syndrome and obstructive sleep apnea. Sleep Med 2016;24:63-70. [Crossref] [PubMed]
- Maris M, Verhulst S, Wojciechowski M, et al. Sleep problems and obstructive sleep apnea in children with down syndrome, an overwiew. Int J Pediatr Otorhinolaryngol 2016;82:12-5. [Crossref] [PubMed]
- Lal C, White DR, Joseph JE, et al. Sleep-disordered breathing in Down syndrome. Chest 2015;147:570-9. [Crossref] [PubMed]
- Kahanowitch R, Aguilar H, Weiss M, et al. Developmental changes in obstructive sleep apnea and sleep architecture in Down syndrome. Pediatr Pulmonol 2023;58:1882-8. [Crossref] [PubMed]
- Fucà E, Costanzo F, Celestini L, et al. Sleep and behavioral problems in Down syndrome: differences between school age and adolescence. Front Psychiatry 2023;14:1193176. [Crossref] [PubMed]
- Raposo D, Menezes M, Rito J, et al. Drug-Induced Sleep Endoscopy in Pediatric Obstructive Sleep Apnea. Otolaryngol Head Neck Surg 2021;164:414-21. [Crossref] [PubMed]
- Adler AC, Musso MF, Mehta DK, et al. Pediatric Drug Induced Sleep Endoscopy: A Simple Sedation Recipe. Ann Otol Rhinol Laryngol 2020;129:428-33. [Crossref] [PubMed]
- Li Z, Celestin J, Lockey RF. Pediatric Sleep Apnea Syndrome: An Update. J Allergy Clin Immunol Pract 2016;4:852-61. [Crossref] [PubMed]
- Baldassari CM, Lam DJ, Ishman SL, et al. Expert Consensus Statement: Pediatric Drug-Induced Sleep Endoscopy. Otolaryngol Head Neck Surg 2021;165:578-91. [Crossref] [PubMed]
- Yeung GMF, Leung SY, Kwok KL. Review findings of drug-induced sleep endoscopy (DISE) in children with obstructive sleep apnea (OSA). Pediatric Respirology and Critical Care Medicine 2021;5:29-39. [Crossref]
- Manickam PV, Shott SR, Boss EF, et al. Systematic review of site of obstruction identification and non-CPAP treatment options for children with persistent pediatric obstructive sleep apnea. Laryngoscope 2016;126:491-500. [Crossref] [PubMed]
- Amos JM, Durr ML, Nardone HC, et al. Systematic Review of Drug-Induced Sleep Endoscopy Scoring Systems. Otolaryngol Head Neck Surg 2018;158:240-8. [Crossref] [PubMed]
- Mitchell RB, Archer SM, Ishman SL, et al. Clinical Practice Guideline: Tonsillectomy in Children (Update). Otolaryngol Head Neck Surg 2019;160:S1-S42. [Crossref] [PubMed]
- Esteller E, Villatoro JC, Agüero A, et al. Outcome of drug-induced sleep endoscopy-directed surgery for persistent obstructive sleep apnea after adenotonsillar surgery. Int J Pediatr Otorhinolaryngol 2019;120:118-22. [Crossref] [PubMed]
- He S, Peddireddy NS, Smith DF, et al. Outcomes of Drug-Induced Sleep Endoscopy-Directed Surgery for Pediatric Obstructive Sleep Apnea. Otolaryngol Head Neck Surg 2018;158:559-65. [Crossref] [PubMed]
- Collu MA, Esteller E, Lipari F, et al. A case-control study of Drug-Induced Sleep Endoscopy (DISE) in pediatric population: A proposal for indications. Int J Pediatr Otorhinolaryngol 2018;108:113-9. [Crossref] [PubMed]
- Wilcox LJ, Bergeron M, Reghunathan S, et al. An updated review of pediatric drug-induced sleep endoscopy. Laryngoscope Investig Otolaryngol 2017;2:423-31. [Crossref] [PubMed]
- Zalzal HG. Nasal surgery for pediatric obstructive sleep apnea. Operative Techniques in Otolaryngology-Head and Neck Surgery 2023;34:165-9. [Crossref]
- Parikh SR, Boudewyns A, Friedman NR, et al. International Pediatric Otolaryngology Group (IPOG) consensus on scoring of pediatric Drug Induced Sleep Endoscopy (DISE). Int J Pediatr Otorhinolaryngol 2023;171:111627. [Crossref] [PubMed]
- Van den Bossche K, Van de Perck E, Kazemeini E, et al. Natural sleep endoscopy in obstructive sleep apnea: A systematic review. Sleep Med Rev 2021;60:101534. [Crossref] [PubMed]
Cite this article as: Friedland Y, Blokland R, Vijayasekaran S. Drug-induced sleep endoscopy (DISE): a retrospective review in Western Australian children. Aust J Otolaryngol 2025;8:22.



